Abstract
Aims: The use of multiple geographical sites for randomised cardiovascular trials may lead to important heterogeneity in treatment effects. This study aimed to determine whether treatment effects from different geographical recruitment regions impacted significantly on five-year MACCE rates in the SYNTAX trial.
Methods and results: Five-year SYNTAX results (n=1,800) were analysed for geographical variability by site and country for the effect of treatment (CABG vs. PCI) on MACCE rates. Fixed, random, and linear mixed models were used to test clinical covariate effects, such as diabetes, lesion characteristics, and procedural factors. Comparing five-year MACCE rates, the pooled odds ratio (OR) between study sites was 0.58 (95% CI: 0.47-0.71), and countries 0.59 (95% CI: 0.45-0.73). By homogeneity testing, no individual site (X2=93.8, p=0.051) or country differences (X2=25.7, p=0.080) were observed. For random effects models, the intraclass correlation was minimal (ICC site=5.1%, ICC country=1.5%, p<0.001), indicating minimal geographical heterogeneity, with a hazard ratio of 0.70 (95% CI: 0.59-0.83). Baseline risk (smoking, diabetes, PAD) did not influence regional five-year MACCE outcomes (ICC 1.3%-5.2%), nor did revascularisation of the left main vs. three-vessel disease (p=0.241), across site or country subgroups. For CABG patients, the number of arterial (p=0.49) or venous (p=0.38) conduits used also made no difference.
Conclusions: Geographic variability has no significant treatment effect on MACCE rates at five years. These findings highlight the generalisability of the five-year outcomes of the SYNTAX study.
Abbreviations
CABG: coronary artery bypass graft
CI: confidence interval
ICC: intraclass correlation
IQR: interquartile range
LM: left main
MACCE: major adverse cardiac and cerebrovascular events
OR: odds ratio
PAD: peripheral arterial disease
PCI: percutaneous coronary intervention
PLATO: a Study of PLATelet Inhibition and Patient Outcomes
RCT: randomised controlled trial
SD: standard deviation
SYNTAX: SYNergy Between PCI With TAXUS and Cardiac Surgery
TVR: target vessel revascularisation
3VD: three-vessel disease
Introduction
Randomised clinical trials (RCTs) that compare treatment effects between groups often enrol patients from multiple centres and geographical sites, to obtain appropriately powered sample sizes and to ensure the applicability of study findings within a suitable timeframe. For RCTs that shape revascularisation guidelines, heterogeneity of treatment effects in coronary artery bypass graft (CABG) vs. percutaneous coronary intervention (PCI) outcomes trials may be driven by differences in baseline patient risk, regional practice differences (arterial conduit use for CABG1 , stent strategies) or adherence to optimal medical therapy2, despite stringent study protocols and attempts to standardise these.
The SYNTAX (SYNergy Between PCI with TAXUS and Cardiac Surgery) trial was a multicentre, randomised controlled trial that compared revascularisation with PCI using paclitaxel-eluting stents to CABG for patients with complex coronary artery disease3. Data from 85 study sites and 18 regions were pooled, representing a range of sample sizes, treatment approaches, and patient morbidities. Whether these differences in the SYNTAX study caused significant interaction between site, region, and treatment effect remains unknown.
Thus, the aim of this study was to examine whether geographical variability (by site or region) had any impact upon treatment effects for the five-year major adverse cardiac and cerebrovascular events (MACCE) rates from the SYNTAX study, and whether this was a potentially important interaction that may affect the robustness or generalisability of this or future trial results.
Methods
The study protocol for the SYNTAX trial has been published previously3-5. In brief, patients with three-vessel disease (3VD) or left main coronary disease were allocated to the randomised revascularisation arms of PCI or CABG, or the individual PCI/CABG registries if patients were ineligible for either treatment. Sites had a minimum of 16 and a maximum of 56 randomised patients, for a total of 1,800 patients (CABG n=897; PCI n=903) comprising the study population3,5. The primary endpoint was non-inferiority of one-year MACCE, with secondary endpoints including MACCE rates at three and five years5.
