Abstract
Background: In patients with complex coronary bifurcation lesions undergoing percutaneous coronary intervention (PCI), various 2-stent techniques might be utilised. The Visible Heart Laboratories (VHL) offer an experimental environment where PCI results can be assessed by multimodality imaging.
Aims: We aimed to assess the post-PCI stent configuration achieved by 2-stent techniques in the VHL and to evaluate the procedural factors associated with suboptimal results.
Methods: Bifurcation PCI with 2-stent techniques, performed by expert operators in the VHL on explanted beating swine hearts, was studied. The adopted bifurcation PCI strategy and the specific procedural steps applied in each procedure were classified according to Main, Across, Distal, Side (MADS)-2 and to their adherence to the European Bifurcation Club (EBC) recommendations. Microcomputed tomography (micro-CT) was used to assess the post-PCI stent configuration. The primary endpoint was “suboptimal stent implantation”, defined as a composite of stent underexpansion (<90%), side branch ostial area stenosis >50% and the gap between stents.
Results: A total of 82 PCI with bifurcation stenting were assessed, comprised of 29 crush, 25 culotte, 28 T/T and small protrusion (TAP) techniques. Suboptimal stent implantation was observed in as many as 53.7% of the cases, regardless of baseline anatomy or the stenting strategy. However, less frequent use of the proximal optimisation technique (POT; p=0.015) and kissing balloon inflations (KBI; p=0.027) and no adherence to EBC recommendations (p=0.004, p multivariate=0.006) were significantly associated with the primary endpoint.
Conclusions: Commonly practised bifurcation 2-stent techniques may result in imperfect stent configurations. More frequent use of POT/KBI and adherence to expert recommendations might reduce the occurrence of post-PCI suboptimal stent configurations.
Introduction
The improvement of percutaneous coronary intervention (PCI) for coronary bifurcation lesions (CBL) is a hot topic in interventional cardiology1. The implantation of 1 drug-eluting stent (DES) in the main vessel (MV) represents the gold standard for unselected CBL, while 2-stent techniques − the implantation of DES in both the MV and the side branch (SB) − are often needed to treat complex bifurcation lesions23. Of note, a variety of 2-stent techniques have been described, and various sequences of the procedural steps can be adopted for their implantation45, potentially affecting the final stent configuration achieved5. Thus, the assessment of bifurcation stenting techniques in experimental settings might help to identify the most valuable technical sequences6. For such scenarios, the Visible Heart Laboratories (VHL) provides an experimental environment where bifurcation stenting techniques can be practised in a setting similar to a clinical one and evaluated using unique multimodal imaging modalities789. In the present study, we assessed the post-PCI stent configuration achieved by 2-stent techniques practised in the VHL and evaluated the procedural factors associated with suboptimal results.
Methods
The aim of the MultimOdality two-stent Bifurcation techniques comparison in a BEating heart Model (MOBBEM) study was to assess, through microcomputed tomography (micro-CT), the procedural results obtained by expert operators practising different 2-stent bifurcation techniques in an explanted beating heart model and to identify the procedural predictors of suboptimal stent implantation.
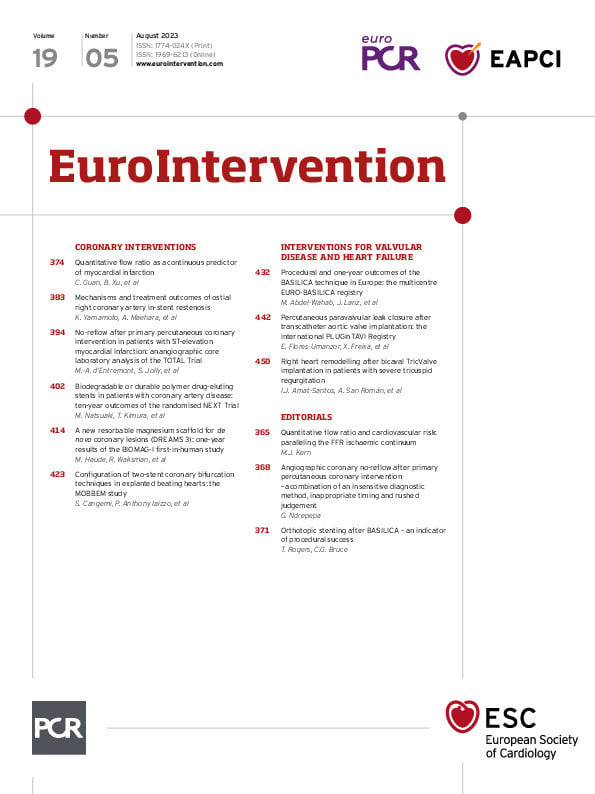
Visible Heart Laboratories methodologies
