Abstract
Bicuspid aortic stenosis (AS) is not rare in patients treated with transcatheter aortic valve implantation (TAVI). Bicuspid valves have unique anatomy which could affect the results of TAVI; however, multiple recent reports have shown that TAVI is safe and effective in this population. Paravalvular aortic regurgitation was initially found to be more frequent in bicuspid patients, but newer-generation devices have shown superior results in this respect. Higher rates of pacemaker implantation after TAVI in bicuspid AS do require further investigation. Current data suggest that bicuspid valves should not be a contraindication for TAVI, but future specific trials are needed to support this assertion.
Introduction
Bicuspid aortic valve is a common congenital defect which most often presents in young adults, but also arises in elderly patients. Bicuspid aortic valves may develop stenosis or regurgitation, which is often associated with dilation of the aorta1. Patients requiring aortic valve replacement for aortic stenosis (AS) at a younger age (lower than 60 years) more frequently have a congenital bicuspid valve. However, the proportion of elderly patients (even octogenarians) who require treatment for AS and have a congenital bicuspid valve is substantial, and may be as high as 20%2.
Owing to their younger age, lower surgical risk and unique anatomy, patients with bicuspid valves have been excluded from all major trials evaluating outcomes of transcatheter aortic valve implantation (TAVI) against surgical aortic valve replacement (SAVR)3-5. Consequently, our knowledge concerning the efficacy and safety of treating bicuspid AS patients with TAVI is largely based on observational reports, most of which utilised early-generation valves6-8.
Bicuspid anatomy
With increased use of high-resolution computed tomography (CT), our understanding of bicuspid AS in elderly patients has grown. CT enables diagnosis of the condition in many patients for whom standard echocardiographic imaging may be limited. CT can also help delineate the similarities and differences in valvular and annular anatomy between patients with bicuspid and tricuspid aortic valves in TAVI populations. In a study comparing CT scans of bicuspid (n=200) and tricuspid (n=200) patients, Philip and colleagues9 found that the aortic annulus was (surprisingly) less elliptical in bicuspid than tricuspid valves (ellipticity index 1.24 vs. 1.29). This study also found that annular area was larger (5.21 vs. 4.63 cm2) and eccentric calcification more common in bicuspid patients. Other studies have shown similar results, whereby the annulus tended to be slightly larger but less or similarly elliptical10-12. The annular dimensions reported in recent large series of bicuspid patients do not exceed the sizes commonly treated using commercially available TAVI devices6,10,13. An example of a typical bicuspid valve, before and after TAVI, can be seen in Figure 1.
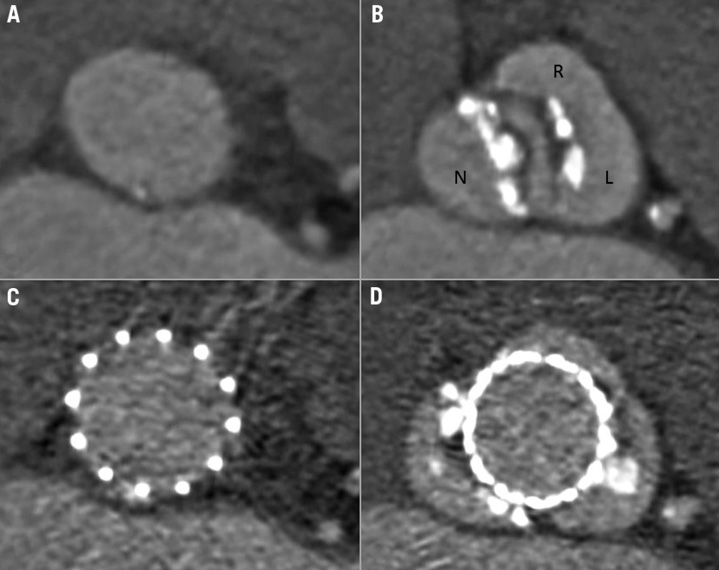
Figure 1. Bicuspid aortic valve before and after TAVI. The annulus of a Sievers type 1 right-left bicuspid valve with aortic stenosis before and after TAVI using a SAPIEN 3 TAVI device. A) Bicuspid annulus with annular area of 4.65 cm2 (long axis 27.3 mm, short axis 21.7 mm, ellipticity index 1.26). B) The same valve showing the enlarged non-coronary cusp (N) and the smaller connected right (R) and left (L) cusps. C) Circular expansion of a SAPIEN 3 TAVI device at annular level. D) Circular TAVI device expansion at leaflet level.
Congenital bicuspid valve morphology (which can be readily identified by CT) is commonly described according to the classification proposed by Sievers and Schmidtke14, which categorises three main types of bicuspid valve (Types 0, 1, 2) according to the number of seam-like raphes connecting the leaflets. The frequency of various morphologies of bicuspid valve appears to be influenced by ethnicity. Whereas Type 1 morphology exceeds 50% of the patients in most published series from western countries, Type 0 morphology was more common in a recent report from China11.
Procedural considerations
Selection of an appropriately sized TAVI device in bicuspid AS is therefore similar to tricuspid AS, since both are based on annular properties15. Device deployment is, on the other hand, more complex, as the angiographic appearance of the cusps is irregular and asymmetric, which can potentially lead to malpositioning, paravalvular regurgitation, and increased rates of pacemaker implantation post TAVI (Figure 2). This is most evident in Type 0 bicuspid valves where only two cusps exist and the classic orthogonal view of a tricuspid valve does not exist.
