Abstract
Aims: Our aim was to perform a meta-analysis to investigate the outcomes of patients undergoing percutaneous revascularisation with drug-coated balloon (DCB) angioplasty because of femoropopliteal in-stent restenosis (ISR).
Methods and results: We searched scientific databases for studies of DCB angioplasty for femoropopliteal ISR. The primary outcome was target lesion revascularisation (TLR). The main secondary outcome was recurrent ISR. Other outcomes of interest were Rutherford class (RC) improvement, ankle-brachial index (ABI) and death. A total of 367 patients enrolled in four studies received DCB (n=188) or plain balloon angioplasty (n=179). Median follow-up was 12 months. Patients treated with DCB angioplasty displayed a lower risk for TLR (odds ratio [OR] 0.20, 95% confidence interval [CI]: 0.07-0.55, p=0.002) and recurrent ISR (OR 0.24, 95% CI: 0.09-0.61, p=0.003), and a sustained RC improvement (OR 2.57, 95% CI: 1.40-4.72, p=0.002) with similar ABI and mortality as compared to those patients treated with plain balloon angioplasty.
Conclusions: In comparison to plain balloon angioplasty, DCB therapy for femoropopliteal ISR is associated with superior clinical and antirestenotic efficacy. Further randomised trials comparing DCB with therapies alternative to plain balloon, in a larger number of patients, and with extended follow-up are needed to address definitively the role of DCB for femoropopliteal ISR.
Abbreviations
ABI: ankle-brachial index
DCB: drug-coated balloon
ISR: in-stent restenosis
RC: Rutherford class
TLR: target lesion revascularisation
Introduction
The percutaneous treatment of patients suffering from clinically relevant atherosclerotic disease of femoropopliteal arteries has a first-line recommendation due to the high percentage of acute success1,2. Despite the fact that the widespread use of new-generation self-expanding nitinol stents has reduced the technical shortcomings associated with plain balloon angioplasty in this vascular bed, lumen re-narrowing at the stented level continues to occur and represents a challenging clinical problem3.
Multiple endovascular technologies including balloon catheters, stents and debulking devices have been evaluated as stand-alone or combined therapies for in-stent restenosis (ISR) of femoropopliteal arteries4. Amongst others, balloon catheters coated with the Taxol derivative paclitaxel, a highly lipophilic antiproliferative drug, have attracted considerable interest5. The drug-coated balloon (DCB) has been associated with favourable angiographic and clinical efficacy in the treatment of de novo lesions of femoropopliteal arteries6. However, despite initially promising results observed in single-arm registries7,8, modestly sized investigations of DCB angioplasty for femoropopliteal ISR displayed an inconsistent clinical performance9,10. As a consequence, the clinical impact of DCB in this setting remains controversial.
Against this background, we performed a meta-analysis of studies to investigate the outcomes associated with a DCB-based revascularisation in patients with femoropopliteal ISR.
Methods
SEARCH STRATEGY AND SELECTION CRITERIA
We searched Medline, EMBASE, the Cochrane Central Register of Controlled Trials (CENTRAL), abstracts from scientific sessions and relevant websites (www.cardiosource.com, www.clinicaltrialresults.org, www.escardio.org, www.tctmd.com, www.theheart.org) without restricting language or publication status. The references listed in all eligible studies were checked to identify further citations. The final search was performed in July 2016. Search terms included the keywords and the corresponding Medical Subject Headings for: “femoropopliteal (femoral) artery”, “in-stent restenosis”, “drug-coated (-eluting) balloon”, “trial” and “randomised trial”. Inclusion criteria were: (1) percutaneous revascularisation with DCB angioplasty because of femoropopliteal ISR, and (2) a minimum of six-month follow-up. Exclusion criteria were: (1) vessels treated with DCB angioplasty other than femoropopliteal arteries; (2) per-protocol use of endovascular devices other than DCB in the experimental group, and (3) duplicated data.
DATA COLLECTION AND ASSESSMENT OF RISK OF BIAS
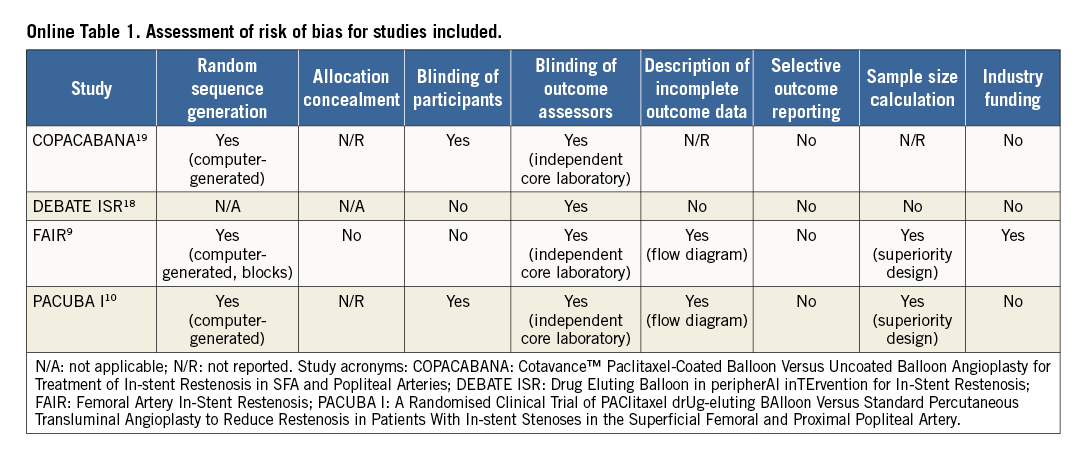
Two investigators (S. Cassese and G. Ndrepepa) independently assessed publications for eligibility at title and/or abstract level, with divergences resolved by consensus. Studies that met inclusion criteria were selected for further analysis. The same investigators independently evaluated freedom from bias for each study, in accordance with The Cochrane Collaboration method11. No formal quality score adjudication was performed12.
