For patients with acute myocardial infarction (AMI), incomplete revascularisation may increase the risk of angina, recurrent myocardial infarction, and mortality1. Current ACC/AHA guidelines state that percutaneous coronary intervention (PCI) of non-culprit lesions may be considered (class IIb) in both STEMI and NSTEMI populations2,3. ESC STEMI guidelines state that “primary PCI should be limited to the culprit vessel with the exception of cardiogenic shock and persistent ischaemia after PCI of the supposed culprit lesion”4. Yet, three randomised clinical trials of PCI for STEMI have suggested that incomplete revascularisation is inferior to complete revascularisation for composite ischaemic endpoints5-7. These relatively small clinical trials support similar conclusions from both registry studies and meta-analyses8.
Thus, the benefit of complete revascularisation in AMI remains a subject of debate; the method (haemodynamic vs. anatomic guidance) and timing (index AMI complete revascularisation, staged PCI during first hospitalisation or staged PCI within 30 days of first angiogram) for complete revascularisation strategies remain undefined7. Furthermore, the small trial size has precluded definitive assessment of mortality benefit with various revascularisation strategies. Thus, further study is clearly warranted. In this issue of EuroIntervention, Quadri et al examine complete revascularisation versus culprit-only PCI in patients with AMI in the international BleeMACS registry9.
congratulated on addressing an area of clinical importance and unclear recommendations. Propensity score matching was utilised to address the obvious imbalances in the complete versus incomplete revascularisation groups in this registry design. Importantly, the primary endpoint focused on the unanswered question of mortality benefit: one-year mortality rates were dramatically reduced in the propensity-matched STEMI population (N=1,664) which underwent staged complete revascularisation as compared to culprit-only PCI (5.3% vs. 13.8%, p<0.01). In the smaller propensity-matched NSTEMI PCI population (N=1,218), one-year mortality was similarly reduced by over 50% with a complete revascularisation strategy (4.5% vs. 10.3%, p<0.01).
The use of a registry design to address the importance of complete revascularisation has two theoretical benefits: A) a larger denominator increases power to detect differences in strategy, especially for less frequent endpoints (i.e., mortality), and B) the ability to reflect the unselected reality of clinical practice provides insight into a broader population than those usually represented in a randomised clinical trial. The BleeMACS registry design suggests a dramatic mortality reduction with complete versus incomplete revascularisation, thus adding strength to the small randomised clinical trials that failed to show mortality differences between strategies. Does the BleeMACS international registry utilise and represent reality in a manner that drives clinicians to conclusions that go beyond those of the randomised trials?
All trials and registries have limitations, and the BleeMACS registry design is informative. First, the high proportion of STEMI patients (comprising 2/3 of the total enrolment) in this study raises concerns about the generalisability of these findings. In the CathPCI registry, PCI indications favour the usual preponderance of NSTEMI (17.9%) as opposed to STEMI (15.8%)10. Second, propensity score adjustment to account for baseline clinical differences in the comparison groups may have been inadequate11. For example, it is not clear that angiographic differences were fully matched: multiple prior registries have demonstrated important anatomic variations that impact on clinical choice of complete versus incomplete revascularisation including extent of coronary disease, left main disease, coronary flow and presence of chronic total occlusion12-14. Thirdly, the lack of core lab adjudication limits the ability to interpret both outcomes and inclusion criteria, as diagnosis of a severe angiographic stenosis in a non-culprit vessel may be variable and influenced by the clinical status of the patient.
Finally, the study of revascularisation strategies in AMI by all registry designs may be inherently inconclusive. As shown in Figure 1, the BleeMACS registry demonstrates multiple flow points where misrepresentation of the patient population and outcomes is likely to impact on the reality being analysed: for example, all hospital-related deaths are excluded from this design. If a particular revascularisation strategy is associated with increased risk of hospital death, this hazard would not be represented. Second, BleeMACS cannot see the intent of the interventional cardiologist at the time of AMI. This leads to a potential misclassification of early death with unknown intent, also known as survivor bias15. As demonstrated in Figure 1, the registry scientist must assume that all patients who died after a single PCI had incomplete revascularisation. However, if the intent was complete revascularisation in one to 30 days, these deaths falsely lower the mortality rate for a complete revascularisation-intended therapy.
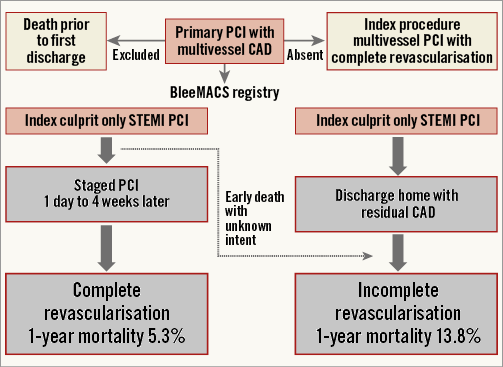
Figure 1. The study design of the BleeMACS registry with respect to the primary PCI population. Bias in survival estimates is inherent in: a) the exclusion of patients who died on the index admission, b) the exclusion of patients with single-stage complete revascularisation, and c) the survival bias by design in which intended staged complete revascularisation will be reclassified as incomplete revascularisation if death occurs after the first PCI (early death with unknown intent).
One method to overcome survival bias in a registry is to compare multivessel PCI at the time of index AMI to all other forms of incomplete or delayed revascularisation. For unclear reasons, BleeMACS has no patients who received complete revascularisation during the index procedure. A recent British Columbia Cardiac Registry study analysed three STEMI PCI revascularisation strategies - complete at index procedure, complete-staged and incomplete16. Of the three strategies, the highest crude and adjusted mortality rate was among those patients undergoing multivessel PCI at the time of the AMI. It is interesting that in British Columbia one in five STEMI PCI patients received complete revascularisation at the time of the AMI. The incomplete representation of this strategy in the BleeMACS registry further impacts on both the mortality and generalisability of this registry design.
In summary, the BleeMACS registry findings should be interpreted cautiously. The dramatic reduction in one-year mortality rates with complete revascularisation remains unproven in clinical trials. Given the registry exclusions, BleeMACS may not represent a true reality for patients with AMI and multivessel CAD. More importantly, the limitations of retrospective comparisons of complete vs. incomplete revascularisation in patients with acute myocardial infarction may inherently distort the reality of patient flow and outcomes in this challenging clinical scenario. There is no doubt that registries are critical for defining real-world practice and estimating actual outcomes. Paradoxically, the reality for revascularisation strategies may only be visible in the highly controlled world of large randomised clinical trials.
Conflict of interest statement
H. Dauerman is a consultant for Medtronic, Edwards Lifesciences and Boston Scientific, and has received research grants from Boston Scientific and Medtronic. The other author has no conflicts of interest to declare.