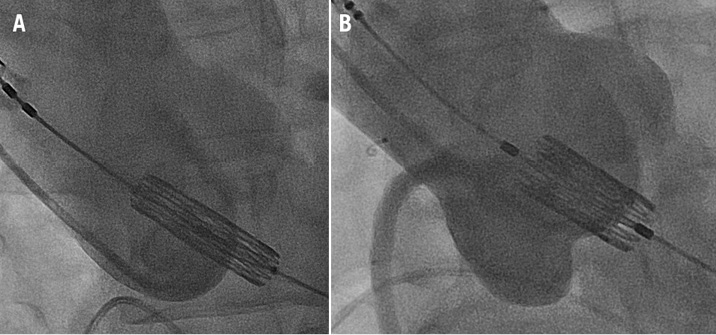
Figure 2. Aortic root angiograms during TAVI device positioning in bicuspid and tricuspid aortic valves. A) Positioning of a SAPIEN 3 TAVI device in the aortic root of a patient with Type 1 (right-left) bicuspid AS. The injecting catheter is in the enlarged non-coronary cusp while the right and left cusps are overlapping and ill-defined. In this case, the TAVI device was implanted successfully and post-deployment imaging confirmed that the view was orthogonal to the annular plane. B) Positioning of a SAPIEN XT TAVI device in the aortic root of a patient with tricuspid AS. The typical orthogonal view shows three symmetrical evenly spaced cusps.
Bicuspid valve anatomy may also have effects on TAVI device expansion. A report evaluating 15 patients treated with a self-expanding device showed non-circular expansion at the annular level16. In this report, non-circularity appeared less common when the TAVI device was implanted deeper below the annular level. Another report of 21 patients, some of whom had post-procedural CTs, reported elliptical expansion of implanted TAVI devices in a number of patients. Non-circular expansion was possibly more common with self-expanding valves10, perhaps as a result of the irregular shape and forces exerted on the expanding TAVI device in a bicuspid orifice. There is also evidence of asymmetric longitudinal expansion of a new-generation balloon-expandable valve13, but information on the degree of expansion at the level of the annulus in balloon-expandable devices is still lacking. Despite this limited information, the midterm results of valve function have not shown suboptimal leaflet function in bicuspid patients as assessed at follow-up echocardiography.
Outcomes
Paravalvular aortic regurgitation (AR) has been shown to be more frequent after TAVI in patients with bicuspid AS6-8,10,12, presumably as a result of inadequate sealing caused by heavy leaflet calcification, irregular distribution of calcium nodules on the leaflets, and resistance to uniform expansion of the device inflow. To date, there are no published data analysing the causes of this phenomenon in bicuspid valves. However, there have been recent reports of improved results with newer-generation devices which feature an external sealing skirt, supporting the hypothesis that AR is caused by an irregular sealing border. Use of the SAPIEN 3 TAVI device (Edwards Lifesciences, Irvine, CA, USA) was associated with no cases of greater than mild paravalvular AR in a multicentre series of 51 patients13. Similarly, there are reports of successful treatment of bicuspid AS using the Lotus™ device (Boston Scientific, Marlborough, MA, USA)17, which also has an external sealing layer.
Pacemaker implantation after TAVI appears to be more frequent in patients with bicuspid AS, and recent large series have reported a new pacemaker rate of 17-29%6-8,13,18. Arguably, there are no direct comparisons with tricuspid patients and most reports utilised earlier-generation devices, but nonetheless this finding is concerning. The higher rate of pacemaker implantation may be associated with difficulty in achieving exact implantation heights as a result of the irregular shape of the leaflets on fluoroscopy. This may result in lower implantation which is known to be associated with increased pacemaker rates. The depth of implantation was assessed in patients undergoing treatment using the SAPIEN 3 TAVI device. Pacemaker rates were significantly higher in patients with lower implantation (extending 8 mm below the level of the annulus)13. Given that the most common type of bicuspid valve is Type 1 (right-left fusion), it has been suggested that this anatomical pattern may exert greater forces directed towards the membranous septum and the conduction system, resulting in higher need for a new pacemaker19. Patients with bicuspid AS are younger and at lower risk (mainly in the surgical AVR cohorts). As TAVI moves into lower-risk populations, the need to avoid a pacemaker as a complication of TAVI appears to be more important.
Patients with bicuspid AS currently treated with TAVI seem to have similar baseline characteristics to typical TAVI patients with tricuspid AS. The German TAVI registry18 found no difference in age or surgical risk (assessed by logistic EuroSCORE) when comparing bicuspid to tricuspid AS patients. Other reports of bicuspid patients have also encompassed elderly patients with increased surgical risks similar to the comparison group of tricuspid patients8,10. In the light of the similar baseline characteristics, it seems that bicuspid AS patients have been served well when treated with TAVI to date. Overall 30-day mortality rates of bicuspid patients in large reports have ranged from 3.9-11%. Other major complications (stroke, vascular injury, major bleeding and aortic injury) do not appear to be higher in this subgroup. Whilst higher rates of moderate or more AR might translate into increased long-term mortality, this risk is likely to be mitigated substantially by the advent of newer TAVI devices.
Future directions
Specific trials evaluating bicuspid AS patients are on the way and will be essential to evaluate the safety and efficacy of TAVI in this important subgroup. Only carefully planned prospective trials will put to rest the valid concerns as to whether TAVI can be an effective and durable therapy for patients with bicuspid AS. As TAVI is offered to younger and lower-risk patients, the proportion of those with bicuspid AS being treated is likely to rise. Our understanding of this group will therefore become of paramount importance.
Conflict of interest statement
The authors have no conflicts of interest to declare.

