Abstract
Aims: This study evaluates three-dimensional (3-D) reconstruction of the coronary arteries in assessment of angiographically borderline lesions.
Methods and results: Three-dimensional (3-D) quantitative coronary angiography (QCA) was performed for 41 intermediate coronary stenotic lesions (IL) in 31 patients. Measurements of cross-sectional stenosis (CSS), diameter stenosis (DS) and plaque volume (PV) were correlated with the fractional flow reserve (FFR) values measured with a commercially-available pressure guide-wire. FFR <0.75 was considered significant. Using FFR, only 9/41 lesions appeared haemodynamically significant (FFR <0.75). When compared to lesions with an FFR >0.75, these lesions had higher CSS (65.3±9.4% vs. 44.7±10.6%, p=0.0001), higher DS (48±5.7% vs. 32.5±9.9%, p=0.0001), and higher PV (41.6±7.6% vs. 29.4±6.7%, p=0.0005), as measured by 3-D QCA. Regression analysis showed significant correlations between FFR and CSS (r=-0.481, p=0.001) and PV (r=-0.443, p=0.004), and a modest correlation between FFR and DS (r=-0,320, p=0.041). Compared with FFR, a CSS of 57% had the highest sensitivity and specificity (88.9% and 87.5%, respectively) for determining significant IL. Multivariate analysis showed 3-D-determined CSS to better predict FFR compared to the other measured variables (p=0.012).
Conclusions: Parameters obtained by 3-D QCA showed a significant correlation with FFR values. A cross-sectional stenosis >57% obtained by 3-D QCA has a high degree of sensitivity and specificity to detect a haemodynamically significant intermediate coronary stenosis.
Introduction
Proper assessment and clinical decision making in angiographically intermediate coronary lesions is often difficult and still debated. Conventional two-dimensional (2-D) coronary angiography cannot fully characterise the clinical significance of coronary stenosis as it gives a two dimensional representation of a three-dimensional structure, making it unable to prFkigureovide reliable geometric information1. To overcome the limitations of angiography, functional assessment of coronary stenosis by fractional flow reserve (FFR) and intravascular ultrasound (IVUS) imaging are currently used to invasively define the severity of intermediate coronary lesions2-5.
It has been previously reported that deferring lesions of intermediate severity at angiography with an FFR ≥0.75 is associated with good clinical outcome. Pijls et al6 recently reported a risk of cardiac death or myocardial infarction <1% per year at 5-year follow-up after deferral of percutaneous coronary intervention (PCI) of an intermediate coronary stenosis based on FFR ≥0.75, which is not decreased by stenting. Similarly, deferring intermediate coronary artery lesion intervention based on IVUS guidance (minimal lumen cross-sectional area (CSA) >4.0 mm2) has been correlated with a low event rate7. Nevertheless, each of these invasive modalities has its limitations8,9, is time consuming and associated with higher costs.
Three-dimensional (3-D) reconstruction of standard coronary angiography using an algorithm integrating single-plane images provides more detailed geometric information about coronary artery lesions than conventional 2-D angiography and has been recently validated10. To date, no data are available regarding the relationship between the 3-D reconstruction parameters and FFR. Accordingly, we sought to evaluate the relationship between 3-D reconstruction parameters and FFR values, and to clarify whether or not 3-D reconstruction has the clinical potential to assess the hemodynamic significance of intermediate coronary stenoses.
Methods
Patient population
A total of 41 intermediate coronary lesions (appearing by visual estimation as stenoses >40% but <70% of the coronary luminal diameter) in 31 patients were studied consecutively by intracoronary pressure measurements and three-dimensional reconstruction at diagnostic catheterisation or before catheter-based intervention. Each vessel studied had an isolated stenosis. Exclusion criteria were patients with ST-segment elevation myocardial infarction, previous coronary artery bypass graft surgery, cardiogenic shock and extremely tortuous coronary arteries. Written informed consent for all procedures was obtained from each patient and the study was approved by the local ethics committee.
