Appropriate sizing of the transcatheter heart valve (THV) is an important factor in minimising and preventing transcatheter aortic valve replacement (TAVR)-related complications such as valve embolisation, annular rupture, and paravalvular aortic regurgitation (PAR).
Transoesophageal echocardiography (TEE) and multislice computed tomography (MSCT) are the established tools for measurement of the aortic annulus prior to the procedure1,2.
Most current THV systems require oversizing of the annulus to get an optimal fit1. Inappropriate oversizing can cause heart block, aortic root haematoma and rupture1. Procedure balloon sizing is an additional, valuable tool to have in the TAVR armamentarium. It can help determine the appropriate THV size in cases with ambiguity between two different valve sizes. Balloon sizing can also serve as a stand-alone imaging modality for annulus/THV sizing. Patsalis et al showed that about 39% of their patients had borderline annulus size based on TEE2. They noted a significant reduction in PAR and in both 30-day and one-year mortality with the use of balloon sizing with aortography in addition to the conventional TEE sizing.
Understanding the technical caveats of balloon sizing is important. In this paper we describe how to perform accurate balloon sizing of the aortic annulus and selection of the THV using the previously described “right cusp rule”3,4. The balloon sizing technique described is applicable to both balloon-expandable and self-expanding THV. The self-expanding THV are more forgiving because they have a larger oversizing range than the balloon-expandable THV. When using a commercially available balloon for sizing, it is imperative to know the precise outer diameter of the balloon, which can differ from the nominal diameter specified by the manufacturer.
Step-by-step instructions for balloon sizing of the AV annulus:
− Place the angled pigtail catheter at the bottom of the right coronary cusp and use the “right cusp rule”3,4 to obtain the coaxial implantation view (Figure 1A). Under sufficient rapid pacing, inject 10-15 mL of contrast with a flow rate of 10 mL/s to ensure optimal visualisation of the three cusps. The distance between the non- and left coronary cusp hinge points correlates to the large annulus diameter (Figure 1A).
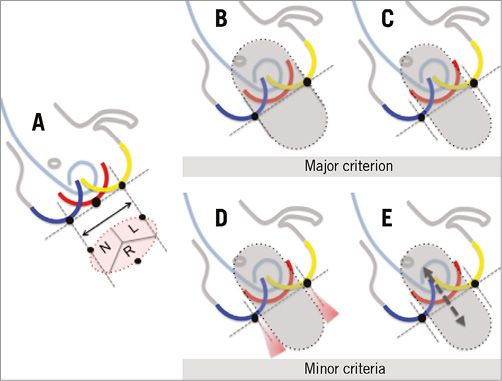
Figure 1. Schematic illustration of the major and minor criteria for balloon sizing of the aortic annulus. A) Obtain the coaxial implantation view using the “right cusp rule”. The hinge points are defined as the nadirs of the cusps. The distance between the hinge points of the non- and left coronary cusp correlates approximately to the large annulus diameter. Place the pigtail catheter in the right coronary sinus and, under sufficient rapid pacing, inject 10-15 mL of contrast with a maximum flow rate of 10 mL/s. B) & C) The major criterion for balloon sizing describes the anatomical relationship between the sinus hinge points and the balloon. In panel B, the balloon is large enough and reaches the hinge points; in panel C, the balloon is smaller than the annulus and does not reach the hinge points. D) & E) Minor criteria for balloon sizing describe the functional relationship between the contrast backflow and the movement of the balloon with regard to the size of the annulus. In panel D, there is contrast backflow with a fully expanded balloon suggesting insufficient seal of the annulus by the balloon. In panel E, there is up-and-down movement of the fully expanded balloon suggesting that the balloon is not well anchored to the annulus.
− Place the chosen balloon across the virtual aortic annulus and, under rapid pacing, fully expand the balloon prior to injecting the contrast media. The anatomical relationship between the sinus hinge points and the balloon describes the major criterion. In Figure 1B, the balloon is big enough and reaches the hinge points. In Figure 1C, the balloon is smaller than the annulus and does not reach the hinge points. The major criterion is the most important and reliable criterion that should be assessed first with balloon sizing. For choosing a THV size when it falls in the “grey zone” between two valve sizes, use the balloon that has the outer diameter of the smaller valve for the balloon sizing. For the balloon-expandable Edwards SAPIEN valve (Edwards Lifesciences, Irvine, CA, USA) for example, use a 20 mm Edwards balloon when deciding between a 20 mm and a 23 mm THV. If the 20 mm balloon reaches the hinge points, then implant the 20 mm THV. If the 20 mm balloon does not reach the hinge points, then implant the 23 mm THV. Similarly, use a 23 mm Edwards balloon when deciding between a 23 mm and a 26 mm THV, and use a 25 mm Edwards balloon when deciding between a 26 mm and a 29 mm THV5.
