Abstract
Aims: We sought to compare annular versus supra-annular sizing for transcatheter aortic valve implantation (TAVI) in patients with a bicuspid aortic valve (BAV).
Methods and results: In this retrospective single-centre analysis, we measured the aortic annulus (Ann) and intercommissural distance (ICD) on multidetector computed tomography scans in 217 BAV patients. With annular sizing being the default method for prosthesis size selection in all cases, we determined clinically relevant sizing errors and assessed the hypothetical impact of supra-annular sizing. Overall there was no significant difference between ICD and Ann (25.1 [23.5; 27.3] vs. 25.4 [23.6; 27.1] mm; p=0.24); intra-individually, ICD was similar to Ann in 26.7%, smaller in 40.1%, and larger in 33.2%. Annular sizing was appropriate in 96.3%, oversized in 0.5%, and undersized in 3.2% of cases. Supra-annular sizing would have resulted in a divergent size selection in 38.7% (smaller: 17.5%, larger: 19.8%, ICD out of range for TAVI prostheses: 1.4%) with potential improvement in a few cases with annular sizing errors, but potential worsening due to improper size selection in a much larger proportion of patients.
Conclusions: Annular sizing for TAVI in BAV is feasible and safe. The added value of supra-annular sizing is questionable.
Introduction
Transcatheter aortic valve implantation (TAVI) has become established as standard therapy for patients with severe aortic stenosis at high risk for surgical valve replacement1. The ongoing expansion of indications for TAVI to lower-risk populations will increasingly involve younger patients with bicuspid aortic valve (BAV)2. Concerns about performing TAVI in BAV relate to the complex aortic root anatomy with potentially increased procedural risks such as paravalvular leakage (PVL) and aortic root injury3. Even though recent evidence suggests that with the use of new-generation devices improved outcomes can be achieved in this subpopulation4, there are some unresolved issues that need to be addressed further. These include the most appropriate sizing method for TAVI in BAV patients, something which is a matter of debate. Whereas in tricuspid aortic valves annular sizing using multidetector computed tomography (MDCT) is the standard of care for the selection of the proper transcatheter heart valve (THV) size, for BAV it has been suggested to determine the intercommissural distance (ICD) 4 or 5 mm above the annular plane to account for the more complex aortic root morphology in BAV that may have supra-annular narrowing5. However, evidence supporting this alternative approach is scarce, and thus far no systematic comparison of these different sizing methods has been reported. In the present analysis, we compared annular versus supra-annular sizing for TAVI in patients with BAV.
Methods
STUDY DESIGN
Consecutive patients undergoing TAVI for native aortic stenosis between June 2011 and August 2018 at our centre were analysed retrospectively. Exclusion criteria included the absence or insufficient image quality of preprocedural MDCT (Figure 1). The procedures were performed using balloon-expandable or self-expanding/mechanically expandable THV (Supplementary Table 1). Baseline data including demographics, comorbidities, and risk scores were drawn from a prospective database. The study was performed in accordance with the Declaration of Helsinki and was approved by the local ethics committee.
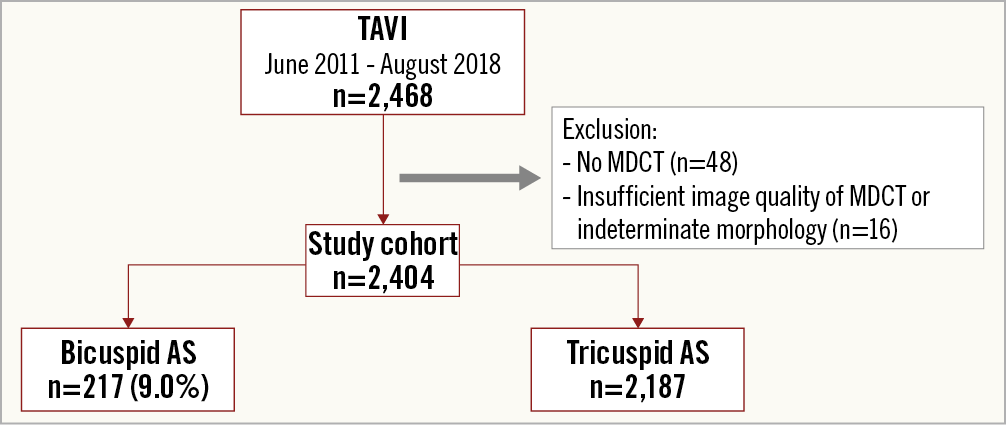
Figure 1. Study population. AS: aortic stenosis; MDCT: multidetector computed tomography; TAVI: transcatheter aortic valve implantation.