OUTCOME VARIABLES
The primary outcome of the current report was target lesion revascularisation (TLR). The main secondary outcome was recurrent ISR. Other outcomes of interest were Rutherford class (RC) improvement, ankle-brachial index (ABI) and death. All endpoints were evaluated according to definitions of original protocols.
STATISTICAL ANALYSIS
Odds ratio (OR) and weighted mean difference with 95% confidence interval (95% CI) were used as summary statistics. The Mantel-Haenszel random effects model (DerSimonian and Laird) was used to calculate pooled OR for categorical variables, whilst the inverse variance random effects model served to calculate pooled mean difference for continuous variables. The Breslow-Day chi2 test and the I2 statistic were used to test heterogeneity across the studies: I2 values of <25%, 25-50% or >50% indicated low, moderate or high heterogeneity, respectively11. The restricted maximum likelihood method (Tau2) took into account the occurrence of residual heterogeneity.
For the primary outcome we performed: (i) a visual estimation of funnel plot, as well as statistical tests to evaluate the possibility of publication bias13-15; (ii) an influence analysis, in which meta-analysis estimates are computed omitting one study at a time; and (iii) a trial sequential analysis, in which meta-analysis sample size calculations are combined with the threshold of statistical significance16. A sensitivity analysis evaluated the extent to which the randomised design or the funded nature of the study might have influenced the risk estimation for the primary outcome. Additionally, a random effects meta-regression analysis assessed the relation between the risk calculation for the primary outcome and relevant patients (age, proportion of males, proportion of individuals with diabetes or with a critical limb ischaemia [CLI] complaint at presentation, length of available follow-up) and lesion features (length, baseline percentage diameter stenosis, proportion of ISR class III, according to Tosaka et al3).
Statistical analysis was performed using Review Manager (RevMan), Version 5.3 (The Cochrane Collaboration, Copenhagen, Denmark), Stata 11.4 (StataCorp, College Station, TX, USA) and TSA version 0.9 Beta software packages. This study was conducted in compliance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement17.
Results
ELIGIBLE STUDIES
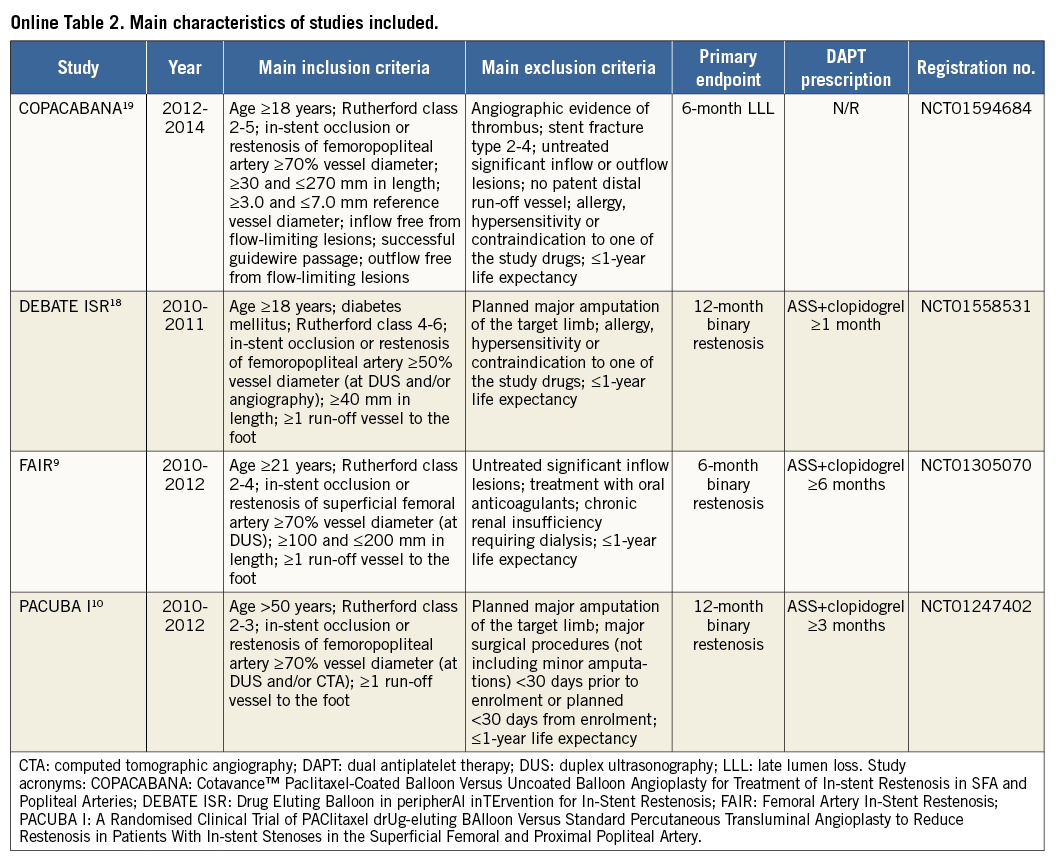
The process of study selection is summarised in Online Figure 1. A total of four studies comparing DCB versus plain balloon angioplasty were included (three as full-length manuscripts presenting the FAIR9, PACUBA I10 and DEBATE ISR18 studies, plus the COPACABANA trial19, presented at the Leipzig Interventional Course 2015).