The study was conducted at the Visible Heart Laboratories (VHL; University of Minnesota, Minneapolis, MN, USA). VHL performs experimental research in which harvested porcine and human hearts are reanimated and attached to supporting equipment that permits them to beat outside the body for 6-8 h, thus, providing enough time to perform bifurcation PCI789. In the present study, adult healthy swine (70-95 kg) were anaesthetised and intubated, then, after exposition of the heart through a medial sternotomy, cardioplegia was delivered via aortic root cannulae. The heart was then explanted, and all major vessels were cannulated and connected to an ex vivo Visible Heart apparatus1011. Subsequently, each heart was warmed and perfused with a Krebs-Henseleit buffer and then defibrillated with an ~30 J shock to induce a sinus rhythm. Next, bifurcation PCI was performed on the reanimated hearts under multimodality imaging guidance with standard fluoroscopy (OEC Elite Fluoroscopy). Intracoronary angioscopy was performed in parallel, using 2.4 and 4.0 mm fiberscopes (Olympus Corporation) placed immediately proximal to the bifurcation to allow direct intracoronary visualisation of each procedural step. After ex vivo stenting procedures were performed on a given study day, each heart was then fixed in an end-diastolic state using a formalin fixation chamber in order to keep the coronaries patent and to allow for the subsequent micro-CT scanning. Experiments were executed in accordance with the most recent recommendations of the “Guide for the Care and Use of Laboratory Animals”12, and the animal research protocol used in this laboratory was reviewed and approved by the University of Minnesota Institutional Animal Care and Use Committee.
PCI in coronary bifurcations
Expert interventional cardiologists from all over the world were invited to the VHL and performed the procedures under the guidance of standard fluoroscopy (OEC Elite Fluoroscopy). Commercially available guiding catheters, guidewires (Cougar/Thunder/Zinger; Medtronic), balloons (Euphora and Euphora NC; Medtronic) and DES (Resolute Onyx and Resolute Integrity; Medtronic) were used.
The exclusion criteria were 1) intended bifurcation stenting technique other than crush, culotte, or T/T and small protusion (TAP); and 2) the absence of complete video recordings allowing a reconstruction of the sequence of interventions performed during the procedure.
Multimodal imaging
During the procedure, intracoronary angioscopy, using 2.4 and 4.0 mm fiberscopes (Olympus Corporation), was placed proximal to the bifurcation in order to allow direct intracoronary visualisation of each procedural step. In parallel, a multichannel digital recording system continuously registered heart function and operator technique. After the stenting procedures, the hearts were fixed using a formalin fixation chamber9, which preserved them in an end-diastolic state, keeping the coronaries well dilated. After fixation, the hearts were scanned with an X3000 micro-CT scanner (North Star Imaging) that allowed for computational stent reconstructions with approximately 20-micron resolution. From these scans, the resulting stent(s) and anatomies were three-dimensionally (3D) reconstructed, segmented, and rendered using medical imaging software (Mimics; Materialise).
Two-stent technique assessment
Two-stent techniques were practised according to the individual discretion of different interventional cardiologists. For the present study, all procedural images (angioscopy, video camera recordings) were reviewed by a trained interventional cardiologist in order to establish the intended bifurcation stenting technique and ensure that the specific sequence of ballooning steps applied were classified according to the Main, Across, Distal, Side (MADS)-2 classification5. In particular, the following data were collected for each PCI performed:
− anatomical data, including type of vessels involved (left main bifurcation, left anterior descending artery-first diagonal, circumflex artery-left marginal artery, right coronary artery-acute marginal artery/posterior descending artery), angles of the bifurcations and diameters of the vessels;
− the number, dimensions and type of balloons and stents used;
− the planned stenting technique that included the following families of commonly adopted 2-stent techniques: crush, culotte, T/TAP;
− the type and number of bifurcation-specific ballooning steps adopted during the procedure, including proximal optimisation technique (POT), kissing balloon inflation (KBI) or isolated side branch dilation.