Cardiac catheterisation and intracoronary pressure measurements
A 5 or 6 Fr guiding catheter was used to engage the coronary artery ostium. After intra-arterial administration of 5000 IU of heparin, 200 µg of intracoronary nitro-glycerine was given, and coronary angiograms were obtained from multiple projections taken at 15-30 frames per second. Baseline angiograms of the target lesion(s) were made from at least two views separated by not less than 30° from each other. A commercially available 0.014» pressure wire (Pressure Wire, Radi Medical Systems AB, Uppsala, Sweden) was then advanced into the coronary artery to a position distal to the target lesion, and steady-state maximum hyperaemia was induced by the continuous infusion of 140 µg/kg/min of IV adenosine administered through the femoral vein. This state of maximum hyperaemia was maintained for at least two minutes to enable reliable coronary pressure measurements. FFR was calculated as the ratio of the distal coronary pressure divided by the proximal coronary pressure under maximal hyperaemia11,12, and a value of FFR <0.75 was considered significant in determining inducible ischaemia2,13.
Three-dimensional coronary reconstruction
Three-dimensional reconstruction of the coronary arteries was made using novel 3-D reconstruction software (IC-3D, Siemens AG, Munich, Germany) installed to a computer connected to the catheterisation laboratory where the conventional two-dimensional coronary angiography film is delivered to the software. The analysis can be done directly online during the coronary angiography procedure or offline after the end of the procedure using the 2-D coronary angiography CD placed in the CD-Rom of the computer and plying the film using the 3-D software. We processed all our patients using the offline analysis. Average time for the 3-D reconstruction procedure was three to five minutes for every patient by choosing two images acquired from the routine angiographic study where the lesion was clearly apparent and separated from each other by at least 30° (the software fails to generate the 3-D model when the views are separated from each other with less than 30°). The required segment to be examined was marked from proximal to distal in each one of the two chosen views (Figure 1) and by clicking on the 3-D reconstruction icon in the software, the software applied directly to do the 3-D model automatically creating the 3-D reconstruction of the segment under examination (with three-dimensional mobility character on the screen), showing one of the two views used for the reconstruction and giving quantitative analysis of the 3-D model (Figure 2).
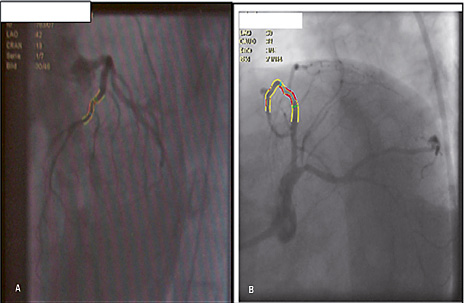
Figure 1. Two orthogonal two-dimensional views used for three-dimensional reconstruction of an intermediate lesion within the left anterior descending artery. The lesion is analysed in two orthogonal two-dimensional images to obtain a three-dimensional reconstruction and quantitative analysis of the 3-D model. A. left anterior oblique 42° cranial 13 view, B. left anterior oblique 21° caudal 31° view.