The risk of bias among studies included is reported in Online Table 1. Finally, a total of 367 participants (188 treated with DCB and 179 with plain balloon angioplasty) were included.
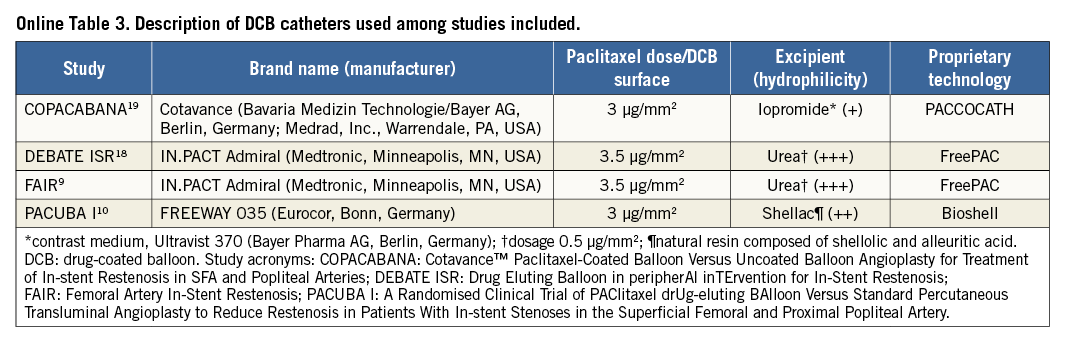
The main characteristics of the studies included are described in Online Table 2. Three out of four studies had a multicentre, randomised design (FAIR9, PACUBA I10 and COPACABANA19). In the remaining study (DEBATE ISR18), consecutive diabetic patients presenting with ISR of femoropopliteal arteries treated with DCB angioplasty were compared with an historical cohort of consecutive diabetic patients receiving plain balloon angioplasty because of femoropopliteal ISR. The main inclusion criterion in the original studies was the evidence of ISR of the femoropopliteal artery (≥50% in diameter and ≥30 mm in length), with at least one run-off vessel to the foot and symptoms ranging from claudication to ischaemic ulcerations. The main exclusion criterion was known or suspected allergy/intolerance to contrast medium, paclitaxel or dual antiplatelet therapy (DAPT). The balloon catheters used were coated with paclitaxel (at a dose of 3 μg/mm210,20 or 3.5 μg/mm29,18 of balloon surface) or uncoated. The antiproliferative drug was delivered directly from the balloon surface to the vessel wall with a vehicle consisting of an organic (urea9,18 or shellac10) or inorganic (contrast medium20) excipient. Device descriptions are summarised in Online Table 3. In all studies, bail-out stenting after angioplasty was allowed in case of a suboptimal result after dilation in both treatment groups.
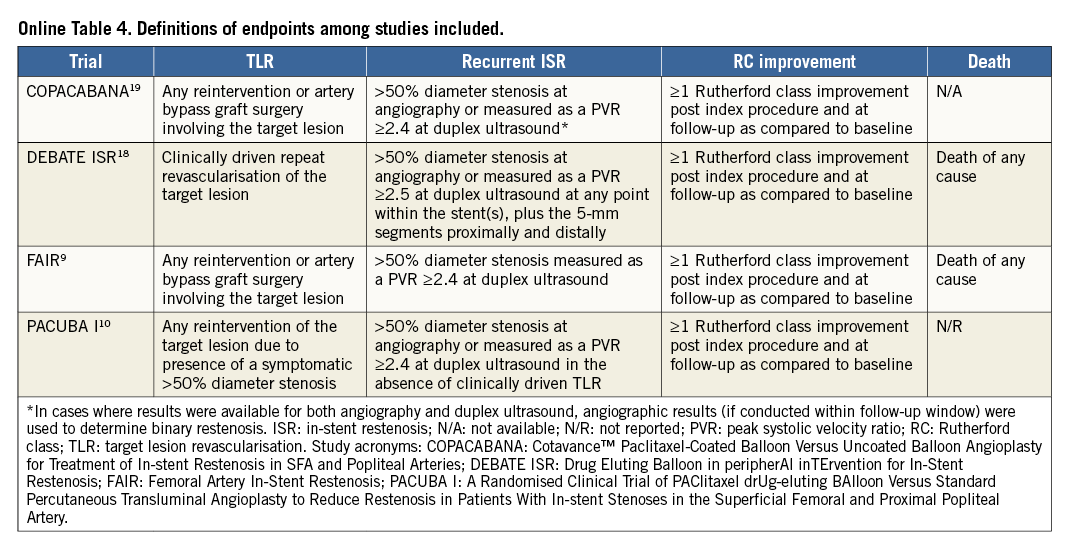
An overview of the main clinical endpoint definitions among studies included is reported in Online Table 4. In three out of four studies the primary endpoint consisted of the incidence of recurrent ISR at six- or 12-month follow-up9,10,18. In the remaining study the primary endpoint was late lumen loss after six months20. For one study, three-year follow-up data were available18. However, the current analysis relies on aggregate data up to 12 months in order to provide a homogenous follow-up among studies included.