CLINICAL ENDPOINT DEFINITIONS
MACCE were defined as a composite of all-cause mortality, stroke, myocardial infarction, and repeat revascularisation, with the five-year period for follow-up considered as 1,855 days5.
STATISTICAL ANALYSIS
Initially, five-year MACCE incidence and odds ratios were calculated for individual sites, as well as individual countries, where all sites were pooled together per country. This was supplemented with survival analysis, analysing the effect of study arm on time-to-MACCE, with censoring at the five-year timepoint. The difference in interventions in time to a composite safety endpoint of cerebrovascular accident (CVA) or MI or death was also analysed, as was the time to repeat revascularisation procedure.
The presence of geographical heterogeneity in the effect of revascularisation treatment (CABG versus PCI) on the five-year incidence of MACCE was quantified in a stepwise fashion. In the first instance, fixed-effect methods were used to explore heterogeneity over sites and over countries using the Breslow-Day chi-square test for OR homogeneity. Secondly, shared frailty Cox models were created using either geographical sites or countries as random clusters. From this cluster variance, an intraclass correlation coefficient was calculated to quantify the percentage of the variance in the time-to-event attributable to geographical centre. These models were also adjusted for differences in baseline patient risk (including age and gender), clinical covariates such as diabetes, smoking rates, lesion complexities, and PCI and CABG procedural variations, in order to examine the effect on the cluster variability. Although hypothesis tests were not of primary interest in this report, p<0.05 was defined as the threshold for significance for the heterogeneity tests. Statistical analyses were performed using SAS, Version 9 (SAS Institute Inc., Cary, NC, USA), and SPSS, Version 16 (SPSS Inc., Chicago, IL, USA).
Results
A total of 556 patients experienced MACCE at five years (36.9% of PCI vs. 31.0% of CABG patients, p=0.12) with mean (SD) time to MACCE of 604.5±585.1 days. Of this group, 328 (59.0%) experienced the composite safety endpoint (myocardial infarction, stroke or death) and 329 (59.2%) underwent repeat revascularisation.
STUDY SITE OR GEOGRAPHICAL REGION (USA, EASTERN OR WESTERN EUROPE) VARIABILITY AND EFFECT ON MACCE RATE
The calculated OR for five-year MACCE are shown by country (Figure 1, Table 1).
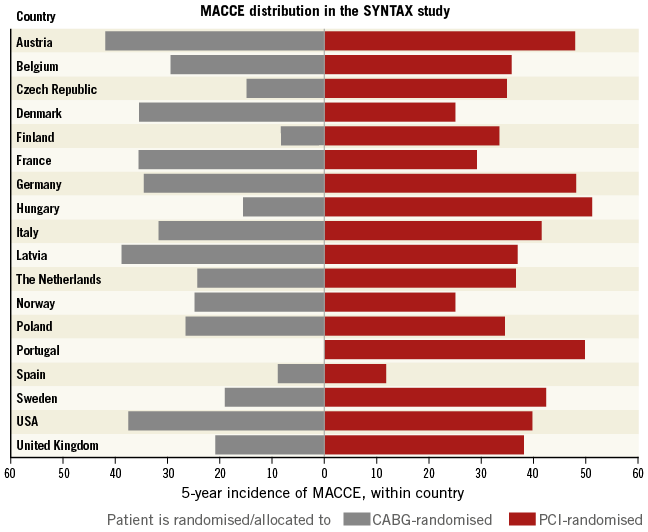
Figure 1. Observed odds ratios by country for risk of five-year MACCE occurrence for individuals in the SYNTAX study.