Double-stenting techniques performed in this study were as follows:
− T/TAP: stenting of the “operative” main vessel and distal rewiring of the jailed branch13, followed by ballooning and the implantation of the second stent in the SB aiming to cover its ostium (and in case of TAP, accepting the creation of a possible small neocarina, with a balloon ready for kissing in the other vessel);
− culotte: overlapping stents in the proximal MV from either SB and distal MV stents, regardless of the length of stent overlap and the order of first stent implantation (SB or distal MV);
− crush: the first stent was deployed in the SB, protruding into the MV, followed by its crush using an MV balloon.
While the stent implantation phases was used to classify the procedures into the three groups, the sequence of ballooning steps were used to divide the procedures into those following EBC best practice recommendations, or not35. In particular, procedures were considered to adhere to EBC recommendations when the following steps for each of the 2-stent techniques were applied:
− T/TAP: MV stent-POT-KBI-SB stent-POT-KBI (T/TAP on top of provisional with final POT only in the case of sufficient space that does not reach the carina);
− culotte: first stent-POT-KBI-second stent-POT-KBI-POT (i.e., culotte with triple POT and double KBI);
− crush: SB stent-POT-KBI-MV stent-POT-KBI-POT (i.e., double kissing [DK]-crush with the crushing balloon size similar to the POT balloon size)
Ballooning steps (including POT and KBI) were performed using non-compliant or semicompliant balloons, according to the operator’s preference.
PROCEDURAL RESULT ASSESSMENT AND PRIMARY STUDY ENDPOINT
For the present study, the postprocedural micro-CT examinations were assessed (blind to the procedural steps applied), focusing on a bifurcation’s region of interest (ROI) that comprised the 5 mm of the MV proximal to the SB take-off, the first 5 mm of the distal MV after the SB take-off and the first 5 mm of the SB (Figure 1). The bifurcation angle was measured analysing the 3D images obtained at postprocedural micro-CT (heart fixed in an end-diastolic state). The quantitative analyses performed in the ROI were focused to detect stent underexpansion, SB ostial area stenosis, and gaps between stents. Underexpansion was defined as a minimal stent area (minimal luminal area in the stented segment) <90% of the reference minimal lumen in the three examined segments (proximal MV, distal MV and SB) (Figure 2A)14. The ostial area free of stent struts was measured from the 3D projection of the SB ostium and defined as the ratio of the area of the largest opened stent cell to the referential SB lumen area15 (Figure 2B). Planimetric ostial area stenosis was defined as the area outside of the largest opened stent cell (referential SB lumen area-the largest opened stent cell lumen area) divided by the referential SB lumen area (Figure 2B). Significant SB ostium stenosis was defined as planimetric ostial area stenosis >50% of the reference. Since the intention of dual stenting techniques is to entirely cover the coronary bifurcation with stent struts, the bifurcation area not covered by stent struts was called the “stent gap”. A significant stent gap was defined as a distance between stent struts >1 mm with a partial (>180°) to circumferential (360°) pattern in the ROI (Figure 2C). The primary endpoint of the study was “suboptimal stent implantation”, defined as a composite endpoint of stent underexpansion (in the proximal or distal MV or SB), SB ostium stenosis and stent gap. The individual components of the primary endpoint constituted the secondary endpoints of the study.