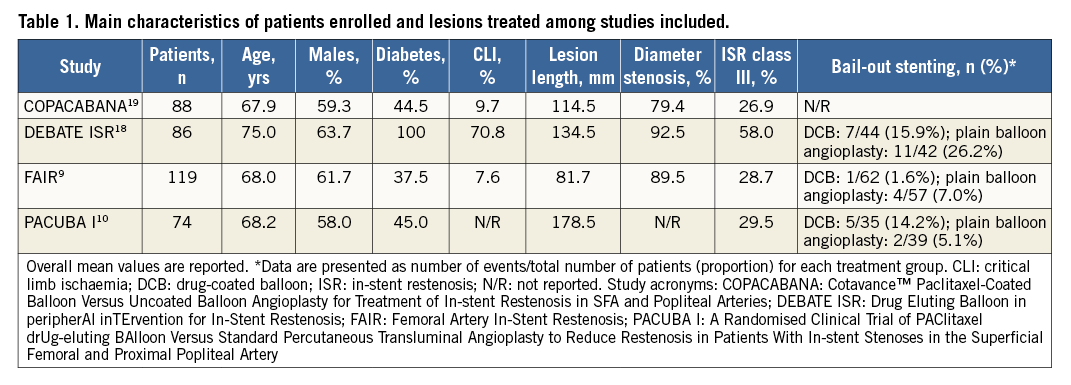
The clinical characteristics of participants included in the original studies are reported in Table 1. Patients had a median age of 68.1 years (67.9-71.6), were predominantly male, with a high frequency of diabetes mellitus, and nearly 10% of cases involved a CLI complaint. Overall, lesions treated were intermediate in length (124.0 mm [98.1-156.5]) and the diameter stenosis was 89.5% (79.4-92.5). Patients treated with DCB angioplasty had a lesion length of 125.9 mm (101.1-152.5) and a diameter stenosis of 89.0% (77.7-91.3). Patients treated with plain balloon angioplasty had a lesion length of 123.2 mm (95.2-160.5) and a diameter stenosis of 89.9% (81.2-93.8). Roughly one third of lesions treated presented as complete occlusion (ISR class III) at baseline angiography. The median percentage of bail-out stenting was 9.1% among patients treated with DCB angioplasty and 7.0% among those treated with plain balloon angioplasty. Standard medical therapy was prescribed to all patients irrespective of the treatment received. The duration of DAPT after revascularisation ranged between one and six months, with a median DAPT duration of three months (1-6).
CLINICAL OUTCOMES
Of those included, 318 patients (86.6%) were available for assessment of outcomes of interest. Median follow-up was 12 months (9-12).
TLR, the primary outcome of the present report, occurred in 92 patients (28.9%) (Figure 1). The risk of TLR was significantly reduced in patients treated with DCB versus plain balloon angioplasty (14.9% versus 44.3%; OR 0.20, 95% CI: 0.07-0.55, p=0.002). There was a high heterogeneity for this risk estimate (I2=68%, p for heterogeneity [phet]=0.03).
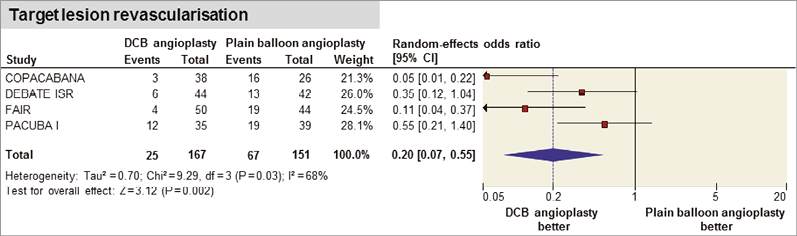
Figure 1. Risk estimate for target lesion revascularisation with DCB versus plain balloon angioplasty. Plots of odds ratio for target lesion revascularisation associated with DCB versus plain balloon angioplasty. The diamond indicates the point estimate and the left and the right ends of the line the 95% confidence interval (CI). DCB: drug-coated balloon. Study acronyms are explained in Table 1.
Recurrent ISR occurred in 118 patients (49.5%, data available for 238 patients [74.8%] enrolled in three studies9,10,18) (Figure 2). The risk of recurrent ISR was significantly reduced in patients treated with DCB versus plain balloon angioplasty (32.5% versus 66.9%; OR 0.24, 95% CI: 0.09-0.61], p=0.003). There was a high heterogeneity for this risk estimate (I2=65%, phet=0.03).
