Abstract
Aims: To identify asymptomatic patients with impaired cerebral perfusion using CT perfusion (CTP) technique during staged carotid stenting (CAS) and cardiac surgery.
Methods and results: This is a prospective, non-randomised study in 16 neurologically asymptomatic patients designed to analyse cerebral perfusion using CTP before and after CAS. Mean transit time (MTT) was significant lower and cerebral blood flow (CBF) was significantly higher in the non-target hemisphere compared to the target hemisphere before treatment (4.64±1.08 s vs. 5.67±1.29 and 57.37±24.90 s vs. 48.19±13.02, respectively). Mean dMTT (absolute difference in MTT values between treated and untreated hemisphere) decreased from 0.92±1.08 s before to 0.04±0.30 s after carotid revascularisation (p<0.05) and mean relative CBF (ratios of the treated to the untreated hemisphere) increased from 0.92±0.12 to 1.04±0.12 after revascularisation (p<0.05). Subgroup analysis based on pre-treatment dMTT showed significant changes in 50% of the patients with larger dMTT. There was one transient ischaemic attack reported 30 days after combined procedure.
Conclusions: A significant improvement of cerebral perfusion after carotid stenting is shown in about 50% of the asymptomatic patients in this study. This suggests the potential presence of a compromised cerebral circulation in asymptomatic patients with severe carotid artery disease scheduled for cardiac surgery.
Introduction
The management of concomitant severe carotid and coronary artery disease is controversial. The incidence of perioperative stroke during cardiac surgery is 2%, however in the presence of severe carotid disease a fourfold increased risk has been described1,2. The initial studies of combined or staged carotid endarterectomy (CEA) in these patients were conceived in an attempt to reduce perioperative morbidity and mortality. In the presence of concurrent carotid and coronary artery disease, carotid stenting (CAS) now offers an alternate means of carotid revascularisation and seems to pose less risk of myocardial ischaemia than CEA.
Evidence suggests that hypoperfusion due to a severely stenotic carotid artery or micro-embolisation from an ulcerative plaque form part of the different mechanisms for peri-operative neurological events during open heart surgery3,4. Hypotension induced ischaemic neurological injury during cardiopulmonary bypass is hard to avoid in patients with severe carotid stenosis. During cardiopulmonary bypass cerebral auto-regulation is severely impaired, making cerebral blood flow directly proportional to cerebral perfusion pressure5. This finding provided a logical reason for carotid revascularisation prior to or in combination with cardiac surgery.
In patients with isolated carotid disease, haemodynamic factors have long been associated with the symptomatic status of stenosis6. Also, the importance of cerebral haemodynamics in association with the risk of stroke in patients with severe carotid stenosis (CS) and occlusion has been described7-10. In asymptomatic subjects with severe CS however, little or no proof of the above is available. Only a paucity of literature is available elucidating the haemodynamics in asymptomatic patients with CS undergoing cardiac surgery6. It has been published recently, that CT perfusion (CTP) technique is able to show impairment of cerebral perfusion in a subgroup of patients with unilateral symptomatic carotid artery stenosis11. This study concluded that relative pre-treatment CT perfusion values can identify symptomatic patients in whom carotid revascularisation would most likely lead to an improvement in cerebral haemodynamics after treatment.
We hypothesised that in asymptomatic patients CTP analysis before CAS can be used to allow identification of those patients who benefit the most of carotid revascularisation through protection against haemodynamic changes during cardiopulmonary bypass.