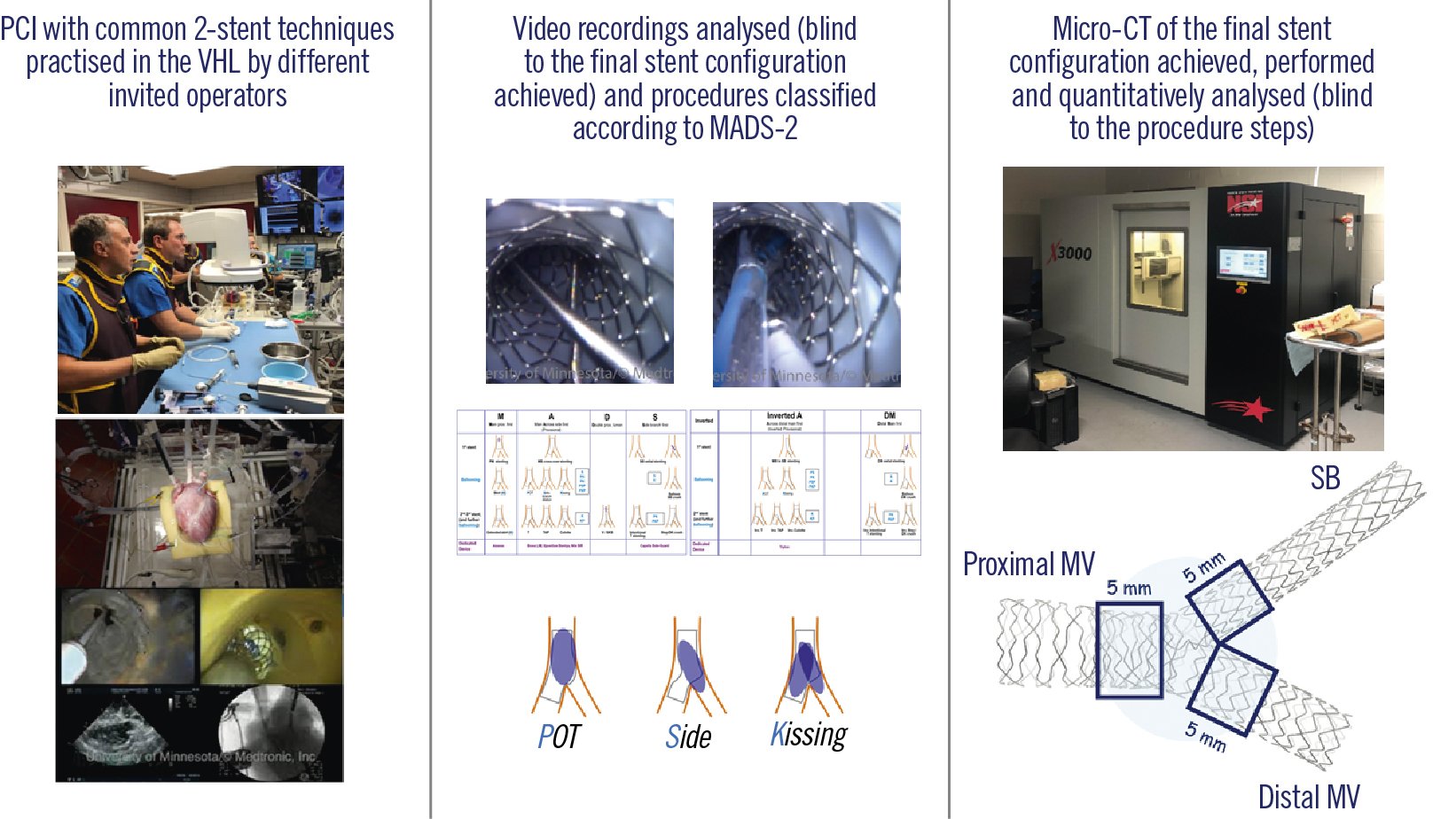
Figure 1. Outline of the study design. MADS: Main, Across, Distal, Side classification; micro-CT: microcomputed tomography; MV: main vessel; PCI: percutaneous coronary intervention; POT: proximal optimisation technique; SB: side branch; VHL: Visible Heart Laboratories
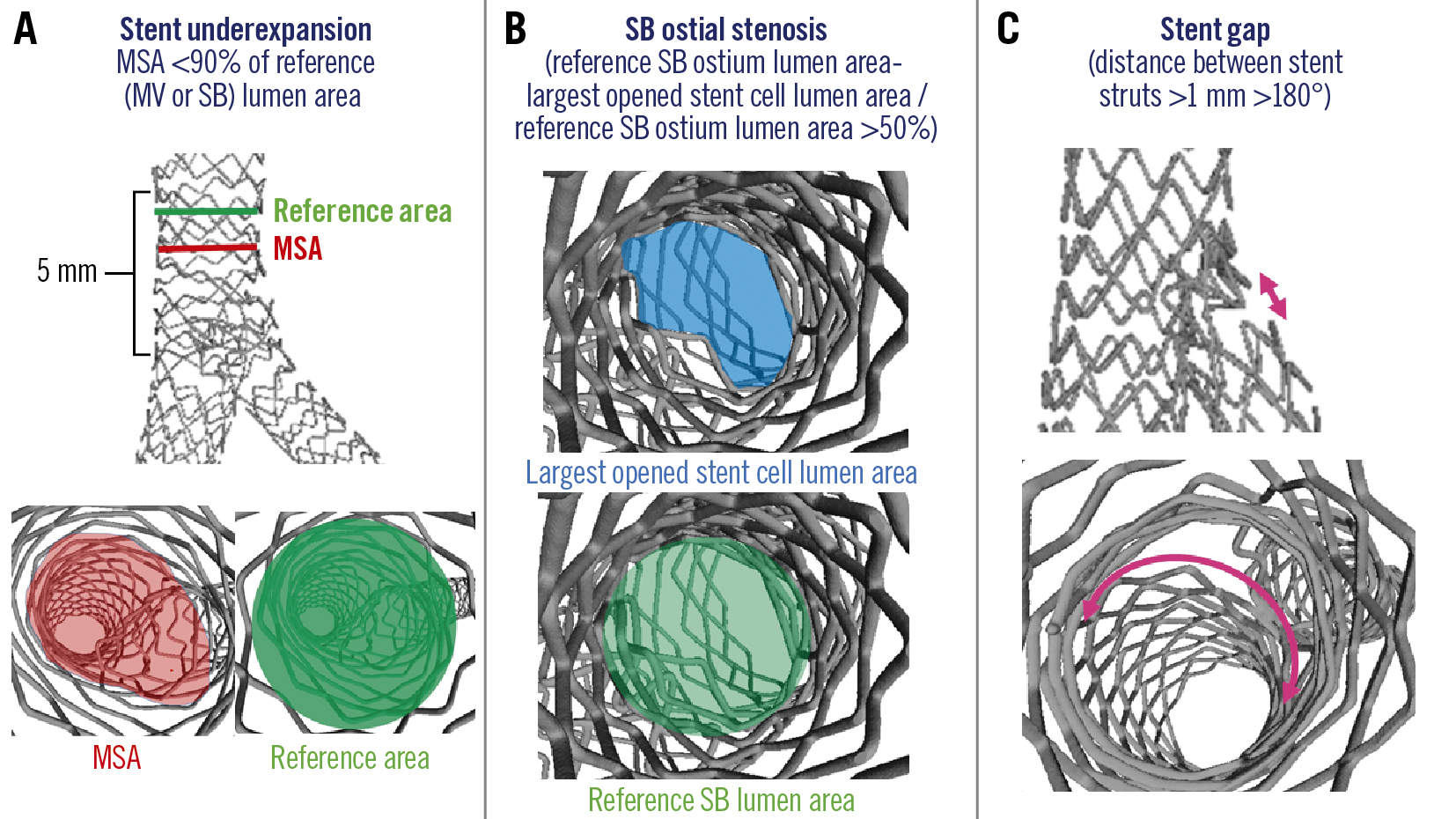
Figure 2. Suboptimal stent implantation features definitions. A) Stent underexpansion. B) SB ostial stenosis. C) Stent gap. MSA: minimum stent area; MV: main vessel; SB: side branch
STATISTICAL ANALYSIS
Continuous variables were reported as means±standard deviation if normally distributed or medians and quartiles otherwise; discrete variables were reported as raw number and percentages. The Student’s t-test, the Mann-Whitney U test, and χ2 tests were used for bivariate analysis, as appropriate. Multivariable logistic regression was used to identify independent predictors of the prespecified study endpoints. Any multivariable regression model included all variables results nominally significant at bivariate association with the endpoint itself. All data analyses were conducted using statistical software SPSS-PASW 23 (IBM), and a two-tailed p-value <0.05 was considered statistically significant for all tests.
Results
Characteristics of treated bifurcations and of bifurcation stenting procedures
Out of 102 consecutive procedures with 2-stent techniques performed in the VHL between 2017 and 2022, a total of 82 bifurcation PCI with planned 2-stent techniques were enrolled in the study (see selection algorithm in Supplementary Figure 1). The characteristics of the treated bifurcations are reported in Table 1. The left anterior descending artery (LAD)-diagonal was the most common bifurcation treated followed by the left circumflex artery (LCx)-obtuse marginal bifurcation. The treated bifurcations were large, with a mean vessel size of 4.0 mm in the proximal MV, 3.4 mm in the distal MV and 2.7 mm in the SB. The crush technique was used in 29 bifurcations (35.4%), the culotte in 25 (30.5%) and T/TAP in 28 (34.1%). The procedural characteristics are reported in detail in Table 2. At least one POT and KBI was performed in each procedure. In the entire study, the average number of POT was 2.0 and the average number of KBI was 1.5, thus reflecting the relevance of these ballooning techniques in common 2-stent technique practice. Overall, 56 procedures (68.3%) were performed using the sequence of ballooning steps recommended by EBC best practices. Of note, adherence to EBC recommendations differed across the different techniques: 14/29 for crush, 18/25 for culotte, and 24/28 for T/TAP (p<0.001).