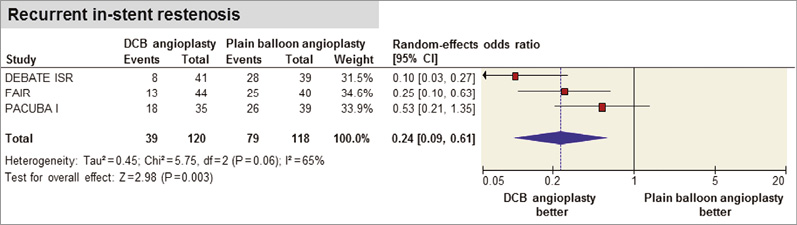
Figure 2. Risk estimate for recurrent in-stent restenosis with DCB versus plain balloon angioplasty. Plots of odds ratio for recurrent in-stent restenosis associated with DCB versus plain balloon angioplasty. The diamond indicates the point estimate and the left and the right ends of the line the 95% confidence interval (CI). DCB: drug-coated balloon. Study acronyms are explained in Table 1.
RC improvement was reported in 134 patients (66.3%, data available for 202 patients [63.5%] enrolled in three studies: FAIR9, PACUBA I10 and DEBATE ISR18) (Online Figure 2A). Patients treated with DCB angioplasty displayed a sustained RC improvement as compared to those treated with plain balloon angioplasty (76.3% versus 55.6%; OR 2.57, 95% CI: 1.40-4.72, p=0.002; I2=0%, phet=0.80).
ABI was obtained in 206 patients enrolled in three studies: FAIR9, PACUBA I10 and COPACABANA19 (64.7%) (Online Figure 2B). No significant difference in terms of ABI was found after DCB in comparison to plain balloon angioplasty (range in mm 0.79 to 0.3 versus 0.84 to 1.60; –0.28 [-0.59, 0.03]; p=0.08). There was a high heterogeneity for this risk estimate (I2=90%, phet<0.0001).
Death occurred in 11 patients (6.2%; data available for 177 patients [55.6%] enrolled in two studies: FAIR9 and DEBATE ISR18) (Online Figure 2C). No significant difference in terms of risk for death was found in patients treated with DCB in comparison to plain balloon angioplasty (5.5% versus 6.9%; OR 0.78, 95% CI: 0.23-2.67, p=0.69; I2=0%, phet=0.72).
SMALL STUDY EFFECTS, INFLUENCE AND SENSITIVITY ANALYSES
Funnel plot distribution of the primary outcome was derived from the standard error of the logarithm OR plotted against the OR for TLR (Online Figure 3A). In addition to visual estimation of the funnel plot, statistical tests excluded a publication bias for the primary outcome.
According to the influence analysis, no single study significantly altered the summary OR for TLR, though the heterogeneity remained high (Online Figure 3B). However, when the analysis for the primary outcome was restricted to those studies evaluating the identical DCB platform9,18, the risk estimate for TLR favoured the investigational device without high heterogeneity (OR 0.21, 95% CI: 0.07-0.62, p=0.005; I2=47%, phet=0.17). The trial sequential analysis revealed that the sample size accumulated provided robust evidence for TLR (Online Figure 4).
There was no modification of the risk estimate for TLR according to the randomised design (p for interaction, [pint]=0.39) or the funded nature of the studies (pint=0.40). Moreover, the risk estimation for TLR had no statistical relation with the age of participants (p=0.60), the proportion of males (p=0.99), the proportion of patients with diabetes (p=0.60), or CLI complaint (p=0.26), lesion length (p=0.20), the baseline percentage of diameter stenosis (p=0.26), the proportion of ISR class III at baseline angiography (p=0.57) or the length of available follow-up (p=0.22) (Online Table 5).
Discussion
This meta-analysis investigated the performance of DCB in patients suffering from ISR of femoropopliteal arteries. In all studies the control group consisted of patients treated with plain balloon angioplasty. The main findings are that: (i) DCB has superior efficacy in comparison to plain balloon angioplasty at one-year follow-up, irrespective of the baseline clinical and angiographic complexity; (ii) the available evidence is sufficient to confirm the superiority of DCB as compared to plain balloon angioplasty in this setting.
Multiple treatment options such as balloon angioplasty, repeat stenting and debulking have been investigated in patients with femoropopliteal ISR4. However, as there is no single therapy which is particularly effective or superior to any other, there is no established best treatment strategy for these cases.
Comparisons of DCB versus plain balloon angioplasty for femoropopliteal ISR included a limited number of patients and displayed inconsistent results20. For this reason, we conducted this meta-analysis to study the performance of DCB angioplasty in patients presenting with ISR of femoropopliteal arteries. This report highlights a number of important issues.