MULTIDETECTOR COMPUTED TOMOGRAPHY
MDCT examinations were performed with a 128-slice or a 384-slice dual-source scanner (SOMATOM® Definition or Force; Siemens Medical Solutions, Forchheim, Germany), as previously described6. Reconstructions were carried out using a cardiac-gated B26f or I26f algorithm with a slice thickness of 0.6 mm in systole between 30% and 40% and in diastole at 70% of the cardiac cycle. For image analysis, dedicated software (3mensio; Pie Medical Imaging, Bilthoven, the Netherlands) was used. Image quality was estimated using a four-point scale. All scans were evaluated by a single cardiologist (W.K. Kim) with profound experience in cardiac imaging and were systematically analysed for the presence of BAV using diastolic and systolic reconstructions7.
In addition to standard aortic root measurements, the ICDmax was determined as surrogate for supra-annular sizing 4 mm above the annular plane using the respective maximum value from systolic (ICDsys) and diastolic (ICDdia) reconstructions (Figure 2). According to the relation between the annulus size (Ann) and ICD, we defined a cylindrical (ICD=Ann±Ann*0.02), trapezoid (ICD
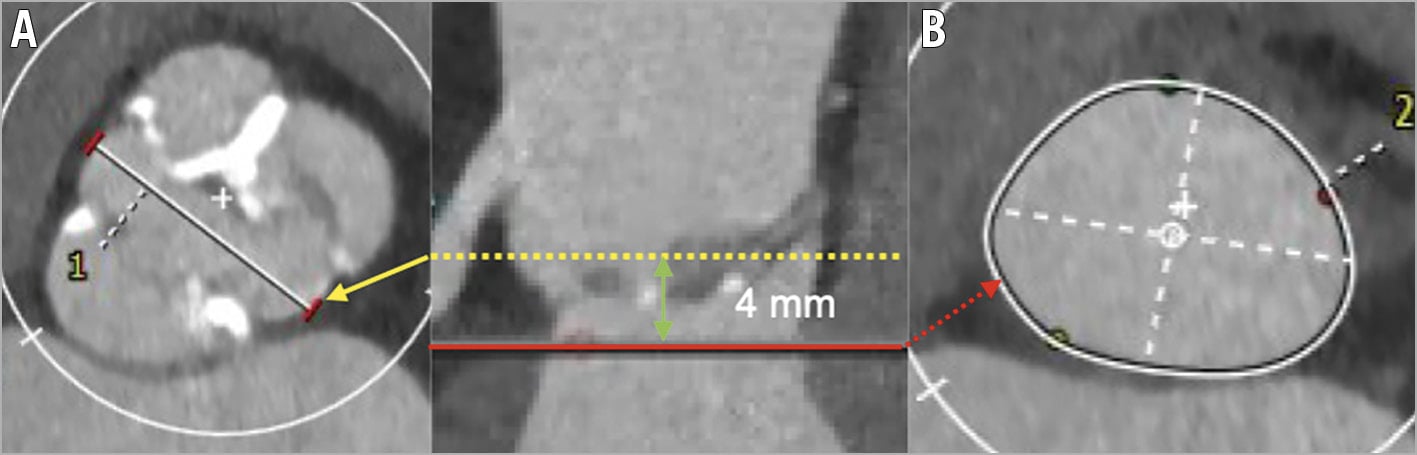
Figure 2. Aortic annulus and intercommissural distance on MDCT. Measurement of (A) the intercommissural distance 4 mm above the annular plane and (B) the aortic annulus in a bicuspid aortic valve.
SIZING
As the selection of the prosthesis size was commonly based on the maximum annulus diameter (Annmax) of systolic and diastolic reconstructions, for supra-annular sizing, the respective maximum value of systolic and diastolic ICD values was used (ICDmax). To estimate prosthesis sizing, we calculated the cover index annular sizing: CIAnn=100*([prosthesis size-Annmax]/prosthesis size) and the supra-annular sizing: CIICD=100*([prosthesis size-ICDmax]/prosthesis size). Nominal thresholds for correct sizing, undersizing, and oversizing of the various prostheses were derived from official recommendations9.