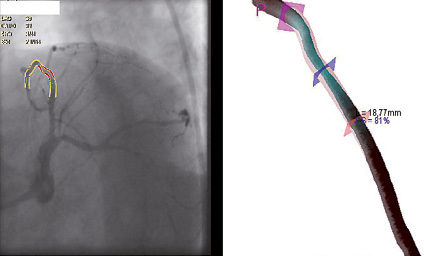
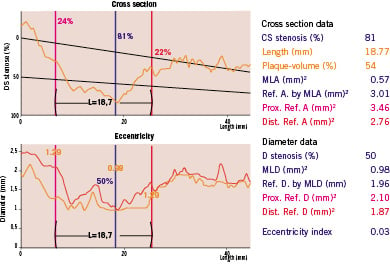
Figure 2. Three-dimensional reconstruction of an intermediate lesion within the left anterior descending artery. The lesion is analysed in two-dimensional images to obtain a three-dimensional reconstruction and quantitative analysis of the 3-D model (the software shows only one of the two analysed views, here showing the left anterior oblique caudal view). Lesion length (L) (proximal and distal harsh marks) and percent cross sectional stenosis (CSS) are shown on the 3-D reconstruction image. CS: cross section; mm: millimetre; Ref. A: reference area; MLA: minimal lumen area; Prox. Ref. A: proximal reference area; Dist. Ref. A: distal reference area; D : diameter; MLD: minimal lumen diameter; Ref. D: reference diameter; Prox. Ref. D: proximal reference diameter; Dist. Ref. D: distal reference diameter
Cross-sectional percentage stenosis (CSS%), diameter stenosis (DS), plaque volume (PV), minimal lumen area (MLA), minimal lumen diameter (MLD), lesion length and eccentricity index were measured automatically by the 3-D software and the obtained measurements were correlated with the FFR values.
Statistical analysis
Data evaluation was performed using a statistical software package (Minitab, version 13.1). Continuous variables are expressed as mean values ±SD and were analysed with the Student’s t-test or Mann-Whitney test, as appropriate. Discrete variables are presented as counts and percentages and were analysed by Pearson’s chi-square or Fisher’s exact test, as appropriate. A scatter plot distribution was used to correlate the absolute values of FFR with the different 3-D reconstruction parameters. Receiver Operating Characteristic (ROC) curves were used to determine the sensitivity and specificity of all 3-D reconstruction values at a specific cut-off point. Multivariate analysis was performed to select the best determinant of FFR less than 0.75. A p-value less than 0.05 was considered statistically significant.
Results
Patient and lesion characteristics
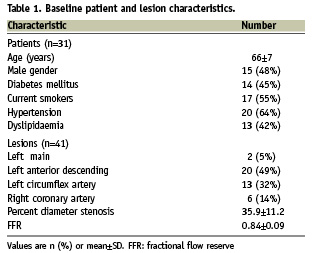
Forty-one coronary lesions in 31 patients were studied (Table 1). Two lesions were located in the left main, twenty in the left anterior descending, thirteen in the left circumflex, and six in the right coronary artery. The mean percent diameter stenosis was 35.9±11.2%. In all cases studied, coronary pressure was successfully measured without complications. The mean FFR value was 0.84±0.09 (range, 0.64 to 1.0). According to FFR measurements, nine lesions were functionally significant with an FFR value of less than 0.75, while 32 lesions had an FFR value above 0.75. Using
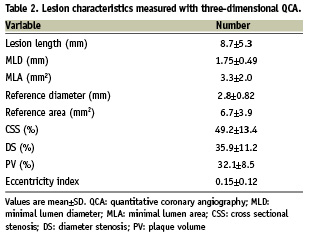
3-D QCA analysis, the mean MLD was 1.76±0.49 mm, the mean reference diameter was 2.8±0.86 mm, and the mean CSS was 49.2±13.4% (Table 2).
3-D reconstruction versus FFR
The relationship between 3-D variables and FFR was examined. Patients with an FFR value < 0.75 had a higher percentage CSS (65.3±9.4% vs. 44.7±10.6%, p=0.0001), higher DS (48±5.7% vs. 32.5± 9.9%, p=0.0001) and higher PV (41.6±7.6% vs. 29.4±6.7%, p=0.0005) (Table 3). Regression analysis showed a significant inverse correlation between FFR and CSS (r=-0.481, p=0.001, Figure 3). Plaque volume also showed a significant inverse correlation (r=-0.443, p=0.004), while DS only demonstrated a modest inverse correlation with FFR (r=-0,320, p=0.041).