Methods
Patients
We analysed 56 consecutive patients planned for CAS and cardiac surgery from May 2005 to October 2009 at our centre in a prospective, non-randomised study. Patients were considered asymptomatic if an ipsilateral cerebrovascular event had not occurred four months prior to cardiac surgery. Significant carotid artery stenosis was defined as a luminal diameter reduction of more than 80%, according to NASCET criteria12,13. The indications for cardiac surgery included symptomatic (documented myocardial ischaemia) severe coronary artery disease (including bypass failure) not eligible for percutaneous revascularisation, symptomatic valve disease and disease (aneurysm/dissection) of the ascending aorta or arch requiring reconstructive surgery, following institutional guidelines14-15. We included patients with bilateral carotid atherosclerosis, patients who agreed undergoing CTP before and after CAS and patients without contraindication for CT scan. Patients were excluded if they had severe renal impairment (eGFR < 35 ml/min), peripheral vascular disease that precluded femoral artery access, major neurological deficit, or any other illness that impeded their ability to provide informed consent. Patients with severe diffuse atherosclerosis of the common carotid artery, chronic total occlusions, and long pre-occlusive lesions (“string sign” lesions) were also excluded. Sixteen patients met the inclusion criteria for the current study. All patients were scanned within three days prior to the treatment and the majority one month after stent placement. The degree of stenosis in the treated carotid artery (target) was assessed before revascularisation and at one month follow-up in all patients using duplex ultrasound.
The study was approved by the medical ethics committee of our hospital and written informed consent was obtained from all patients.
Endpoint definition
Primary endpoint were absolute and relative measurements of cerebral blood volume (CBV), cerebral blood flow (CBF) and mean transit time (MTT), comparing CT perfusion parameters of both hemispheres before and after revascularisation.
Secondary endpoints were the incidence of death, stroke or myocardial infarction (MI) at six months after the CAS and cardiac surgery.
CT perfusion scanning
Dynamic CTP source images were acquired using a 16-detector-row scanner (MX8000 IDT; Philips Medical Systems, Cleveland, OH, USA). A bolus injection of 40 ml contrast with an iodine concentration of 300 mg I/ml (Ultravist 300; Schering AG, Berlin, Germany) was administered at 5 ml/s followed by a 40 ml-saline chaser bolus at 5 ml/s using a power injector with a dual head system (Stellant Dual CT injector; Medrad Europe BV, Beek, The Netherlands) for all perfusion scans. CTP data were transferred to a post-processing workstation (Philips Medical Systems, Best, The Netherlands) on which CBV, MTT, and CBF were calculated. Time-enhancement curves derived from contrast passage through the anterior cerebral artery and the superior sagittal sinus provided the arterial input function (AIF) and venous output function (VOF), respectively. For AIF, an operator placed a region of interest (ROI) over the both anterior cerebral arteries at each slab. Hereafter the computer selected the optimum curve, based on height of the peak and the size of the area under the curve. The same was done for VOF within the superior sagittal sinus. Visual inspection was always performed to assure that the complete AIF and at least three points of the down slope of the VOF were included. The CBV was calculated as the ratio of the area under the time concentration curve of the first bolus passage through the tissue to that of the area under the curve of the VOF. The MTT, the average time required by the blood to cross the capillary network, was calculated by a deconvolution operation16. According to the central volume principle, CBF was calculated from measured CBV and MTT values: CBF=CBV/ MTT17. This method has shown to be most accurate at lower injection rates18-19. The same operator always chose AIF and VOF, visually controlled the curves, and performed the subsequent post-processing of the ROIs for quantitative measurements. Imaging protocol and post-processing have been extensively described in a previous manuscript11.
CAS procedure and subsequent cardiac surgery
Carotid stenting was performed following the highest standard of care using a distal embolic protection device. Cardiac surgery (including coronary artery bypass, valve or reconstructive surgery of the ascending aorta) was scheduled four weeks after CAS, unless clinical instability required earlier intervention. This in accordance with our institutional policy of staged strategy, which has been described earlier14. Patients were examined by a neurologist prior to CAS and before discharge.
Data collection and patient follow-up
Telephone follow-up interviews were conducted at one month and thereafter six monthly intervals by a dedicated full time research coordinator. In case of an event, hospital notes or death certificate were consulted when possible. An independent board-certified neurologist graded symptoms according to functional testing using the modified Rankin score if a cerebrovascular event occurred20.