To account for cases of prosthesis size selection that were divergent from official recommendations, including systematic oversizing when using the ACURATE neo™ device (Boston Scientific, Marlborough, MA, USA)10, overfilling or underfilling of the SAPIEN 3 balloon (Edwards Lifesciences, Irvine, CA, USA), or undersizing in patients with severe device landing zone calcification, we took into consideration procedural outcomes to obtain a comprehensive clinical evaluation of sizing. Hence, a nominal oversizing or undersizing was only categorised as a clinically relevant sizing error in the presence of procedural complications potentially related to an inappropriate selection of the THV size (including PVL ≥2°, device embolisation, permanent pacemaker implantation, and annular rupture). Furthermore, we determined the hypothetical prosthesis size that would have been chosen when employing supra-annular sizing. In cases with complications due to annular oversizing, the selection of a smaller valve size according to supra-annular sizing was rated as potential improvement and vice versa. On the other hand, in cases with good procedural outcomes using annular sizing and discordant supra-annular sizing, we assumed an inappropriate size selection which hence was rated as potential worsening.
ECHOCARDIOGRAPHY AND AORTOGRAPHY
PVL was assessed on discharge transthoracic echocardiography according to established criteria11. All images were reviewed independently by two cardiologists with expert competence in imaging who were blinded to clinical parameters; in cases of disagreement mutual consensus was achieved. The position of the first implanted prosthesis was determined by measuring the distance between the annulus and ventricular aspect at the non-coronary and left-coronary cusps, as described earlier12.