− The minor criteria involve assessing contrast backflow into the left ventricle (LV) and movement of the balloon during the balloon aortic valvuloplasty (BAV). Contrast backflow into the LV during the BAV (Figure 1D) suggests that there is insufficient coverage of the annulus by the balloon. Therefore, selection of the larger THV is recommended. Similarly, movement/watermelon seeding of the balloon during the BAV (Figure 1E) suggests insufficient anchoring of the balloon to the annulus. Therefore, selection of the larger THV is recommended. It is important to note that, if there is no backflow of contrast into the LV, or if there is no movement in the balloon when it is fully expanded, this does not necessarily mean that the balloon is of the right fit in the annulus. The minor criteria provide us with additional information and should always be used in conjunction with the major criterion. Selection of a THV size should not be based solely on the minor criteria.
Figure 2 depicts angiographic examples of the major and minor criteria of balloon aortic annulus sizing. Figure 2A1, Figure 2A2 and Moving image 1 depict the major criterion where the sizing balloon reaches the hinge points. In this scenario, implant a THV of the same size. Figure 2B1, Figure 2B2 and Moving image 2 depict the major criterion where the sizing balloon is smaller than the annulus anatomy and therefore does not reach the hinge points; here, the larger THV size should be chosen. Figure 2C1, Figure 2C2 and Moving image 3 depict the minor criterion where the sizing balloon is borderline large and it is uncertain whether it reaches the hinge points. However, during the aortogram there is backflow of contrast around the balloon and into the LV; here, the larger THV should be chosen.
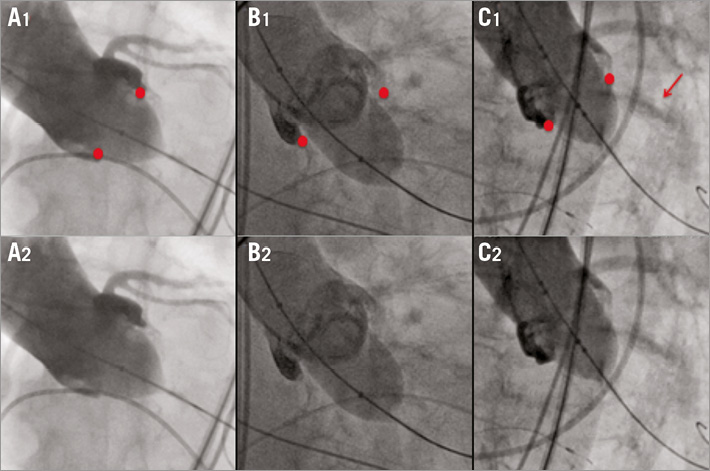
Figure 2. Angiographic cine images of the major and minor criteria for balloon sizing of the aortic annulus. A1/A2) Major criterion: sizing balloon reaches the hinge points; therefore, the balloon is large enough and a THV of the same size could be chosen. B1/B2) Major criterion: sizing balloon is smaller than the annulus and does not reach the hinge points; therefore, the larger size THV should be chosen. C1/C2) Minor criterion: sizing balloon is borderline large and it is uncertain that it reaches the hinge points; however, there is backflow of contrast around the balloon. Therefore, the larger size THV should be chosen.
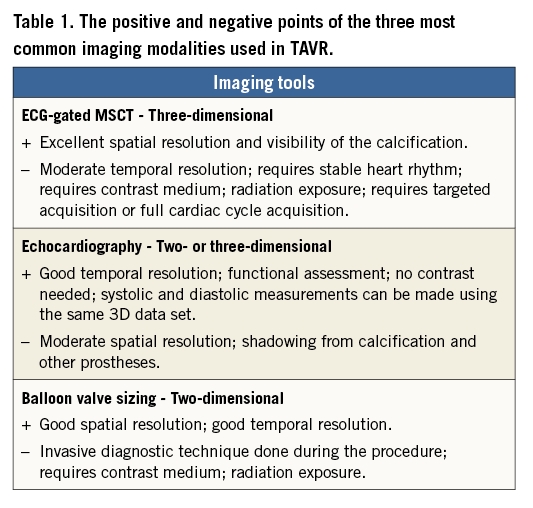
In conclusion, balloon sizing is a complementary technique to MSCT and conventional TEE sizing. It is especially helpful when there is uncertainty as to the annulus dimensions based on poor CT/echo quality, when the measurements fall in the “grey zone” between two valve sizes, and in the following unclear anatomical situations: bicuspid aortic valve, septal bulge, presence of mitral prosthesis, short coronary ostia distances, and in the presence of bulky cusps/valves. Balloon sizing mimics the valve implantation without having the valve in place; it gives us additional anatomical information that is not available with MSCT or TEE imaging. Balloon sizing allows us to assess visually how situations such as severe, eccentric calcifications and bulkiness of the cusps will affect valve implantation, functional results, and complications that may arise. In addition, the patency of the coronary ostia can be visualised during the balloon sizing. Table 1 shows the positive and negative points of the three most common imaging modalities used in TAVR.
Conflict of interest statement
A.M. Kasel is a medical consultant for and receives research support from Edwards Lifesciences. M. Thoenes is an employee of Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Major criterion A.
Moving image 2. Major criterion B.
Moving image 3. Minor criterion C.