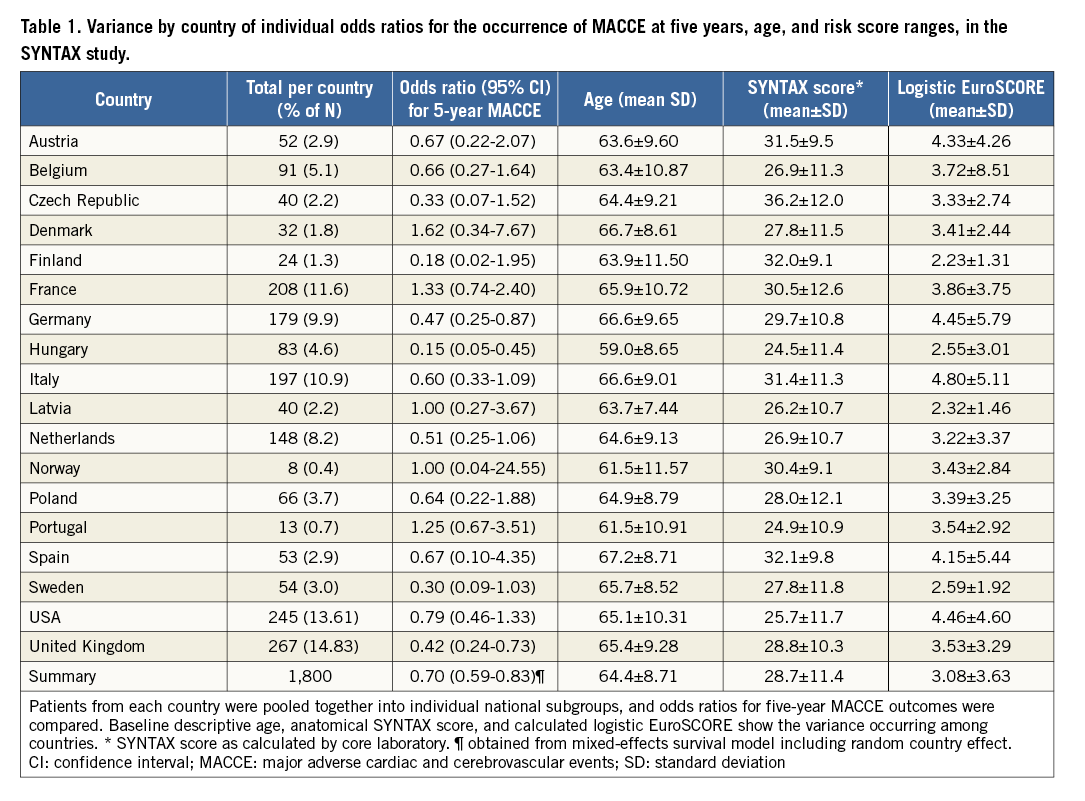
Recruitment numbers ranged from one patient at two sites, to 50 patients for the largest site, with an overall median (IQR) study recruitment of 19 (11.32) per centre. Between study sites, significant MACCE rate variability was not observed (Breslow-Day X2=93.8, p=0.051), supported by survival models showing only a small intraclass correlation of 5.1% (p=0.025). Similarly, the overall OR for five-year MACCE rates was almost identical between individual sites (0.58, 95% CI: 0.47-0.71), and between countries (0.59, 95% CI: 0.45-0.73). No significant heterogeneity was observed between individual countries, indicating that the geographical location for revascularisation did not substantially alter the risk of MACCE occurrence (ICC 0.6%, p<0.001, Breslow-Day X2=25.7, p=0.080; ICC=1.5%, p=0.071).
Sites were then classified into broad geopolitical regions: USA versus Western Europe (UK, France, Austria, Belgium, Denmark, Finland, Germany, Italy, the Netherlands, Norway, Portugal, Spain and Sweden) versus Eastern Europe (Czech Republic, Hungary, Latvia, Poland), and examined in a survival model. There was no significant difference between regions in the hazard ratio (p=0.154); however, we observed qualitative differences with the smallest regional intervention effect in the USA (HR 0.93, 95% CI: 0.61-1.43), followed by Western Europe (HR 0.70, 95% CI: 0.57-0.85), and the largest effect in Eastern Europe (HR 0.49, 95% CI: 0.30-0.80), with an ICC of 5.1%.