OUTCOMES OF INTEREST
Procedural results were evaluated according to updated Valve Academic Research Consortium (VARC-2) criteria13. The primary outcome of interest was the rate of appropriate sizing. Secondary outcomes of interest were complications related to sizing, device success, and all-cause mortality at 30 days; mortality data were obtained from follow-up visits, via telephone interview, or from medical reports.
STATISTICAL ANALYSIS
Continuous variables are expressed as median and interquartile range (IQR), and categorical data are given as numbers and percentages. Continuous variables were compared with the Wilcoxon test or Kruskal-Wallis H test, and categorical data were analysed with the chi-square test or Fisher’s exact test. A two-sided p-value <0.05 was considered significant. All statistical data were calculated using SPSS, Version 21 (IBM Corp., Armonk, NY, USA).
Results
STUDY COHORT
Between June 2011 and August 2018, a total of 2,468 patients with severe native aortic stenosis underwent TAVI consecutively at our centre. After exclusion of 48 cases without preprocedural MDCT and 16 cases with indeterminate bicuspid phenotype (due to insufficient image quality or complex anatomy), the TAVI cohort consisted of 2,404 patients (Figure 1) with excellent, good, and acceptable image quality in 31.4%, 45.1%, and 23.4% of cases, respectively. Using MDCT criteria, we diagnosed 217 (9.0%) patients with BAV (median age 80.0 years [76.4-83.5], STS PROM 3.9% [2.4-5.6]). Baseline characteristics and procedural details are shown in Table 1 and Table 2. Results according to THV generation are illustrated in Figure 3.
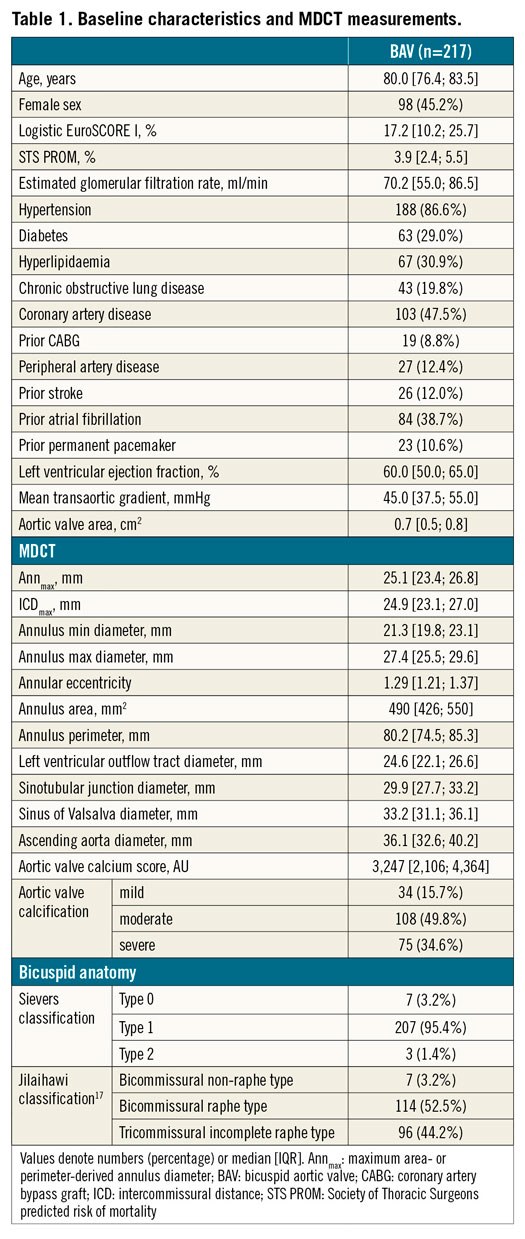
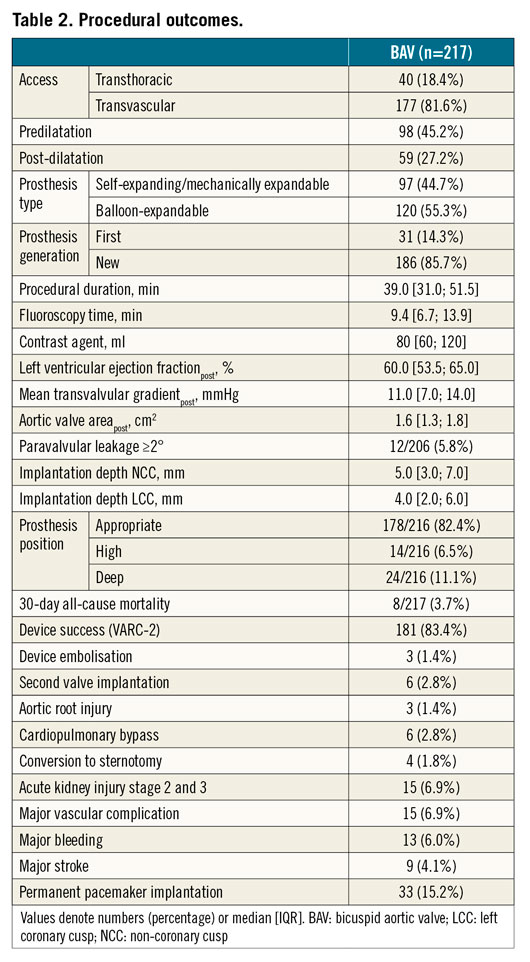
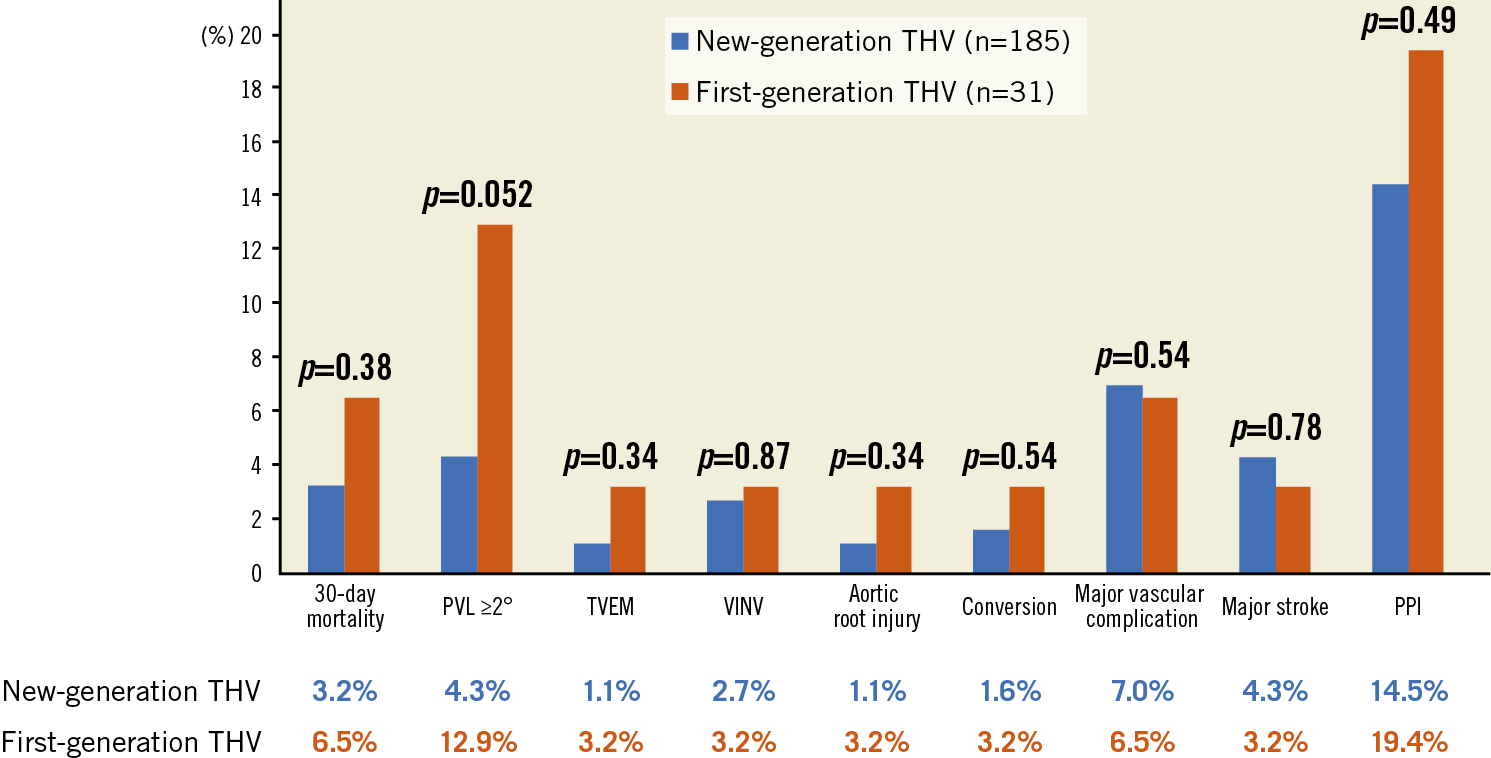