Table 1. Baseline characteristics.
| Parameters | |
|---|---|
| Number of bifurcations treated | 82 (100) |
| Left main bifurcation | 4 (4.9) |
| LAD-diag | 39 (47.6) |
| LCx-OM1 | 21 (25.6) |
| RCA-acute marg/PDA | 19 (23.2) |
| Proximal bifurcation angle (between proximal MV and SB), ° | 134.7±15.7 |
| Distal bifurcation angle (between distal MV and SB), ° | 55.0±15.8 |
| Distal bifurcation angle <70° | 65 (79.3) |
| Proximal MV reference diameter, mm | 4.0±0.5 |
| Distal MV reference diameter, mm | 3.4±0.4 |
| SB reference diameter, mm | 2.7±0.5 |
| Data are expressed as mean±standard deviation or n (%). diag: diagonal; LAD: left anterior descending artery; LCx: left circumflex artery; marg: marginal; MV: main vessel; OM1: first obtuse marginal artery; PDA: posterior descending artery; RCA: right coronary artery; SB: side branch | |
Table 2. Procedural characteristics.
| Techniques | Value | |
|---|---|---|
| Crush | 29 (35.4) | |
| Culotte | 25 (30.5) | |
| Inverted Culotte | 12 (14.6) | |
| T/TAP | 28 (34.1) | |
| Inverted T/TAP | 1 (1.2) | |
| Stent implanted in the MV | size, mm | 3.5±0.6 |
| length, mm | 21.4±5.9 | |
| Stent implanted in the SB | size, mm | 2.7±0.5 |
| length, mm | 16.9±4.1 | |
| POT characteristics^ | Balloon-to-artery ratio | 1.1±0.6 |
| Atmospheres | 15.0±3.8 | |
| Kissing balloon inflation characteristics^ | MV balloon to distal MV artery ratio | 1.0±0.1 |
| SB balloon to SB artery ratio | 1.0±0.1 | |
| Atmospheres | 13.2±2.3 | |
| Number of isolated SB dilations | 0.9±0.6 | |
| Number of POT(s) | 2.0±0.9 | |
| Number of kissing(s) | 1.5±0.6 | |
| EBC recommendations followed | 56 (68.3) | |
| Data are expressed as mean±standard deviation or n (%). ^in the case of multiple POT or kissing balloon inflations, the reported values are those used in the last inflation. EBC: European Bifurcation Club; MV: main vessel; POT: proximal optimisation techniques; SB: side branch; T/TAP: T/T and small protusion | ||
Suboptimal stent implantation and its predictors
Supplementary Table 1 reports the overall micro-CT postprocedural features observed. The stent configuration achieved after PCI was characterised by the presence of a series of imperfections that are detailed in Table 3. Despite the experimental setting and the absence of atherosclerosis, stent underexpansion was detected in 36.6% of cases, planimetric ostial area stenosis in 15.9% and a stent gap in 13.4%. Therefore, the primary study endpoint of suboptimal stent result was found in as many as 53.7% of the treated bifurcations. The occurrence of suboptimal stent implantation was not significantly different regardless of baseline bifurcation characteristics (Supplementary Table 2) or the intended bifurcation stenting technique (Table 3, Figure 3). However, suboptimal stent expansion was also associated with other adverse stent configuration features, such as longer metallic neocarinas (p=0.001) and higher ellipticity indices at the distal MV (p=0.001). When assessing the procedural predictors of suboptimal stent implantation, in univariate analysis, less frequent use of POT (p=0.013) and KBI (p=0.019) and the absence of adherence to EBC recommendations were the only significant factors (Table 4). In the multivariate analysis, a lack of adherence to EBC recommendations was the only statistically significant predictor of suboptimal stent implantation (odds ratio [OR] 0.225, 95% confidence interval [CI]: 0.078-0.646; p=0.006). Figure 4 shows three examples of micro-CT achieved with the main techniques (crush, culotte and T/TAP), practised according to EBC recommendations, demonstrating successful stent implantation.