PATIENT-SPECIFIC FACTORS
AGE AND GENDER
The mean (IQR) percentage of males was 75.8% (71, 85%) for individual sites, and 79.2% (79, 83%) for individual countries (p=0.18). Similarly, the mean (IQR) age for individual sites was 65.2 (64, 67) years, and 64.4 (64, 66) for individual countries (p=0.49). Male gender and age did not influence five-year MACCE in the adjusted models (HR 1.43: 95% CI: 1.21-1.69, p<0.001) (ICC=5.1% male gender, ICC=5.6% age, p<0.025).
BASELINE PATIENT RISKS AND COMORBIDITIES
Rates of baseline patient risk factors (smoking, carotid artery disease, diabetes and hypertension) demonstrated a wide variability across geographical locations, as seen in Table 2. Conversely, minimal variability was observed between site and country for lesion complexity and preoperative risk scores. There were no baseline risk factors that influenced overall hazard ratios for five-year MACCE rates (ICC range 1.0-1.3% where p<0.001, HR range 0.58-0.59, 95% CI: 0.47-0.72), as seen in the survival models.
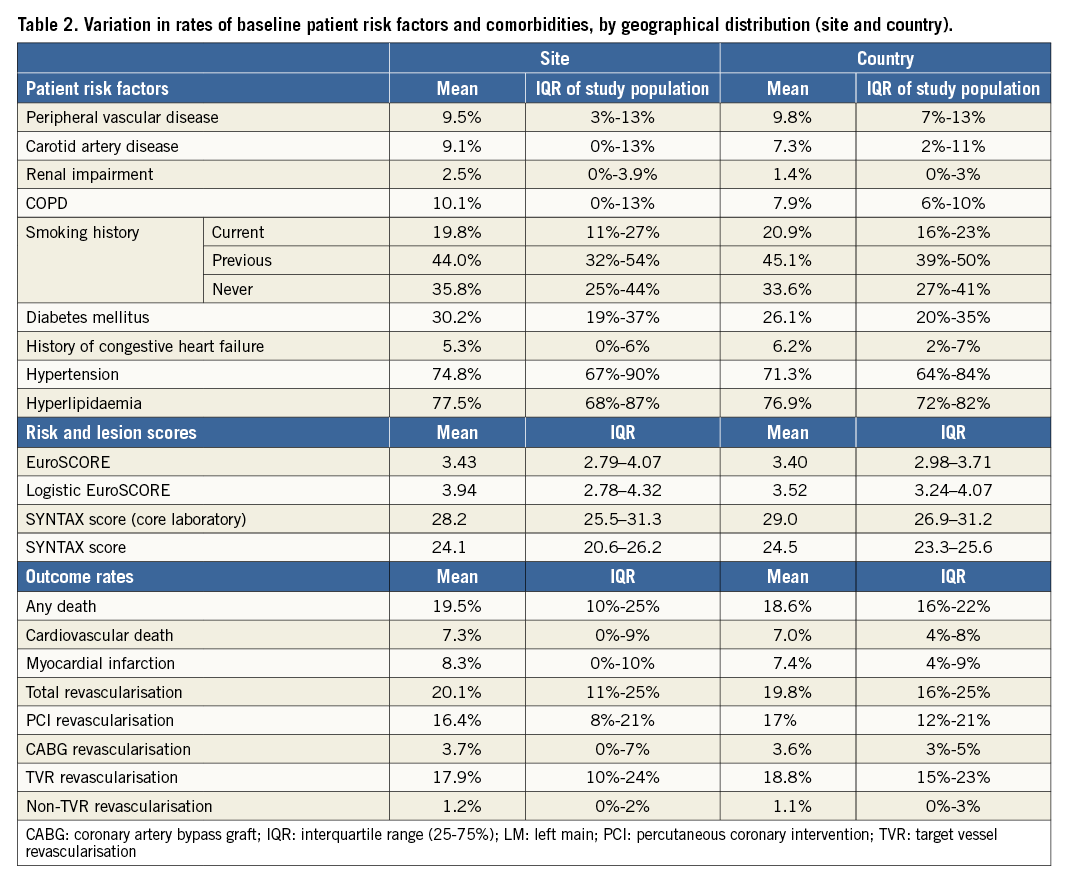
PROCEDURAL TECHNICAL PARAMETERS
The mean (range; IQR) number of patients with implanted stent length >100 mm was similar at 30.2% (0-100%; 13%, 43%) by individual site, and 33.9% (8-59%; 23%, 46%) by country. For the CABG group, a total of 66.0% had one arterial conduit, and 25.2% had two arterial conduits. Single venous conduits were used for 35.8%, and two venous conduits in 33.5%. Similarly to those seen with the SYNTAX scores, multivariate regression models adjusted for lesion characteristics did not show significant variability (ICC 1.1-1.6%, p<0.001).