REDUCED RISK FOR TLR AFTER DCB ANGIOPLASTY
In the present analysis, DCB versus plain balloon angioplasty for femoropopliteal ISR showed a significantly lower risk for TLR at one-year follow-up. There was no significant relation between this risk estimate and the clinical and angiographic complexity at baseline. Interestingly, each of the individual studies included in this report contained only sufficient power for surrogate outcomes, thus supporting the necessity of a meta-analysis to investigate the clinical impact of DCB angioplasty in this scenario. By pooling >300 patients with femoropopliteal ISR, this study lends support to the lower risk for TLR of DCB versus plain balloon angioplasty, since the available sample size accounts for >90% of that required to address a measurable effect of DCB for this endpoint. In this respect, the objective of future studies of DCB therapy in patients with femoropopliteal ISR remains twofold: first, to disclose whether the performance of DCB should be regarded as a “class effect”; second, to assess the relative efficacy of DCB angioplasty versus revascularisation strategies other than plain balloon angioplasty. Indeed, we cannot fully ascertain whether the high heterogeneity observed in the risk calculations for main outcomes is due to different antirestenotic potency among DCB catheters studied; however, here we provide robust evidence against the use of plain balloon angioplasty as a comparative therapy in studies of femoropopliteal ISR.
REDUCED RISK FOR RECURRENT ISR AFTER DCB ANGIOPLASTY
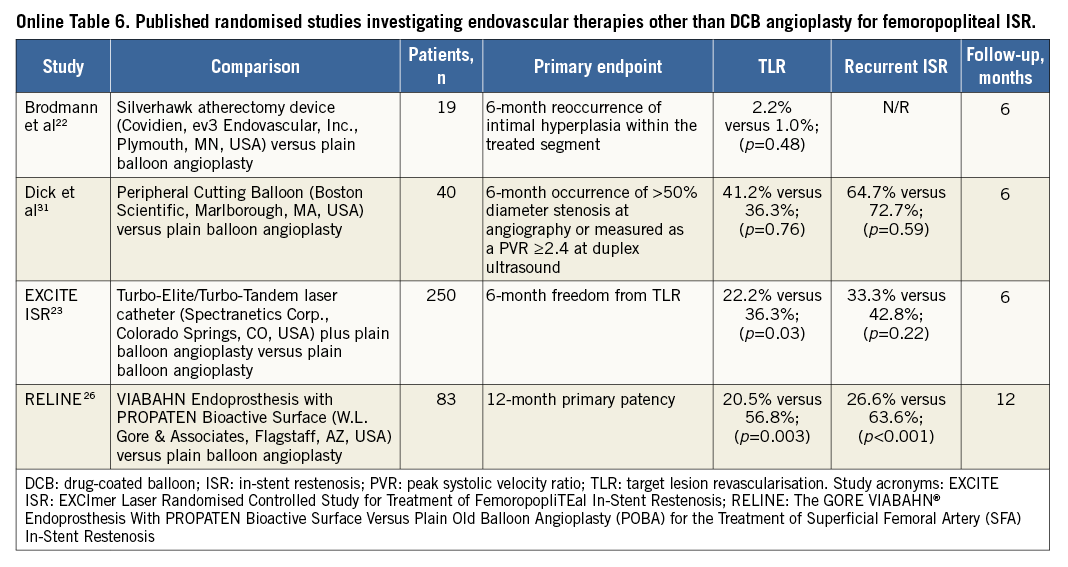
In this analysis, we observed a reduced risk for recurrent ISR at one-year follow-up with DCB versus plain balloon angioplasty for femoropopliteal ISR. The favourable outcome associated with DCB is probably due to inhibition of neointimal hyperplasia, a common finding of restenotic lesions of stented segments21. The complex interplay between biomechanical forces, shear stress of the vessel wall and proliferation of neointima observed in the femoropopliteal arteries constrained from a permanent scaffold are regarded as responsible for the pathophysiological process which leads to restenosis22. Thus, in this setting, DCB-based therapies should be preferred over other available strategies, such as plaque removal devices and stents (Online Table 6). Regarding the first of these, the use of debulking devices as a stand-alone therapy has been associated with inconsistent midterm results23-25. Regarding the second, drug-coated26 or covered stents27 showed acceptable patency up to one-year follow-up, though the shrinkage of the vessel lumen by multiple stent layers (the so-called “onion skin” phenomenon) may potentially impair the vascular compliance and increase the risk of recurrent ISR20,28.
FEMOROPOPLITEAL ISR IS A LONG-LASTING PROCESS
In the current study, patients treated with DCB angioplasty because of femoropopliteal ISR reported a sustained improvement of clinical status at one-year follow-up as compared to those patients treated with plain balloon angioplasty. However, a follow-up longer than one year remains important to rule out definitively a time-dependent efficacy of DCB in this particular setting. In fact, Schmidt and co-workers have recently demonstrated a drop-off of vessel patency two years after DCB therapy for femoropopliteal ISR8. Consistent with this, Grotti and co-workers found that, three years after the index procedure, DCB and plain balloon angioplasty led to a similar risk of reintervention of the affected limb29. In contrast with the coronary vasculature, preclinical models of restenosis after peripheral artery stenting have demonstrated that metallic implants permanently overstretch the arterial wall and provoke a persistent neointimal growth, which may be responsible for the exaggerated “catch-up” phenomenon observed after DCB therapy because of femoropopliteal ISR30. According to results of preliminary investigations, the synergy of different endovascular technologies for femoropopliteal ISR holds promise31, though a more proper evaluation requires further studies with a successful retention of patients enrolled throughout the study period.