Statistical analysis
CT perfusion analysis provides absolute perfusion data for each pixel in the target and non-target hemispheres; CBV expressed as ml/100 g tissue, MTT expressed in seconds and CBF expressed in ml/100 g tissue/min. We chose to include relative perfusion data in our analysis by normalising measured values in the target hemisphere to those in the non-target hemisphere because brain perfusion measurements are subject to high inter-subject variation and influenced by physiologic stimuli21-22. As a relative measure for MTT we chose the absolute difference in MTT values between the target and the non-target hemisphere (dMTT) because MTT itself is derived from the difference between the width of the curves (AIF and voxel of interest). The ratios of target to non-target hemisphere were calculated for relative CBF (rCBF) and relative CBV (rCBV) because these parameters are derived from the ratio of the areas under the attenuation curves (VOF and voxel of interest). The mean of measurements in the two evaluated slabs was calculated for both absolute and relative data for each CTP scan.
We first analysed the total group of patients and compared absolute pre- and post-treatment values and target versus non-target hemispheres using a paired t-test. Subsequently, we analysed the relative data and compared pre- and post-treatment dMTT, rCBF and rCBV. Finally, we split our study population into two equal groups based on the baseline dMTT: in group 1 we analysed eight patients with lower dMTT, in group 2 eight patients with higher dMTT. The MTT was chosen because it is least affected by the differences between grey and white matter and because it has shown to be significantly correlated with cerebral perfusion pressure (CPP) and is therefore considered to be a sensitive index of CPP23-25. Pre-treatment and post-treatment values for rCBV, dMTT and rCBF were compared using the Wilcoxon signed ranks test in each group. Statistical analysis was performed using statistical package SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered statistically significant.
Results
Patient characteristics
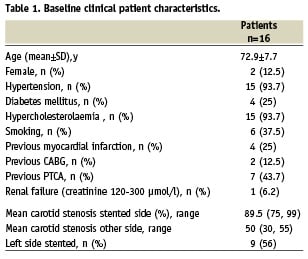
The baseline clinical characteristics of all patients are shown in Table 1. No patient had undergone a previous carotid endarterectomy or carotid angioplasty or stenting. Adequate stent-apposition without haemodynamic significant (re)stenosis or stent thrombosis was seen in all patients on control duplex examination. Mean arterial blood pressure during pre- and post-treatment CT was not statistically significant. In the majority of patients the post-treatment CT was performed before cardiac surgery. Pre- and post-treatment CT were performed in 16 patients.
Angiographic/stenting and cardiac surgery results
One patient reported a transient ischaemic attack (TIA) following CAS. None of the included patients had symptoms between pre- and post-treatment CT. The mean angiographic degree of stenosis was reduced from 89.5%±5% (before stenting) to 5%±9%. In all patients the same type of stent (Acculink; Abbott Laboratories, Abbott Park, Il, USA) was implanted successfully, using only one type of distal protection device (Emboshield filter, Abbott). The mean time interval to cardiac surgery after CAS was 24 days, with a range of one day to three months. In four patients coronary artery bypass grafting was combined with valve replacement. There was no minor or major stroke or myocardial infarction reported within 30 days of the combined procedure. One patient died of documented pneumonia one month after cardiac surgery.
Perfusion parameters
ABSOLUTE PERFUSION PARAMETERS
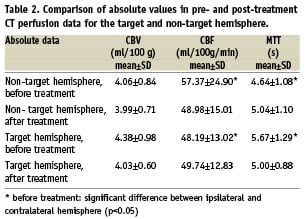
When comparing CT perfusion parameters of both hemispheres before and after revascularisation, we found a significant lower MTT and higher CBF in the non-target hemisphere compared to the target hemisphere before treatment (4.64±1.08-s vs. 5.67±1.29 and 57.37±24.90 vs. 48.19±13.02, respectively). There were no significant changes after revascularisation in both hemispheres (Table 2).
