Abstract
Prosthesis-patient mismatch (PPM) is frequent following surgical aortic valve replacement (SAVR) and is associated with an increased risk of morbidity and mortality. Preventive strategies to avoid or minimise PPM should be implemented in patients who are at high risk (i.e., patients with a small aortic annulus or those undergoing a valve-in-valve procedure within a small surgical bioprosthesis) and/or vulnerable to PPM (i.e., depressed left ventricular [LV] systolic function, severe LV hypertrophy, concomitant mitral regurgitation, and paradoxical low-flow, low-gradient aortic stenosis). Recent studies suggest that transcatheter aortic valve replacement (TAVR) may be superior to SAVR for the prevention of PPM and associated adverse cardiac events, particularly in the subset of patients with a small (<21 mm) aortic annulus. However, further randomised studies are needed to confirm the potential superiority of TAVR for this purpose.
Introduction
PPM occurs when the effective orifice area (EOA) of a normally functioning prosthesis is too small in relation to the patient’s body size, resulting in abnormally high postoperative gradients. Moderate PPM (indexed EOA <0.85 cm2/m2) is quite frequent (20-70%) following SAVR, whereas the prevalence of severe PPM (indexed EOA <0.65 cm2/m2) ranges from 2-20%1. PPM, and especially severe PPM, is associated with increased risk of operative mortality and adverse cardiac events, less symptomatic improvement, regression of LV hypertrophy and recovery of coronary flow reserve, and reduced long-term survival1. A meta-analysis including 34 studies of 27,186 patients demonstrated that both moderate and severe PPM increased all-cause (hazard ratio [HR]: 1.19 for moderate PPM and 1.84 for severe PPM) and cardiac-related mortality (HR: 1.32 for moderate and 6.46 for severe PPM)2. It is thus important to prevent PPM (and especially severe PPM) in patients undergoing aortic valve replacement (AVR). However, the preventive strategy should be individualised according to baseline clinical characteristics, the estimated risk of PPM, and the anticipated risk of the AVR procedure.
Patient selection
PATIENTS AT RISK OF PPM
Patients with a small aortic annulus (<21 mm) are definitely at higher risk of PPM following SAVR (Figure 1)1. Prior to SAVR, it is possible to estimate the risk of PPM by knowing the aortic annular diameter (which determines the size of prosthesis that can be implanted) and the patient’s body surface area (which determines cardiac output requirements). With this information, one can calculate the predicted indexed EOA (normal EOA reference value for the model and size of prosthesis being implanted divided by the body surface area). Values of <0.85 cm²/m² or 0.65 cm2/m2 identify the risk of moderate or severe PPM, respectively. However, the indexation of EOA to body surface area may overestimate the presence and severity of PPM in obese patients (body mass index >30 kg/m2). In these patients, the VARC-2 consensus document3 recommends using lower cut-point values of indexed EOA to identify or predict PPM: <0.70 cm2/m2 for moderate PPM and <0.60 cm2/m2 for severe PPM.
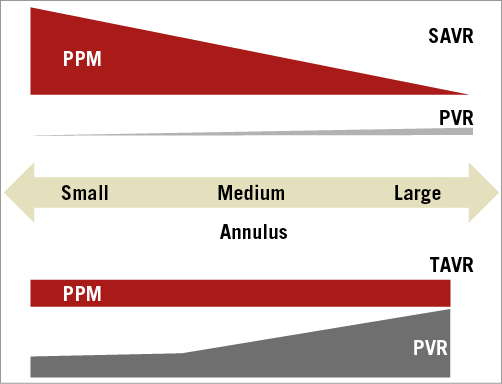
Figure 1. Schematic representation of the risk of prosthesis-patient mismatch and paravalvular regurgitation following TAVR and SAVR according to aortic annular size. PPM: prosthesis-patient mismatch; PVR: paravalvular regurgitation; SAVR: surgical aortic valve replacement; TAVR: transcatheter aortic valve replacement
FACTORS INDICATING VULNERABILITY TO PPM
The impact of PPM is not equivalent in all patients, thereby underlining the importance of individualised preventive strategies (Figure 2). PPM is indeed relatively well tolerated in elderly, sedentary patients with preserved LV function, whereas it has a highly detrimental impact on survival and quality of life in younger (<70 years) patients, as well as in those with impaired LV systolic function (ejection fraction <50%), severe LV hypertrophy, concomitant mitral regurgitation, and/or paradoxical low-flow, low-gradient aortic stenosis2,4,5. Younger physically active patients have higher metabolic demand and cardiac output requirements and are thus more susceptible to the negative impact of PPM on their longevity and quality of life. The subset of patients most vulnerable to PPM is probably the one with pre-existing impairment of LV systolic function4,5, consistent with the concept that increased LV afterload caused by PPM is less well tolerated by a poorly functioning ventricle. A second vulnerable subset of patients is the one with concomitant mitral regurgitation where the patients undergo isolated AVR (with no concomitant mitral valve procedure), since residual LV afterload related to PPM may hinder regression of mitral regurgitation following AVR.
