Abstract
Aims: Distal embolisation during carotid artery stenting (CAS) is the main cause of cerebral complications; thus, the amount of embolisation occurring during CAS can be considered as a surrogate endpoint of cerebral complications. Our aim was to find patient characteristics which are associated with a higher risk of embolisation during CAS.
Methods and results: From January to December 2010 all consecutive patients undergoing CAS with embolic protection at three medium- to high-volume Italian centres were prospectively enrolled in this multicentre study. After CAS, the embolic debris was classified by visual inspection into two groups: “scarce” (no debris or hardly visible debris), and “relevant” (visible embolic debris) embolisation. Two hundred and thirty-six consecutive patients (79% males, 32.7% symptomatic) were enrolled. Open cell stents were used in 52.7% of the patients, distal filters were employed in 85.5% and proximal protection in 14.5%. Procedural success was achieved in 100% of procedures. Relevant embolisation was observed in 16.1% of patients, including those who suffered all the periprocedural complications (4.2%). At multivariate statistical analysis, high circulating LDL cholesterol and C-reactive protein levels were the only factors associated with relevant embolisation.
Conclusions: In this study, high circulating LDL cholesterol and C-reactive protein levels were associated with relevant embolisation after CAS, opening up the hypothesis that therapy with statins before elective CAS may reduce plaque embolisation and improve outcome. (EudraCT number: 016737-95).
Introduction
Carotid artery stenting (CAS) for severe carotid artery stenosis, a widely used technique to prevent stroke, should be carried out in centres with low 30-day death and stroke rates1,2. This procedure is associated with a low but consistent rate of neurologic complications which are mainly due to distal embolisation of atherothrombotic material during the procedure and in the following hours3. The risk of cerebral ischaemic complications is variable, and the ability to predict a higher embolisation risk would be helpful in tailoring the procedure to the patient and increasing the clinical success rate. Various factors have been correlated with a higher embolic risk, including symptomatic carotid stenosis, diabetes, hypoechoic plaque morphology at duplex ultrasound, tortuous vascular anatomy, and advanced age4,5. However, such factors are not able to predict accurately the occurrence of periprocedural ischaemic complications, which would help to prevent clinically relevant strokes. A method of reliably predicting distal embolisation after CAS seems particularly attractive. The focus of this study was to evaluate prospectively patient characteristics which are associated with a higher risk of embolisation following CAS interventions.
Methods
STUDY PROTOCOL AND POPULATION
This study was a multicentre, prospective, single-arm study whose patients were enrolled between January and December 2010, reflecting contemporary management of carotid artery stenosis.
All consecutive patients undergoing CAS at three medium- to high-volume centres (>75 CAS interventions/year) were prospectively enrolled into the study. All patients were correctly informed as to the study purposes and signed an informed consent. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee.
Operators had to be certified for CAS and to have had adequate experience following current guidelines1.
Our patient population was composed of both symptomatic and asymptomatic patients with a clinical indication to CAS. All patients underwent anatomical evaluation of the culprit lesion, proximal vessels and aortic arch with magnetic resonance imaging. The angiographic cut-off of percent lesion stenosis was 80% in cases of patients who were asymptomatic, and 50% in cases where they were symptomatic. Patients were considered symptomatic if they had had a minor or major stroke related to the carotid lesion in the last six months, and were evaluated by the referral neurologist. Exclusion criteria were: total carotid occlusion; unstable cardiovascular disease; recent stroke (<1 month) and type III aortic arch (because we feared that it could increase the risk of procedural complications interfering with the study endpoints).
PROCEDURE
CAS was performed according to the operator’s experience and current guidelines. A proximal or distal embolic protection was mandatory, one or the other being used according to physician’s experience and preference. Both femoral and radial accesses were allowed. Pre- and post-dilatation after stenting was left to the operator’s discretion and the choice of the stent was free as well. Filters were washed with saline just after removal and immediately assessed by investigators. In case of Mo.Ma® Proximal Cerebral Protection Device (Medtronic, Minneapolis, MN, USA) use, the blood retrieved was passed into the basket and immediately assessed by investigators.