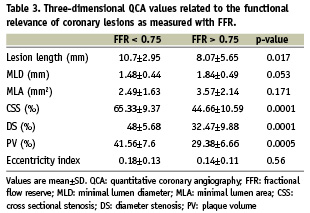
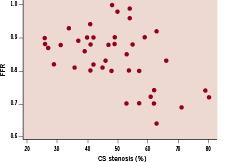
Figure 3. Scatterplot of fractional flow reserve (FFR) against cross sectional stenosis (CSS). The correlation between these two variables is –0.48; there is significant evidence of non-zero correlation (p= 0.001)
Compared with an FFR value of less than 0.75, the sensitivity and specificity curves for the 3-D reconstruction measurements were observed as in Figures 4 and 5. The best agreement with the FFR was found when the percent cross-sectional stenosis was >57% (sensitivity 88.9%, specificity 87.5%, area under the curve 0.93), and when the percent diameter stenosis was >45% (sensitivity 88.9%, specificity 90.6%, area under the curve 0.93). By multivariate regression analysis, the most independent determinant of FFR among percent CSS, percent DS, plaque volume, MLA and MLD was percent CSS measured by 3-D QCA (p=0.012).
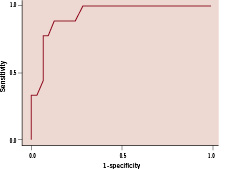
Figure 4. Receiver Operating Characteristic (ROC) curve for percent cross-sectional stenosis (CSS). The best cut-off value for an FFR<0.75 was for a CSS >57% (sensitivity 88.9%, specificity 87.5%, area under the curve 0.93).
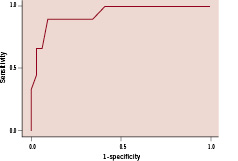
Figure 5. Receiver Operating Characteristic (ROC) curve for percent diameter stenosis (DS). The best cut-off value for an FFR<0.75 was for a DS >45% (sensitivity 88.9%, specificity 90.6%, area under the curve 0.93).
Discussion
To the best of our knowledge, this is the first study to evaluate 3-D angiographic coronary reconstruction parameters for assessment of the functional severity of intermediate coronary stenoses in comparison to FFR. Two important findings can be drawn from our study: (1) 3-D reconstruction parameters showed a significant relationship to the FFR values, and (2) 3-D reconstruction cut-off point of percent CSS of 57% had a potential to predict an FFR estimation below or above the ischemic threshold.
Three-dimensional reconstruction of the coronary arteries is a new technique that was developed mainly to overcome the problem of vessel foreshortening in 2-D angiographic images. Vessel foreshortening is due to the two-dimensional representation of three-dimensional structures and may cause errors in the assessment of lesions or the selection and placement of stents10,14, that is why after visual assessment of the lesions, patients were sent directly for pressure wire evaluation of the coronary lesions without 2-D QCA assessment. In addition, 3-D reconstruction provides geometric information about the coronary artery tree and coronary lesions, including percent cross sectional stenosis and percent diameter stenosis. Using these parameters to help determine the functional significance of intermediate coronary lesions makes 3-D coronary angiography a promising tool for evaluation of lesion severity in the cardiac catheterisation laboratory.
Until now, there is no single method that can provide both anatomic and functional data to permit more accurate decisions in the management of patients with intermediate coronary lesions. The currently available techniques in the cardiac catheterisation laboratory are FFR for physiological assessment and IVUS for anatomic assessment.
Patients with angiographically moderate coronary lesions can be safely managed without revascularisation on the basis of FFR measurements6,15,16. In the recently published Fractional Flow Reserve versus Angiography for Guiding Percutaneous Coronary Intervention (FAME) study, routine measurement of FFR in patients with multivessel coronary artery disease who are undergoing PCI with drug eluting stents significantly reduced the rate of the composite end point of death, non-fatal myocardial infarction and repeat revascularisation at one year follow-up17. However, the use of a pressure wire for assessment of intermediate lesions is limited by its reliance upon achieving maximal hyperaemia. This limitation to the use of FFR is most prominent in patients with severe micro-vascular disease, in whom maximal hyperaemia may not be reached, thereby falsely elevating the measured FFR value. This has been previously demonstrated in patients with a large myocardial infarction who undergo early (within 48 hours) assessment with FFR18,19.
