Multiple studies have shown that nitinol stents improve patency and relieve symptoms more effectively when treating femoral and popliteal obstructions than percutaneous transluminal angioplasty (PTA) alone. However, it is now well known that stents in the superficial femoral artery (SFA) and popliteal arteries are subject to external forces such as bending, twisting, elongation, foreshortening, and external compression1. As a consequence, in-stent restenosis (ISR) has been reported to occur in up to 40% of femoropopliteal lesions treated with metallic stents within one year2,3, with the risk of ISR increasing with lesion length. As the population with femoropopliteal stenting continues to increase, occurrence of ISR has become a clinically relevant problem.
In fact, the treatment of ISR in the femoropopliteal artery is one of the major remaining challenges of endovascular therapy. ISR is often a complex phenomenon that involves both mechanical and biological aspects: first, the presence of long stented segments in femoral arteries is a limit for positive vascular remodelling, which becomes even more true in case of localised fractures and compressions. Second, in the presence of a long stented segment, intimal hyperplasia tends to occur earlier, and dehydration resulting from PTA could accelerate vessel reocclusion.
For all these reasons many factors have to be considered when treating femoropopliteal ISR: the presence of a stenosis versus an occlusion, acute vs. chronic symptoms (suggesting acute thrombus), stent fractures, length of lesion, stent compression, type of stent, location of stent, etc. Consequently, it is very difficult to find a definite treatment able to solve all these issues. Cutting balloon angioplasty has failed to provide durable results4; laser and drug-eluting stents5,6 have shown some encouraging results but the solution is still far off.
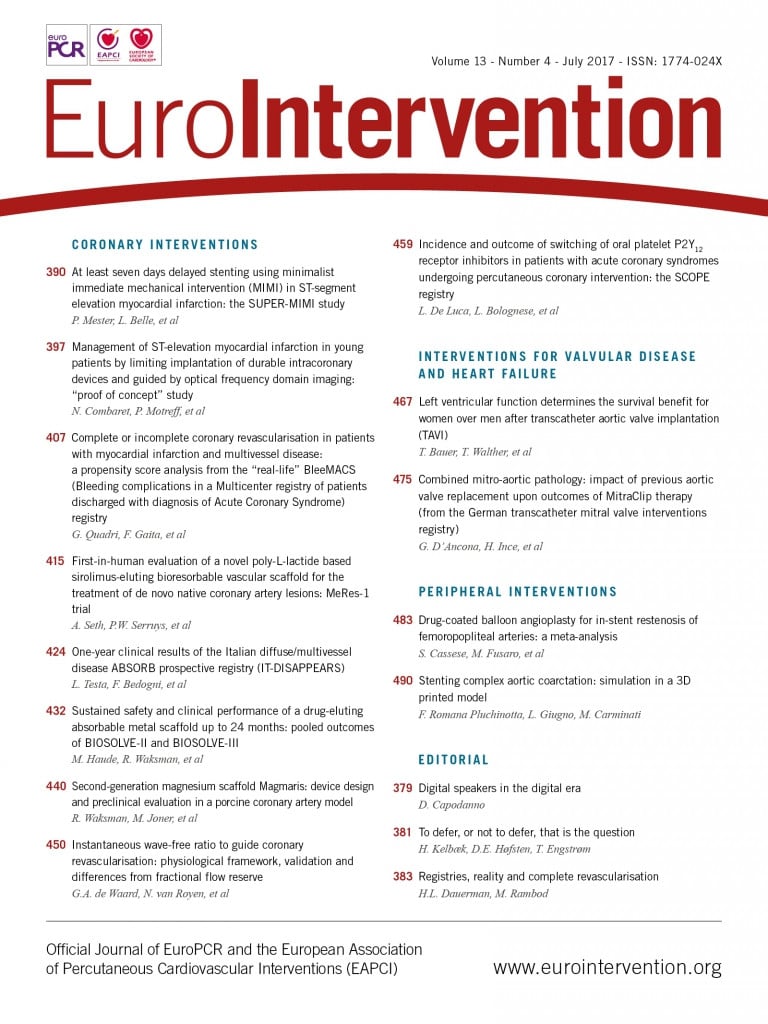
In the current issue of EuroIntervention, Cassese et al7 report a meta-analysis aimed at comparing plain balloon angioplasty and drug-coated balloon (DCB) angioplasty in treating femoropopliteal ISR. Putting together the results of small groups of patients, the authors were able to derive outcome considerations that confirm DCB efficacy in femoropopliteal ISR.
The present report adds another piece to the complex puzzle of femoropopliteal interventions: DCB have shown good midterm and long-term outcomes in both short and long femoropopliteal lesions8-11, with the potential advantage of leaving stenting for bail-out situations (i.e., flow-limiting dissections). With the current evidence, DCB should be considered the first strategy in ISR lesions. However, although putting together data is helpful to achieve statistical significance, still there is the risk of merging different scenarios. DCB are safe and effective in promoting an antiproliferative action (in both short- and longer-term follow-ups), but there are still many cases of mechanical stent disruption (e.g., stent fracture, incomplete expansion, etc.) that would hardly benefit from this type of treatment. Further prospective studies possibly enrolling femoropopliteal lesions according to the pathophysiological mechanism of ISR should be undertaken to guide interventionalists in finding a tailored, effective strategy for each clinical scenario.
Conflict of interest statement
The authors have no conflicts of interest to declare.