Figure 3. Outcomes of first- versus new-generation transcatheter heart valves. PPI: permanent pacemaker implantation; PVL: paravalvular leak; TVEM: transcatheter valve embolisation and migration; VINV: valve-in-valve.
ICD AND ANNULUS MEASUREMENTS
On average, ICDmax was similar to Annmax (25.1 [23.5; 27.3] vs. 25.4 [23.6; 27.1] mm; p=0.24). Intra-individually, ICDmax was similar to Annmax in 26.7% (cylindrical shape), smaller in 40.1% (trapezoid shape), and larger in 33.2% (inverse trapezoid shape).
ICDmax and the ICDmax/Annmax ratio differed according to the BAV subtype (Figure 4); the difference was greatest in patients with bicommissural non-raphe type (BiCNon-Raphe) (27.0 mm [25.8; 27.5]; 1.04 [0.99; 1.12]), followed by patients with bicommissural raphe type (BiCRaphe) (25.9 mm [24.2; 27.9]; 1.01 [0.97; 1.05]) and tricommissural incomplete raphe type (TriC) (24.2 mm [22.3; 25.9]; 0.98 [0.94; 1.02]; p<0.001 for both comparisons).
PROSTHESIS SIZE SELECTION
Supplementary Table 2 summarises complications potentially related to sizing errors (n=48, four patients had multiple complications). Using the aforementioned criteria, a small number of primarily sizing-related complications were identified among BAV (8/48; 16.7%). Under this premise, annular sizing in BAV was deemed to be appropriate in 96.3%, oversized in 0.5%, and undersized in 3.5% of cases.
Compared with annular sizing, supra-annular sizing would have resulted in a selection of similar sizes in 61.3%, upsizing in 19.8%, and downsizing in 17.5%, while in 1.4% the ICDmax would have been too large for currently available TAVI prostheses (Table 3).
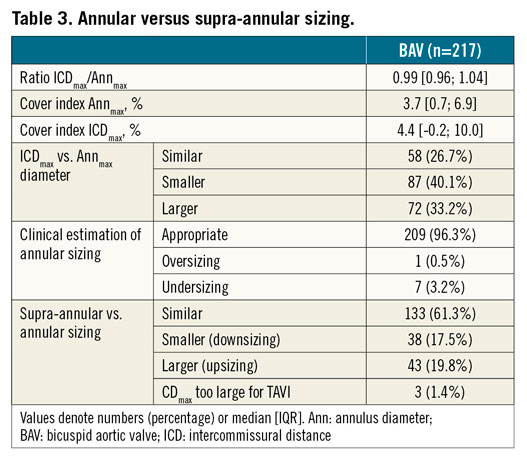
The proportion of upsizing was highest in BiCNon-Raphe-type valves (57.1%), whereas the proportion of downsizing was highest in TriC-type valves (27.1%) (Figure 4).
