Early restoration of antegrade blood flow is key for patients with ST-segment elevation myocardial infarction (STEMI). Primary percutaneous coronary intervention (PCI) with stent implantation is routinely recommended in current guidelines for STEMI1. However, for those with stable blood flow and non-obstructive residual lesions, the non-stenting approach might be an option. Consequently, acute and chronic stent-related complications (distal embolisation, stent thrombosis, and restenosis) could be avoided, especially in younger STEMI patients with longer life expectancy. With a better understanding of the pathophysiology of STEMI, new concepts are emerging for a tailored management of STEMI, such as deferred PCI. The contradictory results of deferred trials have made it not routinely recommended for STEMI23.
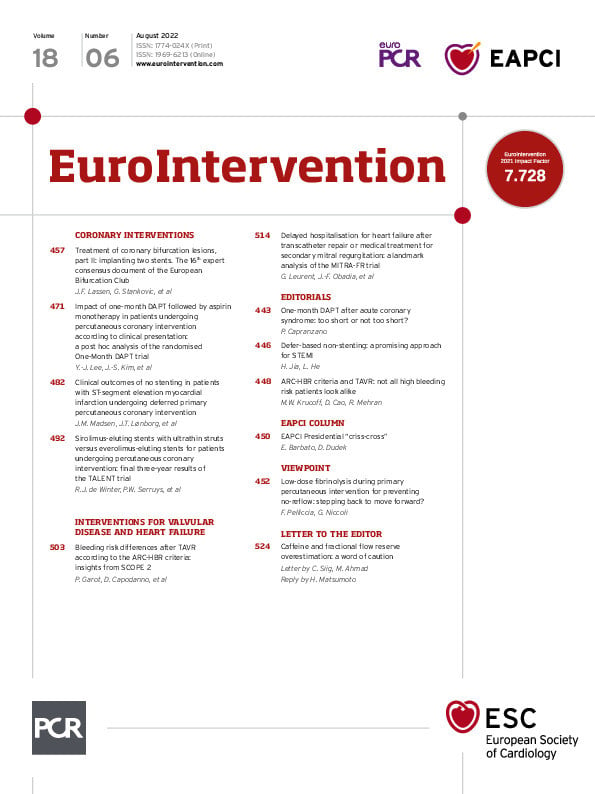
In the current issue of EuroIntervention, Madsen et al discuss their post hoc analysis of the DANAMI-3-DEFER study, which explored the safety and effectiveness of a defer-based non-stenting strategy for STEMI4.
In DANAMI-3-DEFER, thrombectomy and balloon dilation were performed to achieve stable flow during primary PCI for the patients allocated to the deferred stenting group. The deferred procedure was conducted after 24-48 hours from the index intervention. Those with culprit lesions with ≤30% angiographic residual stenosis assessed visually, no significant thrombus, and/or no visible dissection were treated without stenting. A total of 84 non-stenting patients in the deferred group were enrolled in the current study. The remaining 590 patients treated with immediate stenting were set as the control group. In a median follow-up duration of 3.4 years, the primary endpoint (a composite of all-cause mortality, recurrent myocardial infarction, and any unplanned target vessel revascularisation [TVR]) was comparable between the deferred non-stenting and immediate stenting groups. Secondary clinical endpoints and sensitivity analyses all showed similar results.
The work of Madsen and colleagues reconfirmed the concept of “more taking-out, less implantation” for STEMI and fused it with the deferred stenting idea. Another report (the SUPER-MIMI sub-study) also explored the possibility of the defer-based non-stenting strategy and found that 4 of 57 non-stented culprit lesions presented rethrombosis, 10.5% underwent target lesion revascularisation (TLR), and 82.5% of patients remained event-free at 4.1 years5. Of note, the decision to stent or not was at the discretion of the operator in their study. The different results between the SUPER-MIMI study and Madsen's may be due to different reperfusion strategies during the index procedure. In the SUPER-MIMI substudy, all patients had high thrombus burden, 63.2% of the non-stented cases received thrombus aspiration, and 50.9% were treated with glycoprotein IIb/IIIa inhibitors (GPI). In the study by Madsen et al, plain old balloon angioplasty (POBA) was used in 71.4% of patients and thrombus aspiration in 7.2% during initial PCI.
Notably, in the study by Madsen it al, the non-stenting criteria were mainly established based on angiographic diameter stenosis without knowledge of the lesion's characteristics. Intravascular imaging, specifically OCT should be used to characterise lesions and to help make a decision in the event of an eroded plaque with enough lumen to allow the omission of stenting. The EROSION and EROSION III trials have confirmed the role of OCT in the tailored management of STEMI678. For patients with TIMI flow 3 and residual angiographic diameter stenosis ≤70%, the majority of OCT-defined erosions and over 40% of OCT-defined ruptures could be treated with the non-stenting strategy at primary PCI8.
These exploratory studies have demonstrated that the non-stenting strategy is safe and feasible for selected STEMI patients with non-obstructive stenosis and stable haemodynamics after possible pretreatment. However, several issues remain to be further concretised to generate a paradigm shift towards the application of this defer-based non-stenting strategy: the detailed (qualitative and quantitative) angiographic and/or intravascular imaging criteria for the non-stenting approach; the selection of pretreatment (POBA, thrombus aspiration, purely wire) for different lesion characteristics and the indications for GPI use; and the duration of dual antiplatelet therapy.
The defer-based non-stenting strategy raised by Madsen and colleagues provides a novel direction in the individualised management of STEMI. Their findings make new sense of the “deferred” concept and give us hope that for acute STEMI patients, once stable blood flow has been achieved, the next step might offer various choices for tailored patients. Randomised trials with effective clinical endpoints are warranted to optimise this novel approach.
Conflict of interest statement
H. Jia has received research grants from the National Key R&D Program of China (2016YFC1301103) and the National Natural Science Foundation of China. L. He has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.