REVASCULARISATION, SAFETY AND LEFT MAIN/THREE-VESSEL DISEASE
For the overall PCI group, 52.3% (572) had complete revascularisation vs. 47.7% (521) with incomplete revascularisation (p=0.39). The minimum and maximum country-level PCI percentages were 46% and 54%, respectively, with variability in outcomes persisting across sites. Comparing PCI to CABG, the adjusted hazard ratio for revascularisation was 2.03 (95% CI: 1.61-2.55).
For left main patients, overall revascularisation rates were 26.7% (90) for PCI vs. 15.5% (49) for CABG. Cox regression showed HR 1.82 (95% CI: 1.28-2.57 and p<0.001), which increased to 1.89 (95% CI: 1.33-2.68) when in the adjusted mixed-effects survival model. By geographic subgroup, a wide range of left main (LM) disease and revascularisation rates was observed, with the revascularisation rates being driven by PCI and TVR rates, as expected.
REVASCULARISATION BY CABG
For patients treated by CABG, the percentage of complete versus incomplete surgical revascularisation was 68.7% vs. 31.3%, respectively. Linear models (one vs. two vs. three or more conduits) showed no heterogeneity by site for the number of arterial (p=0.49) or venous (p=0.38) conduits, or by country for the number of arterial (p=0.43) or venous (p=0.46) conduits.
COMPOSITE SAFETY ENDPOINT
The five-year rate of a composite of CVA, MI or mortality was 17.8% in the CABG group and 21.2% in the PCI group. Adjusted for clustering, the composite safety HR was 1.21 (95% CI: 0.98-1.51), and the ICC was 3.6% by site, or 4.7% by country, indicating only a small clustering effect.
Discussion
This analysis of SYNTAX trial five-year outcomes shows that no significant heterogeneity of treatment effects was observed, taking into account both geographic and demographic differences. Degrees of variability in outcomes across sites were evident, as expected, even when site and country pooling occurred, in particular for PCI, TVR, and the type of conduits used for CABG. These findings reflect similar results from the recent CABG subgroup analysis by Head et al1. Importantly, analysis for group by disease (such as LM or three-vessel disease) interactions showed that either revascularisation strategy (PCI or CABG) remained protective of MACCE outcomes, whether the LM or 3VD groups were treated. Even adjusting for baseline patient characteristics such as age and gender, known to impact upon prognosis for coronary revascularisation, there were no significant differences in the overall odds ratio for five-year MACCE rates.
These results extend findings from the recent analysis of US vs. European clinical outcomes for the SYNTAX CABG (randomised and registry) cohort1. No differences in MACCE rates existed between Europe and the USA (28.7 vs. 24.3%; p=0.11), although higher revascularisation rates for US patients were observed (15.0 vs. 9.8% for Europe; p=0.011), driven by repeat PCI (14.6 vs. 9.2% for CABG; p=0.005). The current study shows that these differences also exist between both individual centres and countries, for PCI and TVR, but not for CABG, and not driven by lesion complexity (SYNTAX score, number of bifurcations, trifurcations), risk assessment (EuroSCORE), or presence of LM versus 3VD. Whether local hospital factors, closer follow-ups, or variable revascularisation thresholds drive these differences remains unclear.