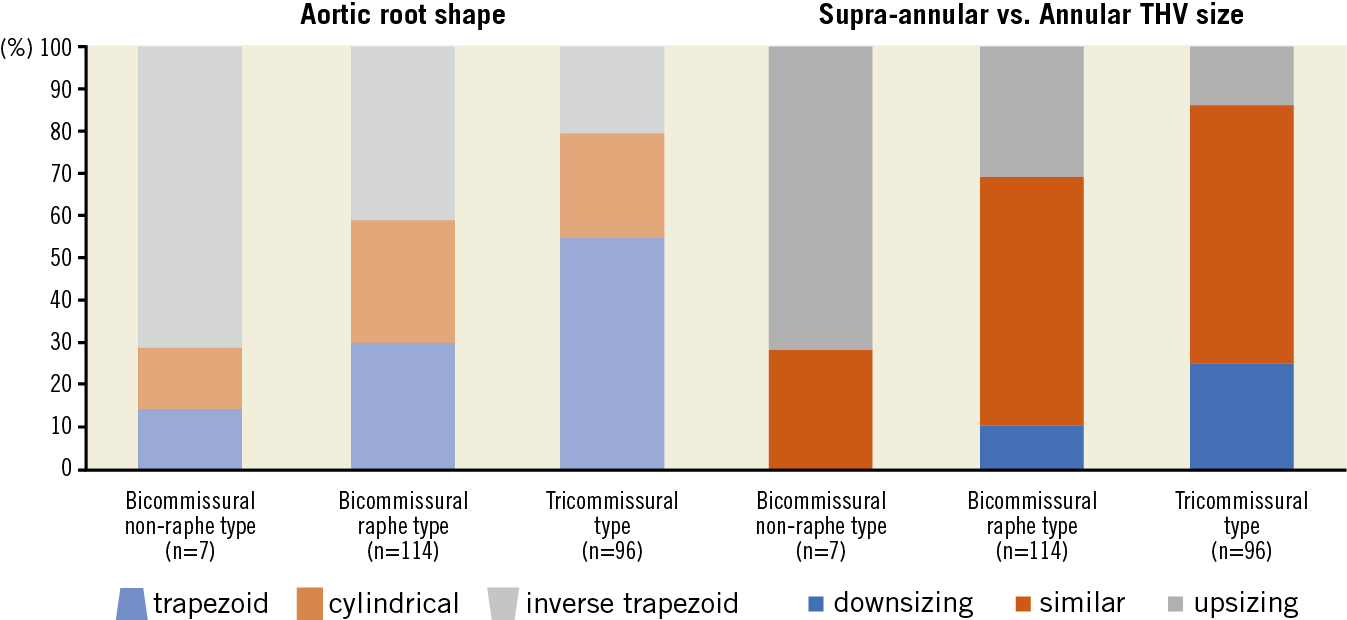
Figure 4. Intercommissural distance vs. annulus diameter. The proportion of patients with an inverse trapezoid shape of the aortic root (ICD larger than Ann) is more prevalent in bicommissural phenotypes, whereas a trapezoid shape (ICD smaller than Ann) is more common in tricommissural phenotypes. Accordingly, supra-annular sizing would lead more frequently to upsizing in bicommissural types and to downsizing in tricommissural phenotypes. Upsizing included three cases with ICD being too large for TAVI prostheses.
Among the cases with complications suggestive of annular sizing errors, supra-annular sizing would potentially have led to a more appropriate valve size selection in a few cases (n=5; 2.3%), exclusively in non-cylindrical aortic root shapes. In cases with good outcomes according to annular sizing, supra-annular sizing was divergent in a much larger proportion of patients (n=79; 36.4%) and may have resulted in a potential worsening due to inappropriate valve size selection, regardless of the underlying aortic root shape (Figure 5) or the THV type (Supplementary Figure 1).