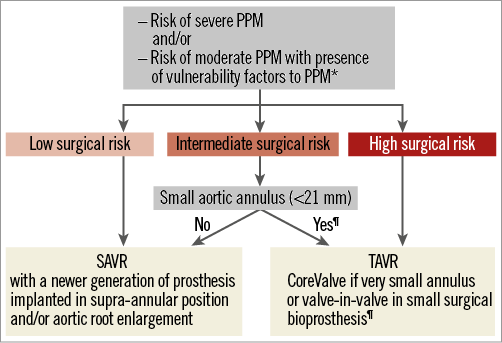
Figure 2. Algorithm for patient and procedure selection for the prevention of prosthesis-patient mismatch. * Impaired LV systolic function, severe LV hypertrophy, concomitant mitral regurgitation, paradoxical low-flow, low-gradient aortic stenosis. ¶This proposed strategy is based on limited data and will need to be validated by further studies in larger series. PPM: prosthesis-patient mismatch; PVR: paravalvular regurgitation; SAVR: surgical aortic valve replacement; TAVR: transcatheter aortic valve replacement
In summary, preventive strategies to avoid or minimise PPM should be considered in patients who are at high risk (i.e., patients with small aortic annulus) and/or vulnerable to PPM (i.e., younger age, impaired LV systolic function, severe LV hypertrophy, concomitant mitral regurgitation, and paradoxical low-flow, low-gradient aortic stenosis).
Procedure selection
The cardiac surgeon is confronted with a dilemma in attempting to prevent PPM since, on the one hand, avoidance of PPM is crucial (especially in vulnerable patient subsets) whilst, on the other hand, alternative procedures to prevent PPM (e.g., aortic root enlargement or implantation of a stentless bioprosthesis) increase the complexity, duration and operative risk of SAVR.
TAVR has emerged as a valuable alternative to SAVR in patients with high or extreme surgical risk. Some recent studies suggest that it may be equivalent to SAVR in low/intermediate-risk cohorts6. The incidence of moderate and severe PPM reported in TAVR series was 15-45% and 2-20%, respectively7-11. Furthermore, PPM was associated with less functional improvement, regression of LV mass and diastolic dysfunction, and reduced survival10,11.
Randomised studies indicate that TAVR is associated with less PPM than SAVR11,12. In Cohort A of the PARTNER I trial, PPM was more frequent (60% versus 47%) and more often severe (28% versus 20%) after SAVR than after TAVR11. The differing incidence of PPM between SAVR and TAVR was even more pronounced (65% vs. 40%) in the subgroup of patients with a small aortic annular diameter (<21 mm). In contrast to SAVR, the presence of a small aortic annulus does not appear to be a major risk factor for PPM following TAVR (Figure 1)13. Furthermore, patients with a small annulus have a lower risk of paravalvular regurgitation following TAVR than those with a larger annulus11,13 (Figure 1). This may explain why patients in PARTNER I Cohort A with a small aortic annulus undergoing TAVR demonstrated improved survival compared with SAVR, whereas the opposite trend was observed (improved survival after SAVR compared with TAVR) in those with a large annulus13. Figure 2 proposes an algorithm for the selection of AVR procedure according to: i) the estimated risk of PPM, ii) the presence of factors predicting vulnerability to PPM, iii) the predicted surgical risk, and iv) the aortic annular size. In patients at risk of PPM, TAVR may be preferable to SAVR in those with high surgical risk and those with intermediate surgical risk and a small aortic annulus.
In summary, these data suggest that TAVR may be superior to SAVR for the prevention of PPM and its associated adverse cardiac events in the subset of patients with a small (<21 mm) aortic annulus. Further randomised studies are now needed to confirm the potential superiority of TAVR in this subset.
Device selection
Some studies (including one randomised study) have suggested that the self-expanding CoreValve® (Medtronic, Minneapolis, MN, USA) is associated with less PPM but more paravalvular regurgitation than balloon-expandable SAPIEN valves (Edwards Lifesciences, Irvine, CA, USA)14,15. Some studies have also reported that patients undergoing a valve-in-valve procedure within small (≤21 mm) surgical bioprostheses have a very high risk of severe PPM16. Use of the CoreValve in such patients may yield better haemodynamic results and less PPM compared with balloon-expandable valves (conceivably due to the supra-annular position of the CoreValve leaflets).
Conclusion
In patients undergoing AVR, preventive strategies should be implemented in those at risk of severe PPM and/or with factors predicting vulnerability to PPM. TAVR offers a valuable alternative to SAVR to prevent PPM in the subset of patients with a small aortic annulus.
Funding
P. Pibarot holds the Canada Research Chair in Valvular Heart Disease and his research programme is funded by the Canadian Institutes of Health Research (Ottawa, Ontario, Canada).
Conflict of interest statement
P. Pibarot has received research support from Edwards Lifesciences for echocardiographic core laboratory analyses of transcatheter valves. The other authors have no conflicts of interest to declare.