On the other hand, intravascular ultrasound permits direct measurement of the lumen, coronary artery wall and components of atherosclerotic plaques20,21. In a study by Abizaid et al7, deferring intermediate coronary artery lesion intervention based on IVUS guidance (minimal lumen CSA ≥4.0 mm2 and/or minimal lumen diameter (MLD) ≥2.0 mm) has been associated with a low event rate (2% chance of death or myocardial infarction) at an average follow-up of 13 months. However, what is still not completely clear is the benefit to treat lesions with an IVUS CSA <4.0 mm2. The high event rate associated with these lesions should be weighed against the risk of revascularisation and usually depends upon the subjective decision of the operator. Furthermore, IVUS-derived values for estimation of lesion severity only apply to the proximal and mid segments of major epicardial arteries22. In a trial evaluating the ability of three-dimensional intravascular ultrasound (3-D IVUS) to predict the physiologic significance of coronary lesions, the authors found that physiologic severity of coronary lesions is primarily influenced by lumen area and lesion length and can be established by 3-D IVUS23.
Both pressure wire and IVUS are relatively expensive and time consuming techniques. In addition, they increase the burden of an invasive procedure with passage of a pressure wire or a guidewire and IVUS catheter in the coronary arteries, together with the administration of larger amounts of heparin and contrast agent, thereby exposing the patient to more procedural risk and increasing the duration of exposure to radiation. Compared to pressure wire and IVUS, 3-D reconstruction of the coronary arteries is not time consuming and can be performed off-line as well as on-line without any need for more invasive manoeuvres. For using Multi-Slice Computer Tomography (MSCT) as a non-invasive method for assessment of ischaemia-inducing coronary stenoses, many studies unfortunately demonstrated that anatomical assessment of coronary stenosis severity by MSCT does not reliably predict its functional significance24-26.
The mean percent diameter stenosis measured by 3-D QCA was 35.9±11.2% for lesions assessed visually as 40-70% stenoses. This is due to the limitation of the visual estimation by its poor accuracy and high inter- and intra-observer variability1.
Our data reveal that cross sectional area stenosis is the most important individual 3-D variable able to judge a haemodynamically significant stenosis. Several histo-pathological studies have demonstrated that angiographic evidence of stenosis is usually not detected until the plaque cross-sectional area approaches 40% to 50% of the total cross-sectional area of the vessel27-29. Also several studies have demonstrated a strong correlation between cross-sectional area stenosis obtained by IVUS and FFR22,30. Briguori et al22 evaluated 53 lesions in 43 patients with both IVUS and FFR and found that an area stenosis >70% had a high sensitivity and specificity in predicting an abnormal FFR value (<0.75). Takagi et al30 also showed that an IVUS-derived area stenosis >60% best correlated with an FFR value <0.75. These data are consistent with our finding that a CSS >57% obtained by three-dimensional reconstruction best predicted an FFR <0.75.
Conclusion
Three-dimensional reconstruction of conventional coronary angiography can be a practical tool in the catheterisation laboratory to provide critical anatomic and functional data that permit more accurate decisions in the management of patients with intermediate coronary lesions. A cross sectional stenosis >57% obtained by 3-dimensional QCA has a high degree of sensitivity and specificity to judge a haemodynamically significant intermediate coronary stenosis. Larger studies are required to confirm these findings.
Acknowledgements
The authors are grateful to the clinical research group at the Herz-Kreislauf-Zentrum Segeberger Kliniken GmbH. Our special thanks go to Mr. D. Robinson for his professional statistical support.