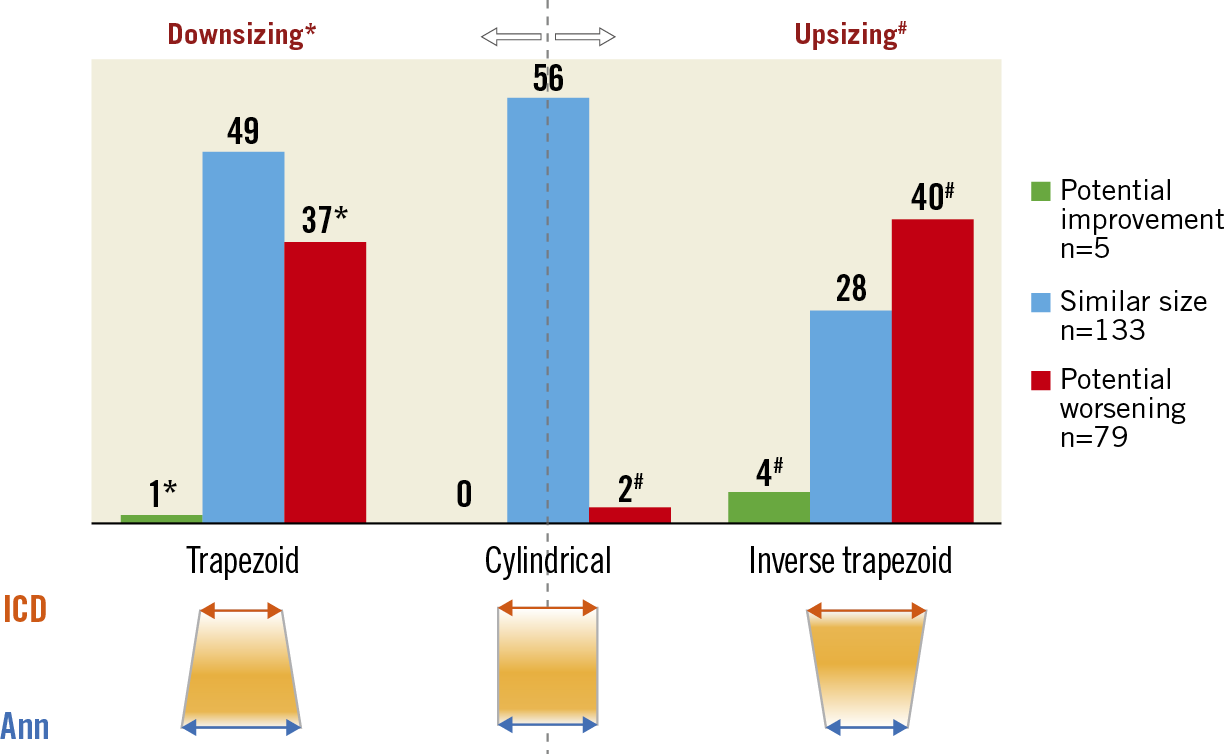
Figure 5. Aortic root shape and impact on sizing. Supra-annular sizing would have led to a potentially improved size selection in a few cases with non-cylindrical aortic root shape, but the proportion of cases with potential worsening due to supra-annular sizing was much larger irrespective of the aortic root shape. Downsizing occurred exclusively in patients with a trapezoid shape, whereas upsizing was more common in patients with an inverse trapezoid shape. The latter group included three cases in which the ICD was too large for currently available TAVI prostheses.
CYCLIC VARIATIONS OF ICD AND ANNULUS
Systolic and diastolic MDCT reconstructions were available in 214 (98.6%) and 211 (97.2%) patients, respectively. ICDsys (24.9 mm [23.1; 27.0]) was larger than ICDdia (24.4 mm [22.3; 26.4]; p<0.001). Furthermore, ICDsys in general was similar to Annsys (25.1 mm [23.4-26.8]; p=0.08), whereas ICDdia was significantly smaller than Anndia (24.8 mm [23.3; 26.8]; p=0.001). In detail, ICDsys was similar to Annsys in 34.6% of the cases, larger in 29.3%, and smaller in 36.1%. ICDdia was similar to Anndia in 26.3%, larger in 28.7%, and smaller in 45.0%.
Discussion
The main findings of the present study are:
1) In BAV, the relation between the diameter of the annulus and ICD varied according to the BAV subtype and resulted in different aortic root shapes (cylindrical, trapezoid, inverse trapezoid).
2) Annular sizing for TAVI in patients with BAV using various THV was feasible and safe and yielded good procedural outcomes in >95% of patients.
3) Supra-annular sizing would have resulted in divergent size selection in approximately 40% of cases with potential improvement in a few cases with complications due to annular sizing errors, but potential worsening due to improper size selection in a much larger proportion of patients.
Existing data on supra-annular measurement and sizing are scarce and conflicting, and the optimal sizing methodology in BAV remains a matter of debate. Only a few reports have demonstrated the feasibility of supra-annular sizing with measurement of a smaller ICD that would lead to the selection of a smaller prosthesis size, but these studies were limited by small sample sizes and confounding factors14,15. Another shortcoming of supra-annular sizing is that there is no standard of how to perform the measurement. The ICD is commonly determined 4 to 5 mm above the annular plane, where implanted THVs have been shown to be mostly constrained, but there are also reports of circumscribing the border of the leaflets which would more or less correspond to the aortic valve area and therefore will commonly be smaller than annular dimensions16. Furthermore, it remains unclear in which phase of the cardiac cycle the ICD should be measured.