Table 3. Study endpoints.
| Postprocedural adverse features | Total | T/TAP (n= 28) | Culotte (n=25) | Crush (n=29) | p-value |
|---|---|---|---|---|---|
| Stent underexpansion (<90%) | 30 (36.6) | 11 (39.3) | 4 (16.0) | 15 (51.7) | 0.023 |
| – Proximal MV underexpansion | 5 (6.1) | 2 (7.1) | 0 | 3 (10.3) | 0.274 |
| – Distal MV underexpansion | 13 (15.9) | 5 (17.8) | 2 (8.0) | 6 (20.7) | 0.417 |
| – Side branch underexpansion | 21 (25.6) | 9 (32.1) | 3 (12.0) | 9 (31.0) | 0.173 |
| SB ostial area stenosis (>50%) | 13 (15.9) | 3 (10.7) | 4 (16.0) | 6 (20.7) | 0.588 |
| Stent gap (>1 mm for >180°) | 11 (13.4) | 5 (17.8) | 4 (16.0) | 2 (6.9) | 0.432 |
| Suboptimal stent result (primary endpoint) | 44 (53.7) | 17 (60.7) | 10 (40.0) | 17 (58.6) | 0.256 |
| Data are expressed as n (%). MV: main vessel; SB: side branch; T/TAP: T/T and small protrusion | |||||
Figure 3. Suboptimal stent implantation. Suboptimal stent implantation according to 2-stent technique (A) and adherence to EBC recommendations during PCI (B). EBC: European Bifurcation Club; PCI: percutaneous coronary intervention; T/TAP: T/T and small protrusion
Table 4. Predictors of suboptimal stent results.
| Technical characteristics | Suboptimal stent result | Optimal stent result | p-value univariate | p-value multivariate |
|---|---|---|---|---|
| Number of POT(s) | 1.8±0.9 | 2.2±0.8 | 0.015 | - |
| Number of kissing balloon inflations | 1.4±0.6 | 1.7±0.5 | 0.027 | - |
| EBC recommendations followed | 24 (42.9) | 32 (57.1) | 0.004 | 0.003 |
| Data are expressed as mean±standard deviation or n (%). EBC: European Bifurcation Club; POT: proximal optimisation technique | ||||
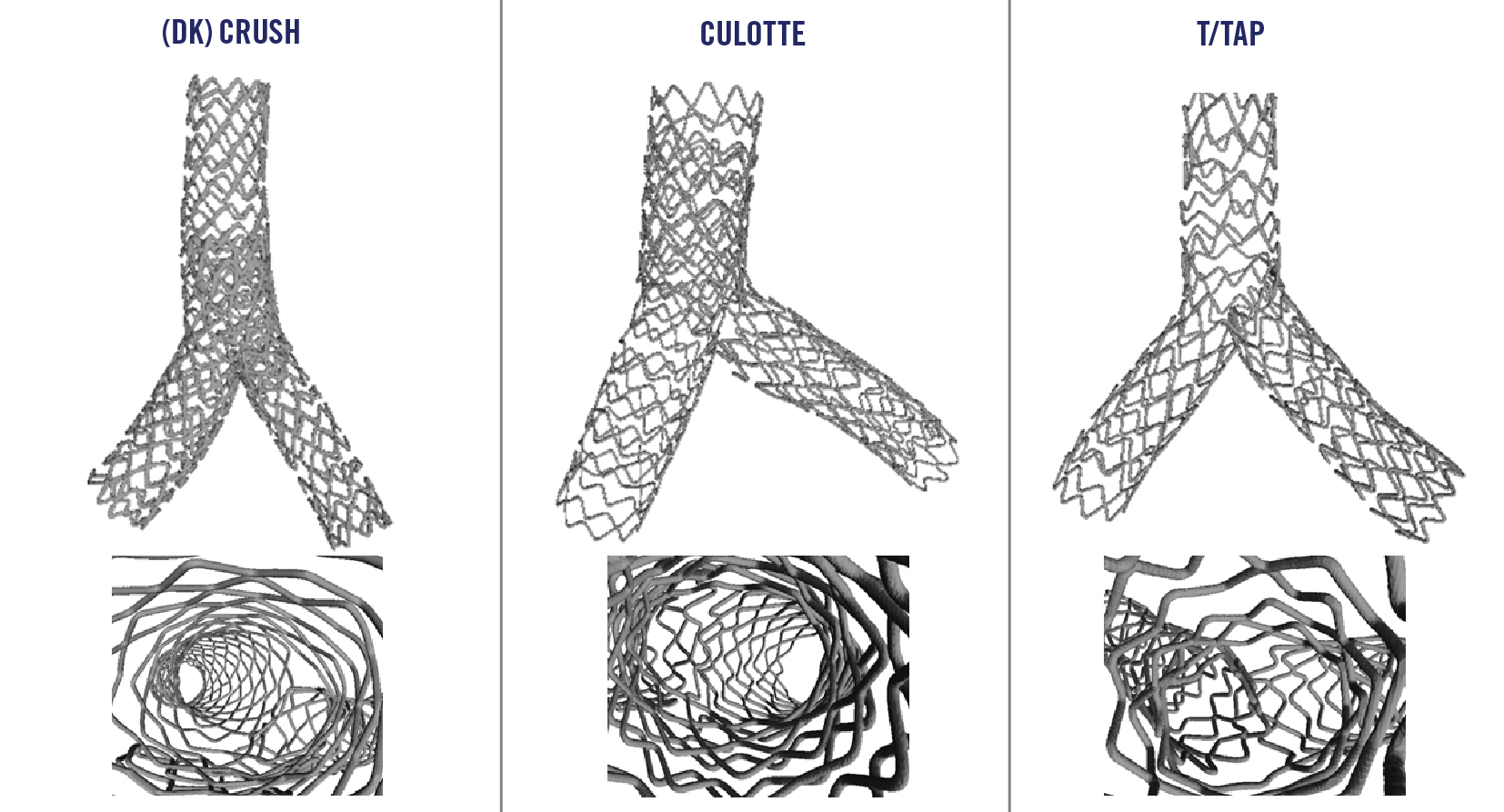
Figure 4. Examples of post-PCI micro-CT obtained with the three different 2-stent techniques conducted according to EBC recommendations. DK: double kissing; EBC: European Bifurcation Club; micro-CT: microcomputed tomography; PCI: percutaneous coronary intervention; T/TAP: T/T and small protrusion
Predictors of secondary endpoints
A series of procedural characteristics were associated with stent underexpansion, including the use of culotte technique (protective factor; p=0.010), the use of crush technique (risk factor; p=0.035), lower incidence of POT (p=0.001), lower incidence of KBI (p=0.030), and lack of adherence to EBC recommendations (p=0.007). In the multivariable analysis, only less frequent use of POT independently predicted the occurrence of stent underexpansion (OR 0.435, 95% CI: 0.220-0.861; p=0.017). Stent gap was significantly influenced by baseline