FOLLOW-UP AND STUDY ENDPOINTS
After entering the study, all patients received a complete neurologic evaluation; such an evaluation was repeated after 48-72 hours in order to assess possible manifest or sneaky post-procedural ischaemic-related complications. All patients received a clinical visit and MRI evaluation after one month. Neurologic symptoms or complications possibly related to other factors (e.g., contrast media or hypertensive state-related) were assessed and differentiated.
The main goal of the study was to find out which biometric or procedural parameter better correlated with the clinical outcome after the intervention and was thus able to predict the risk of distal embolisation. A complete analysis of all clinical, biological and procedural data including blood lipids, C-reactive protein (CRP), and pretreatment with statins was recorded.
The presence or absence of embolic debris in the filter, an event which has already been shown to be a surrogate endpoint of cerebral complications1, identified the two main groups used later for the analysis. Embolisation assessment was performed immediately after CAS by an experienced operator and subsequently had to be confirmed by the three primary study investigators. The embolic debris was classified by visual inspection into two groups: “scarce” (no debris or hardly visible debris), or “relevant” (visible embolic debris) embolisation.
STATISTICAL ANALYSIS
Continuous variables are expressed as mean±standard deviation (SD) and categorical variables as count and percentages, respectively. The heterogeneity of distribution of categorical variables was assessed by χ2 test with Yates’ correction or Fisher’s exact test as necessary; for continuous variables the Student’s t-test was used. Both univariate and multivariate logistic regression models adjusted for potential confounding factors were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs). All p-values were two-sided. An alpha value of 0.05 was set as the statistical significance threshold. Statistical analyses were performed using Stata software, version 11 (StataCorp LP, College Station, TX, USA).
Results
Two hundred and thirty-six consecutive patients undergoing CAS at three medium- to high-volume Italian centres were enrolled into this prospective study: 187 (79.0%) were males, and 77 (32.6%) were symptomatic for previous cerebrovascular accidents related to ipsilateral carotid disease. The mean age was 71±7.9 years. The embolic protection system consisted of distal filters and Mo.Ma in 84.5% and 15.5%, respectively, and procedural success was achieved in all of our study population. Thirty-day adverse cerebrovascular events including transient ischaemic attacks and major strokes were registered in 12 patients (5.1%). Table 1 shows the main procedural and follow-up clinical results of the study.
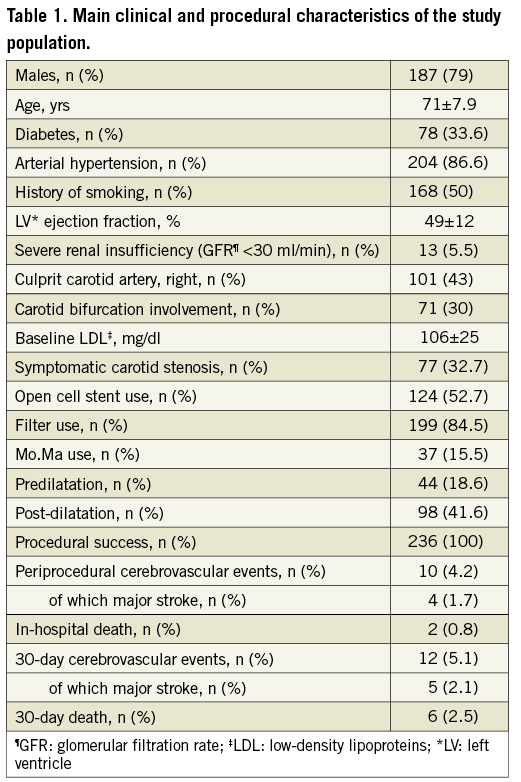
Relevant embolisation was observed in 38 patients (16.1%). In two patients of this group (and in none of the other one) a small intracranial embolus was visible at post-PTA intracranial angiography in a distal collateral segment of the middle and the anterior cerebral arteries. Both of these patients had a distal protection device which failed to capture the debris embolised during stenting. Intracranial PTA was not attempted because we observed an angiographic improvement after a few minutes and because both patients remained asymptomatic.
