“You can also commit injustice by doing nothing.”
Marcus Aurelius
An 89-year-old lady is scheduled to undergo transcatheter aortic valve implantation (TAVI) with a balloon-expandable valve. Her aortic annulus is repeatedly measured at 430 mm² on a preprocedural computed tomography (CT). What valve size do you choose? What factors influence your decision? Would your choice be the same if the patient was a low-risk patient at the age of 69?
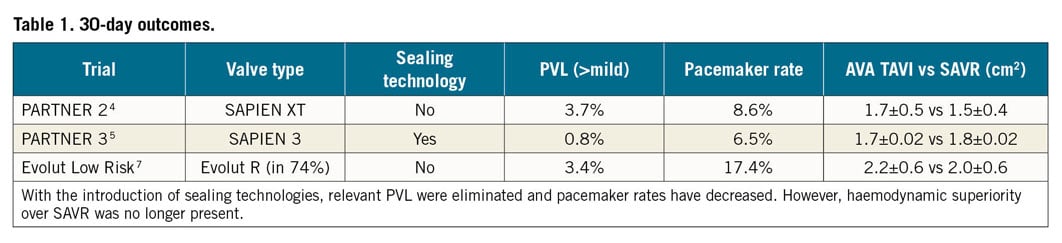
Today, a remaining challenge (or Achilles’ heel) of TAVI is the issue of sizing. Undersizing in TAVI can lead to paravalvular leaks (PVL) and suboptimal aortic valve areas (AVA), whereas oversizing is a risk factor for higher pacemaker rates and annulus ruptures1. While the problem of PVL was almost eliminated by technical advances (sealing skirts), the need for pacemakers was reduced by improved implantation techniques (high implantation). To allow ideal haemodynamics, optimal sizing and valve selection are aimed at achieving the largest possible AVA.
In 2012, the finding of even mild PVL being associated with worse outcome2 led to more aggressive oversizing. This was possible thanks to more accurate sizing techniques using 3D data sets from CT, resulting in implantation of larger valves3. TAVI outperformed surgical aortic valve replacement (SAVR) with regard to AVA (TAVI 1.7±0.5 cm² vs SAVR 1.5±0.4 cm², p<0.001)4. This was an important advantage of TAVI, as larger AVA improve haemodynamics and longevity. The introduction of effective sealing skirts was a blessing and a curse at the same time: PVL were almost eliminated, but haemodynamic superiority over SAVR was lost. In the PARTNER 3 trial, TAVI achieved smaller AVA as did SAVR (TAVI 1.7±0.02 vs SAVR 1.8±0.02, p=ns)5 and, in a series of Evolut PRO (including a sealing technology) implantations6, the achieved AVA paralleled the surgical AVA in the randomised trial7. This may in part be due to better surgical techniques, but still, moderate or severe patient-prosthesis mismatch was present in about 1/3 of TAVI patients5. To achieve as large an AVA as possible is important, particularly in younger, active, low-risk patients with a long life expectancy (Table 1).
The study of Breitbart et al8 in this issue of EuroIntervention helps us in our daily clinical decision making in several regards.
In 21 patients with contained annulus ruptures, conservative treatment was confirmed to be safe and without impact on prognosis. There was vigorous prosthesis oversizing in the population with contained rupture (on average 23% – in our example, this would correspond to a 26 mm valve prosthesis in an annulus of 430 mm²). Of note, >85% of patients were women. It is probable that women with a very small annulus are more likely to be implanted with a largely oversized valve. Alternatively, gender differences in tissue characteristics could play a role.
The prosthesis used was the SAPIEN XT valve (Edwards Lifesciences, Irvine, CA, USA) in >60% of patients, lacking a sealing technology and therefore forcing the operator to choose as large a prosthesis as possible. Can we conclude that vigorous oversizing seems safe and effective? Maybe, but there is a caveat to interpreting these data too enthusiastically: what we do not know from this study is the average oversizing in the remaining 98.9% of the population that did not experience annulus rupture. Also, the most feared annulus ruptures resulting in intraprocedural cardiogenic shock and often in in-hospital mortality were excluded from the current study.
We must be aware that “annulus rupture” does not equal “annulus rupture”, but rather describes a continuum of different stages (asymptomatic to cardiogenic shock). Further, annulus rupture is a general term used to describe a variety of injuries that may occur in the aortic root and left ventricular outflow tract during TAVI. While most of the cases of annulus rupture described here were “asymptomatic”, nevertheless one patient experienced intraprocedural pericardial effusion, and probably some of the 24% pericardial effusions and haematothoraces diagnosed post-procedurally were caused by the “contained” annulus ruptures.
The incidence of 1.1% of asymptomatic, benign annulus ruptures reported in the registry is probably underestimated, given the fact that post-procedural CT was only available in 60% of patients – the incidence will most likely be somewhere between the reported 1.1% and the 5% reported by another group performing a post-procedural CT in every patient9.
Back to our 89-year-old patient with an annulus of 430 mm². Depending on the amount of calcification, choosing a 23 mm valve is reasonable. If the patient is 69 years old where haemodynamics and longevity are more in focus, an elegant solution in case of borderline sizes is to choose the larger valve (26 mm in our example) and underfill the balloon (underexpansion of the valve prosthesis). If after valve implantation an unsatisfactorily high gradient is present or in case of PVL, the valve can be gradually expanded by post-dilatation if anatomical assessment allows for it. The elegant concept of underexpanding valve prostheses will, however, only reduce but not eliminate the incidence of annulus ruptures. As we learned from the study of Breitbart et al, annulus ruptures also occurred with the use of self-expanding valves if post-dilatation was used.
In conclusion, we learn from the study that we should not be too afraid of oversizing and striving for as large an AVA as possible. If in doubt, we recommend choosing a larger underfilled valve. In that way you still have options to “do something” if the result is not satisfactory.
However, as stated above, it is not only about PVL, AVA and annulus ruptures - the question remains whether the price to pay when aiming for large AVA is a higher pacemaker rate. Further, there is certainly more information in the pre-interventional imaging CT to predict PVL, pacemaker rate and risks of annulus rupture with regard to aggressive oversizing. Larger studies should analyse in more detail the pathophysiology of annulus rupture and its association with high-risk features. There is still a lot to do to optimise our TAVI results.
Conflict of interest statement
F. Nietlispach is a consultant and proctor for Abbott, Edwards Lifesciences and Medtronic. C. Gräni has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.