RELATIVE PERFUSION PARAMETERS
The mean dMTT decreased from 0.92±1.08s before to 0.04±0.30s after carotid revascularisation (p<0.05) and mean rCBF increased from 0.92±0.12 to 1.04±0.12 after revascularisation (p<0.05). The rCBV did not change significantly (Table 3 and Figure 1).
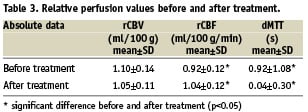
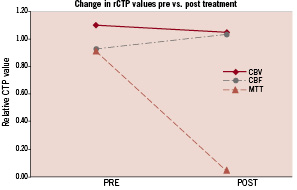
Figure 1. Changes in relative cerebral perfusion values before/after carotid artery stenting.
SUBGROUP ANALYSIS BASED ON DMTT
In the first eight patients baseline dMTT was <0.7s, in the second half baseline dMTT was >0.7s. The effect of carotid revascularisation on cerebral perfusion parameters was dependent on the baseline dMTT (Table 4). In the eight patients of group 1, no significant change in any of the relative CT perfusion values was detected. In the patients of group 2, mean dMTT decreased from 1.67±1.06s to -0.03±0.33s (p<0.05) and rCBF increased from 0.86±0.09 to 1.1±0.14 (p<0.05) but no significant changes in rCBV occurred (Figure 2).
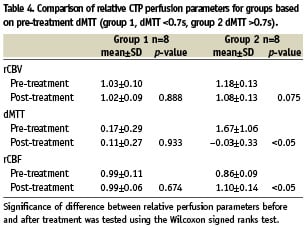
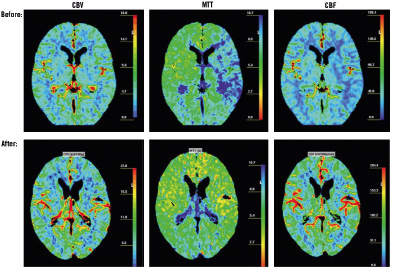
Figure 2. An illustration of CT perfusion images: the mean transit time (MTT), cerebral blood volume (CBV), and cerebral blood flow (CBF) maps are shown before and after CS.
Discussion
It is well recognised that there are a number of potential aetiologies for perioperative stroke in the cardiac surgical patient, including embolisation of atherosclerotic debris or thrombus from the aortic cannulation site, air embolus, left ventricular thrombus, aortic dissection, low cardiac output, and intracerebral disease, in addition to extracranial significant carotid artery disease. While clinically significant carotid disease may be responsible for only a minority of perioperative strokes in this patient population, it is the one aetiology that can be identified preoperatively and non-invasively and can be prevented by timely intervention26.
The importance of haemodynamic factors in the pathogenesis and treatment of ischaemic cerebrovascular disease in patients undergoing cardiac surgery is a matter of on-going debate. Stratifying patients based on the degree of CS fails to differentiate those with reduced cerebral perfusion pressure from those with non-compromised cerebral haemodynamics. Moreover, it seems hazardous to use the degree of CS to decide whether a patient may be at increased risk for stroke on haemodynamic grounds. This implies that choice of medical therapy or revascularisation should not be based on these considerations. It has been established that the effect of CS on cerebral circulation could be more accurately assessed by analysis of arteriographic circulation patterns, depicting the adequacy of collateral circulatory pathways and patterns27. It remains to be determined whether the patients with true cerebral circulatory compromise are at an increased risk for stroke, either spontaneously or during cardiopulmonary bypass. Among others, thrombo-embolisation plays a role in the origin of perioperative stroke in patients undergoing cardiac surgery. However, it seems likely that the effects of thrombo-embolic particles are influenced by the presence of perfusion deficits28.