Nineteen patients with relevant embolisation (50.0%), and 127 (64.1%) of the other group had been on statin treatment for at least one month. Table 2 shows how the occurrence of serious and mild adverse events was significantly higher in the group of patients with a relevant embolisation during the index procedure.
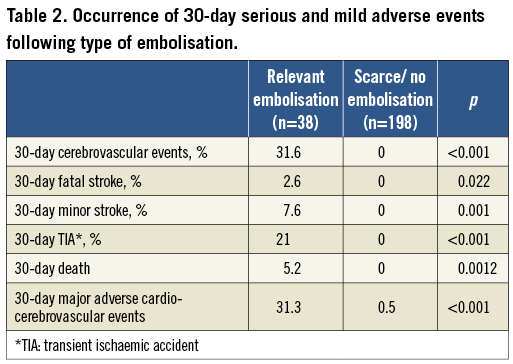
Univariate statistical analysis showed how only the presence of symptoms as a clinical indication for stenting, low-density lipoprotein (LDL) cholesterol and CRP values were significantly correlated with the occurrence of relevant embolisation. After adjustment for possible confounding factors like age, sex, clinical risk factors and procedural data, the multivariate analysis showed how the correlation with relevant embolisation remained for LDL cholesterol and CRP as continuous variables, and LDL cholesterol for the upper two quartiles of >90 and >120 mg/dl, with a positive linear trend (p=0.001) (Table 3, Figure 1). Moreover, contrast media use and in-cathlab blood pressure were matched with clinical outcomes and did not show any interference.
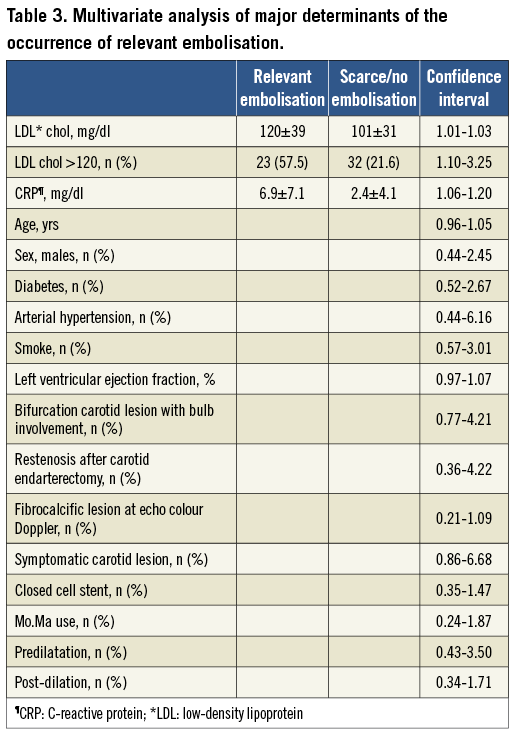
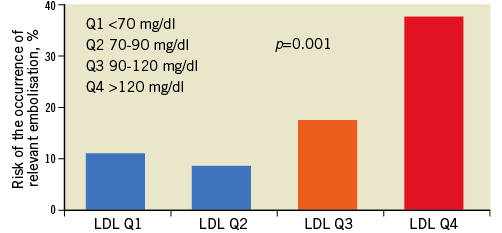
Figure 1. Risk of relevant embolisation as per LDL quartiles after adjustment for confounding factors, showing a highly significant linear trend.