Study limitations
The current study presents a number of limitations. First, this meta-analysis was based on aggregate data from both randomised and observational studies. However, there was no interaction between study design and primary outcome. Second, the assessment of publication bias was based on a small number of trials, a fact that limits a definitive conclusion regarding the existence of potential bias due to small study effects. Third, the risk estimation for death relies on aggregate data from two out of four studies, a fact which limits a definitive conclusion regarding this outcome. Fourth, we observed a considerable drop-out of patients during follow-up among the original studies, a fact which may somewhat limit the conclusiveness of this report. Fifth, DAPT duration varied among studies included in this report, and the possible effect of a prolonged or more potent platelet inhibition cannot be defined in this context. Finally, although the potential need for multiple DCB catheters to treat long lesions should be acknowledged, we did not perform a cost-effectiveness analysis evaluating the economic impact of DCB as compared to plain balloon angioplasty for treating femoropopliteal ISR.
Conclusions
The results of our meta-analysis suggest that, in patients presenting with ISR of femoropopliteal arteries, a percutaneous intervention with DCB as compared to plain balloon angioplasty offers superior clinical and antirestenotic efficacy at one-year follow-up. These findings should be interpreted with caution in view of the limited number and the different design of the included studies. Future randomised trials should compare DCB with therapies other than plain balloon angioplasty in a larger number of patients with follow-up longer than one year, in order to address definitively the role of DCB in this complex patient population.
| Impact on daily practice In patients with atherosclerotic disease of femoropopliteal arteries, new-generation stents reduced the mechanical shortcomings associated with plain balloon angioplasty. Notwithstanding this, lumen re-narrowing at the stented level still represents a challenging clinical problem. This analysis found that, at one-year follow-up, drug-coated balloons are associated with superior efficacy as compared to plain balloon angioplasty in patients with restenosis after femoropopliteal stenting. The evidence provided in this report is sufficient to discourage the use of plain balloon angioplasty as comparative therapy in future studies of restenosis after stenting of femoropopliteal arteries. |
Conflict of interest statement
A. Kastrati reports patent applications related to drug-eluting stent technologies. R. Byrne reports receiving lecture fees from B. Braun Melsungen AG, Biotronik and Boston Scientific and scientific support from Boston Scientific and HeartFlow. D. Giacoppo is the recipient of a research fellowship grant funded by the European Association of Percutaneous Cardiovascular Interventions (EAPCI). The other authors have no conflicts of interest to declare.