The increasing number of endovascular procedures for the treatment of CS performed during the last decade has intensified the need for monitoring the outcome of these procedures. The semi-quantitative evaluation of cerebral perfusion makes it a reliable tool for the follow-up of patients who undergo CAS. CTP before and after CAS has shown to allow for assessment of pre-treatment inter-hemispheric differences, which may or may not resolve after treatment.
The first finding of this study is that there is significant improvement of cerebral perfusion after carotid stenting even in this selected group of asymptomatic patients. This suggests the presence of a compromised cerebral circulation due to carotid stenosis, even though these patients have never been aware of this. The second finding is that not all patients have shown such an improvement. Based on pre-treatment dMTT, in about 50% of the patients improvement is seen, while in the others no significant reduction of mean transit time or any other perfusion parameter was observed.
Gaudiello et al demonstrated that the normalisation of the perfusion parameters occurs in all patients as soon as one week after the stent-placement procedure29. A recent study published by Trojanowska et al showed a trend toward haemodynamic normalisation at three days post-stenting but an incomplete normalisation in a small percentage of patients at six months30. The selection of patients, the interventional procedure performed, and the volume of study could all account for the differences. Most interesting, Sanchez-Arjona et al have shown, with a different method of study, significant haemodynamic changes in the anterior brain circulation, ipsilateral to CAS at six hours after the procedure31.
The neuropsychologic consequences of an ischaemic event are well known, though generally neglected because the attention of the physician is driven toward the more striking and invalidating motor deficits32. However, recent articles have demonstrated that even asymptomatic patients with an elevated ICA luminal narrowing show higher depression scores or reduced neuropsychologic test performances that seem to be reversed by CAS33-35. Notwithstanding the fact that only an improved cerebral perfusion has been demonstrated in this study, a lesser stroke risk or improvement in neurocognitive functioning during cardiac surgery might be considered as potential benefits after CAS.
Study limitations
Although CT perfusion analysis yields absolute quantitative data, several studies have shown that values obtained with this technique are subject to physiological variations and are influenced by post-processing steps24,36. Some of these limitations, intrinsic to absolute perfusion values, are overcome by using relative perfusion parameters, relating the absolute perfusion data in the target hemisphere to the contralateral hemisphere. The advantage of this approach is the elimination of physiological variations and inter-patient differences in total cerebral perfusion but the disadvantage is that results will be more difficult to interpret when significant stenoses are present in both carotid arteries. Also, the presence of a carotid stenosis influences the AIF and may result in overestimation of absolute MTT and underestimation of absolute CBF. However, the use of relative data largely eliminates these effects11.
Secondly, we did not compare CT perfusion values to a reference standard such as PET or Xe-CT. However, previous studies have already shown that CBF measured with CT perfusion correlates well tot these established techniques18.
Third, we did not evaluate the effects of the configuration of the circle of Willis nor the presence of (irregular) plaques, because for such a multi-factorial analysis many more patients are needed and the purpose of this study was to evaluate whether it is possible to discriminate patients with different response to carotid intervention based on cerebral perfusion at baseline.
Fourth, some patients had cardiac surgery before the post-treatment perfusion scan, which may have influenced cerebral perfusion pressure. How much this pressure is influenced in patients with compromised cerebral auto regulation remains unclear, but is not inconceivable.
Conclusion
The management of concomitant severe carotid and coronary artery disease is controversial. Limited data are available on cerebral haemodynamics in association with the risk of stroke in asymptomatic patients with severe carotid stenosis undergoing cardiac surgery. Using CT perfusion technique, more specifically the mean transit time, a significant improvement of cerebral perfusion after carotid stenting is shown in about 50% of the asymptomatic patients in this study. This suggests the presence of a compromised cerebral circulation due to carotid stenosis, even though these patients are asymptomatic. The impaired perfusion observed in this patient population can be reversed. CAS prior to cardiac surgery might thereby positively influence the reduced neuropsychological functioning which has been described in asymptomatic patients with an elevated ICA luminal narrowing.