Discussion
The main goal of this study was the determination of the items associated with a relevant embolisation after CAS. Our results confirm a previously reported hypothesis, namely that a large embolic burden in the filter is related to poor outcome after CAS, probably emphasising the limited value of currently available embolic protection devices in this setting6,7. What this study adds is that the most important independent factors associated with a relevant embolisation may be predicted and modified; thus, it seems possible to tailor the procedure to a patient’s profile and to improve the outcome of CAS.
Among the clinical and procedural factors associated with relevant embolisation in this pilot study, LDL cholesterol seems to be the most treatable, thanks to the use of statins. Moreover, we have to underline how preprocedural statin use in this study was associated with the occurrence of lower cerebrovascular adverse events although without a statistical significance (p=0.064).
Several studies have demonstrated that lipid-lowering treatment with statins modifies carotid plaque composition by increasing echogenicity and reducing lipid-rich necrotic core8,9. Interestingly, in a recent pilot study, a 30-day high-dosage atorvastatin treatment (80 mg/day) was associated with an increased echodensity, and presumably stabilisation, of carotid plaques10. However, intensive statin treatment has not yet been correlated with a reduction of ischaemic complications during and after CAS in asymptomatic patients. This is the goal of the currently ongoing ROSPREC trial, a multicentre randomised clinical trial we are conducting whose aim is to address the effect of six-week rosuvastatin pretreatment (40 mg/day) in reducing cerebrovascular events after CAS in asymptomatic patients.
CAS should be reserved to selected patients and performed by experienced operators in medium- to high-volume centres in order to keep the risk of procedural-related embolisms as low as possible. However, the results of the CREST trial show how CAS pays the price of a higher occurrence of periprocedural cerebrovascular events if compared to surgery (4.1% vs. 1.9%, p=0.0019)11. However, despite the use of proximal or distal embolic protection systems, now mandatory during CAS, a totally effective protection of the brain from all embolic fragments is not currently achievable, because some parts of the plaque do indeed pass the protections and embolise distally. Diffusion-weighted magnetic resonance imaging demonstrates the presence of new multiple asymptomatic small areas of cerebral ischaemia in almost all patients after CAS, even if this phenomenon is clinically silent in the vast majority of patients12,13.
The ability to predict cerebrovascular accidents accurately during CAS would be of primary importance for many reasons: treatment choice, access route, stent design, embolic protection type, antithrombotic regimen, etc. With this prospective study we were able to point out some of the factors which may help in tailoring the procedure to the specific risk of patients undergoing CAS. We have to underline that current practice, as outlined by international guidelines, should be followed and not delayed according to our results: e.g., in an unstable symptomatic patient where carotid revascularisation should be performed urgently, statin therapy should never take precedence over surgical or interventional treatment and thus should never result in a delay of urgent CAS.
Study limitations
This study has several limitations. The first of these is its design: it is a prospective single-arm study, and hypothesis-generating. The active role of statins on distal embolisation prevention after CAS has to be assessed in ad hoc studies such as the ongoing ROSPREC trial. The presence of debris after CAS was assessed by the operator because this is an evaluation that should be carried out immediately, although we believe that a centralised assessment could reduce the risk of bias.
Conclusions
In conclusion, this study shows how preprocedural LDL cholesterol and CRP levels are independently associated with relevant embolisation and adverse clinical outcome after CAS. The main implication of our results is that these factors may be predicted and modified, giving the chance to tailor and programme the procedure to a patient’s profile and therefore to improve the outcome of CAS.
| Impact on daily practice The risk of distal embolisation during CAS is a major drawback of this intervention. In this study we investigated all the clinical and interventional characteristics that were associated with distal embolisation occurrence, and found a strong correlation with preprocedural LDL cholesterol and CRP levels. These two items can be treated in a preventive way with pharmacological aids, to reduce the risk of distal embolisation and stroke after CAS. |
Conflict of interest statement
The authors have no conflicts of interest to declare.