ANNULUS AND INTERCOMMISSURAL DISTANCE
In the present cohort, ICDmax was similar overall to Annmax, in contrast to previous studies in which the ICD was smaller than annulus dimensions14,15. This may be explained by cyclic variations of the ICD that we observed in the present analysis, but which in most previous studies were not taken into consideration systematically. In a series by Jilaihawi et al, systolic reconstructions were available for the determination of the ICD, but their proportion was not further specified17. Conversely, in the present study systolic and diastolic reconstructions were available in the vast majority, thus we noted a difference between ICD and Ann only when considering diastolic reconstructions (ICDdia, Anndia), whereas ICD and Ann were similar when using systolic images (ICDsys, Annsys) or the respective maximum values (ICDmax, Annmax). These cyclic differences of the ICD should be taken into consideration for future studies on supra-annular sizing.
In addition, the ICD varied depending on the BAV subtype, showing larger values in bicommissural phenotypes and smaller values in tricommissural phenotypes (Figure 4), which is consistent with previous reports17.
ANNULAR AND SUPRA-ANNULAR SIZING
Using stringent criteria, we identified only a few cases with primarily sizing-related complications (Supplementary Table 2); hence, annular sizing was deemed to be appropriate in >95% of cases. On the other hand, supra-annular sizing in approximately 40% would have led to a divergent sizing strategy, with presumably improved size selection in only a few cases and conceivably improper size selection in a much larger proportion of patients (Figure 5). As supra-annular sizing was only hypothetical and we were not able to determine if and how a divergent size selection would have affected procedural outcomes, our observations are at best hypothesis-generating. Nonetheless, it is unlikely that two different sizes of a prosthesis could be implanted in the same patient with similarly good results. Even though we cannot prove superiority of annular sizing over supra-annular sizing, our results demonstrate that annular sizing is feasible and safe for TAVI in BAV, questioning the need for an alternative sizing approach. A recent registry on THV sizing in BAV demonstrated the feasibility of annular sizing in 88% of cases, whereas it was recommended to integrate supra-annular sizing only in borderline situations5.
Supra-annular sizing and high positioning of the prosthesis in BAV, as promoted by some TAVI operators, appears intuitive and could be useful in certain scenarios, but it is unclear how to select those patients who would benefit from supra-annular sizing. An unselected implementation of this alternative sizing approach in routine clinical practice does not seem to be justified, as the potentially detrimental effects could outweigh the benefits. Importantly, the underlying aortic root shape does not necessarily allow prediction of whether supra-annular sizing would be beneficial over annular sizing, for instance by systematic downsizing in cases with a trapezoid-shaped aortic root, as one would assume.
Limitations
This is a retrospective analysis with its inherent limitations as mentioned above. The variety of different THVs that were implanted may have had an impact on the divergent size selection when employing supra-annular sizing, as sizing charts vary with respect to the covered annulus range, available sizes, and overlapping of valve sizes. Assessment of PVL by means of echocardiography was not core lab-adjudicated and was performed without distinction between transvalvular and paravalvular regurgitation, although the proportion of transvalvular regurgitation is usually small18.
Conclusions
Annular sizing for TAVI in bicuspid aortic valves is feasible and safe and is associated with good outcomes, in particular with the use of new-generation devices. Our results suggest that an incremental benefit due to an altered sizing regimen seems unlikely.
|
Impact on daily practice Annular sizing should be considered the default approach for TAVI in patients with bicuspid aortic valve, whereas our results do not support the additional or even exclusive implementation of supra-annular sizing in this subset. |
Acknowledgements
We thank Elizabeth Martinson, PhD, from the KHFI Editorial Office for her editorial assistance.
Conflict of interest statement
W.K. Kim reports receiving proctor fees and/or lecture honoraria from Boston Scientific, Abbott, Edwards Lifesciences, and Medtronic. C. Liebetrau reports receiving lecture honoraria from Abbott, AstraZeneca, Bayer, Berlin-Chemie, Boehringer Ingelheim, Daiichi Sankyo, and Pfizer – Bristol-Myers Squibb, and meeting expenses from Bayer, and Daiichi Sankyo. M. Renker reports receiving lecture honoraria from Abbott. A. Rolf reports receiving lecture honoraria from AstraZeneca, Boehringer, Pfizer, MSD, and Bristol-Myers Squibb. M. Doss reports receiving proctor fees and/or lecture honoraria from Boston Scientific, and Abbott. C. Hamm reports being on the advisory board of Medtronic. H. Möllmann reports receiving proctor fees and/or speaker honoraria from Abbott, Biotronik, Boston Scientific, and Edwards Lifesciences. The other authors have no conflicts of interest to declare.