This analysis also demonstrates the importance of using appropriate heterogeneity testing for RCTs, particularly for studies with larger sample site numbers and uneven strata sizes. In the multicentre PLATO study6, 33 pre-specified secondary endpoint analyses were performed, with three showing significance for interaction, in particular for patients enrolled in North America (p=0.045). The observed interaction (MACCE HR 1.25 for North America, HR 1.27 for the USA vs. 0.84 overall)7 was an unexpected finding, and suggested that geographic variation in recruitment may have influenced responsiveness to ticagrelor. Whether this was biologically plausible8, or due to chance7, remains unknown.
Where rare differences do occur, how may they be explained? Are they due to statistical or trial design features, patient, hospital, or regional level factors, or due to chance alone? Certainly, international cardiovascular trials that compare revascularisation procedures may be more sensitive to standards of care than pharmacology trials. If these differences do persist after appropriate stratification or adjustment for clinical factors in the analysis, there may be implications for health policy and regulatory authority approval, as was initially the case for the PLATO study. The results from the current study highlight the limitations of relying purely on fixed effects hypothesis tests for heterogeneity, and support the need for more comprehensive pre-specified heterogeneity analyses for these types of cardiovascular trial.
Finally, the results from this analysis also increase the utility of the SYNTAX five-year data for future pooled analyses examining PCI vs. CABG revascularisation outcomes, as we near five-year endpoints for a number of revascularisation trials. Where appropriate modelling is not performed, even the most well performed pooled analyses may raise more questions than answers. In a meta-analysis of four previous trials (ARTS, ERACI-II, MASS-II, SOS) comparing five-year outcomes of bare metal stents to CABG, patient-level data were pooled to improve power for subgroup analysis9-13. No treatment effect heterogeneity for composite MACCE was found, although treatment effect heterogeneity was observed for five-year mortality alone for SOS vs. the other trials (p<0.001). Further analysis of the high-risk subgroups, without the use of appropriate modelling, did not fully account for the findings9. This highlights the importance of the current study and its potential contribution to further revascularisation analyses.
Limitations
Considering the non-inferiority SYNTAX study design, lack of inclusion of the registry population for this analysis may have limited the strength of the analysis. Similarly, fixed effects models may drop sites or strata with sparse data from the analysis, potentially diminishing model efficiency. To overcome this, analyses were strengthened using interaction terms for both the fixed and random models. One of the study strengths is that this is one of the first analyses to highlight the lack of heterogeneity standards for reporting in key cardiovascular trials. Many authors now contend that pre-specification in analysis protocols for specific heterogeneity assessments may improve any new trial’s findings. Given the regional variations that have been well reported in some ACS studies, this analysis should reassure clinicians that no significant regional variations in treatment effect exist for the SYNTAX five-year follow-up study.
Conclusions
Geographic variability did not impact upon treatment effects for the SYNTAX five-year outcomes study, supporting the generalisability and robustness of the findings from this multicentre randomised controlled trial.
| Impact on daily practice Trials relying on multi-region patient recruitment may show treatment effect variability between regions that affects the initial study results, as was the case for the PLATO study. By showing no significant heterogeneity of treatment effect on five-year clinical outcomes, our findings support the SYNTAX trial’s generalisability and robustness, and indeed its place in current revascularisation guidelines. |
Guest Editor
This paper was guest edited by Emanuele Barbato, MD, PhD, FESC; Cardiovascular Center Aalst, Belgium and Department of Advanced Biomedical Sciences, University of Naples Federico II, Naples, Italy.
Acknowledgements
The authors would like to acknowledge the input from individual SYNTAX site investigator teams.
Funding
The SYNTAX study was funded by Boston Scientific.
Conflict of interest statement
P.W. Serruys, A.P. Kappetein, F-W. Mohr, M-C. Morice, B. Chevalier are Investigators for the SYNTAX Group. Otherwise they have no conflicts of interest related to this manuscript. The other authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.