Supplementary data
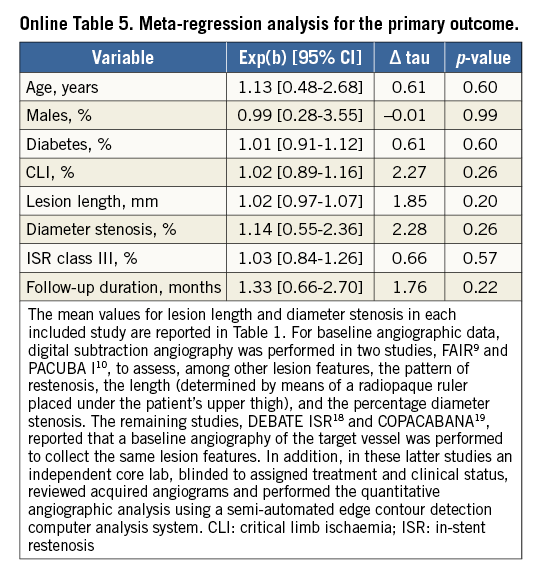
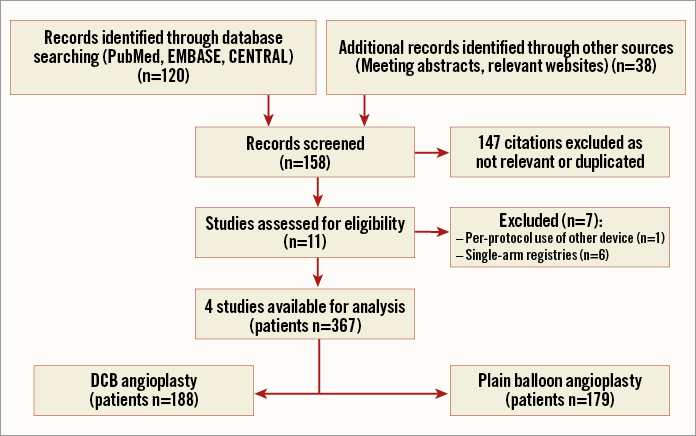
Online Figure 1. Flow diagram of study selection process. Flow chart for the study selection process according to Preferred Reporting Items for Systematic reviews and Meta-Analyses. DCB: drug-coated balloon
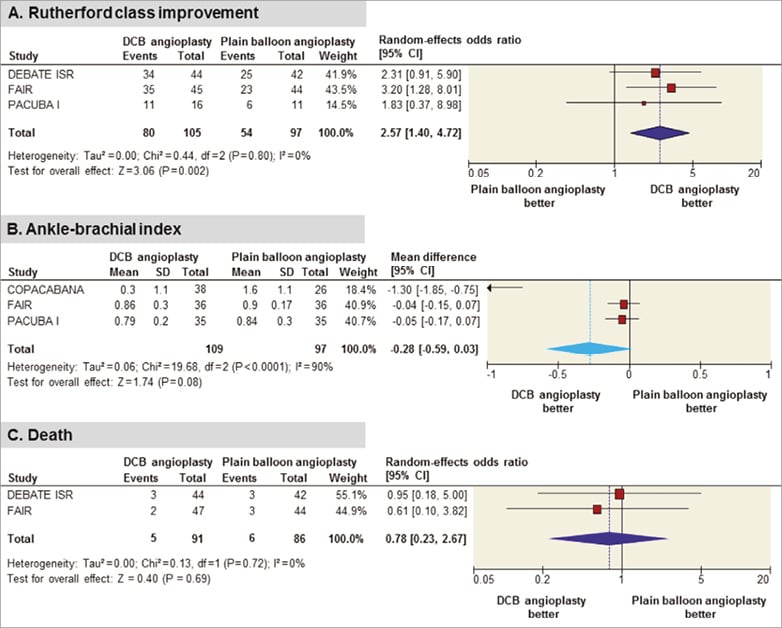
Online Figure 2. Risk estimates for other secondary outcomes of DCB versus plain balloon angioplasty. Plots of odds ratio for A) Rutherford class improvement, B) ankle-brachial index, and C) death associated with DCB versus plain balloon angioplasty. The diamond indicates the point estimate and the left and the right ends of the line the 95% confidence interval (CI). DCB: drug-coated balloon. Study acronyms: COPACABANA: Cotavance Paclitaxel-Coated Balloon Versus Uncoated Balloon Angioplasty for Treatment of In-stent Restenosis in SFA and Popliteal Arteries; DEBATE ISR: Drug Eluting Balloon in peripherAl inTErvention for In-Stent Restenosis; FAIR: Femoral Artery In-Stent Restenosis; PACUBA I: A Randomised Clinical Trial of PAClitaxel drUg-eluting BAlloon Versus Standard Percutaneous Transluminal Angioplasty to Reduce Restenosis in Patients With In-stent Stenoses in the Superficial Femoral and Proximal Popliteal Artery.
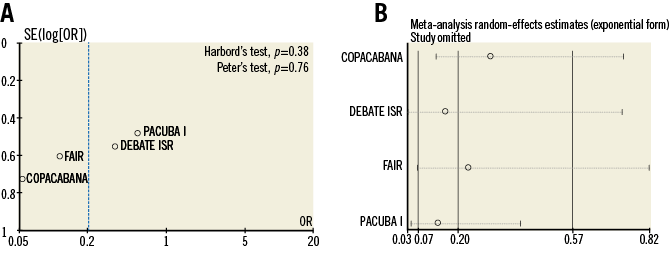
Online Figure 3. Funnel plot and influence analysis according to primary outcome. A) Funnel plot distribution of trials according to primary outcome. The standard error (SE) of the logarithm of odds ratio – log(OR) – is plotted against the OR of target lesion revascularisation. B) Influence analysis according to primary outcome. Meta-analysis random-effects estimates for target lesion revascularisation are computed omitting one study at a time. Study acronyms: COPACABANA: Cotavance Paclitaxel-Coated Balloon Versus Uncoated Balloon Angioplasty for Treatment of In-stent Restenosis in SFA and Popliteal Arteries; DEBATE ISR: Drug Eluting Balloon in peripherAl inTErvention for In-Stent Restenosis; FAIR: Femoral Artery In-Stent Restenosis; PACUBA I: A Randomised Clinical Trial of PAClitaxel drUg-eluting BAlloon Versus Standard Percutaneous Transluminal Angioplasty to Reduce Restenosis in Patients With In-stent Stenoses in the Superficial Femoral and Proximal Popliteal Artery.
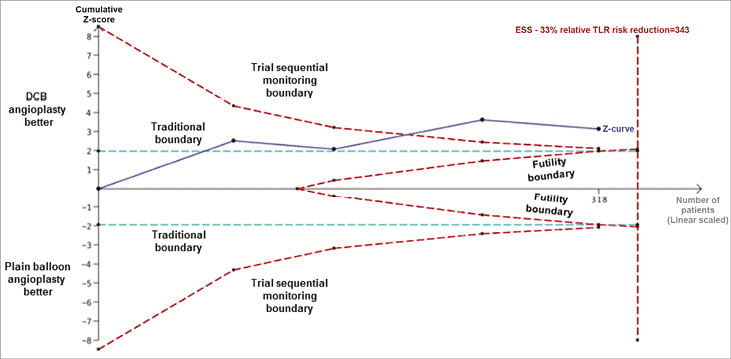
Online Figure 4. Trial sequential analysis for the primary outcome. Heterogeneity adjusted estimated sample size (ESS) of 343 participants calculated on the basis of odds ratio of target lesion revascularisation (TLR) of 44.3% in the control group, relative risk (RR) reduction=33%, alpha=5%, beta=20%, I2=0%. Dashed blue cumulative Z-curve crossed the light green dashed traditional boundary, the dashed red information size boundary and the dashed red futility boundary, thereby suggesting firm evidence for the DCB angioplasty group as compared to the plain balloon angioplasty group with respect to this outcome. Horizontal dashed light green lines illustrate traditional level of statistical significance (p=0.05).