characteristics (more common in the procedures performed in the LCx-OM1 [first obtuse marginal artery] bifurcation; p=0.018; and less common in LAD bifurcations; p=0.006). In the multivariable analysis, only stenting performed in the LCx-OM1 bifurcation independently predicted the occurrence of a stent gap (OR 0.087, 95% CI: 0.011-0.715; p=0.023). Finally, no significant predictor of ostial SB stenosis was recognised.
Discussion
Two-stent techniques are commonly adopted during PCI for coronary bifurcation lesions with high anatomical complexity. Yet, patients receiving 2 stents are known to have an increased risk of late stent thrombosis16 and mortality17. Accordingly, the search for improvements in PCI technique for these patients is ongoing. To this end, the present study conducted in a preclinical, unique, experimental PCI simulation setting showed that:
− the practice of 2-stent techniques are not warranted to achieve the intended stent conformation (considering that, a “suboptimal stent result” is often detected by micro-CT at the procedure’s end);
− the application of (repeated) bifurcation PCI-specific ballooning techniques (namely POT and KBI) is probably more important for successful stent implanation than stenting technique selection;
− a series of recommended sequences for POT and KBI, which have been developed in recent years and are recommended by expert consensus, might enhance the efficacy of popular techniques like crush, culotte and T/TAP.
Within the limits of results stemming from an animal experimental model, these findings provide original, useful insights regarding 2-stent techniques.
Bifurcation PCI is a hot topic in interventional cardiology and preclinical evaluations of stenting techniques may safely generate important insights1. Among the different possible experimental settings, VHL is particularly interesting as it allows operators to practise stenting techniques in an environment almost identical to a clinical one7. The interest generated by this model among bifurcation stenting experts prompted many committed interventional cardiologists to visit the VHL and to practise bifurcation PCI, including 2-stent techniques. Among different imaging modalities available in the VHL9, micro-CT is the highest resolution 3D modality, allowing a precise assessment of post-PCI stent conformation. Thus, we adopted this methodology to search for stent imperfections like underexpansion, uncovered areas and SB ostium obstruction that are undesired in 2-stent techniques but are seldom recognised as causes of clinical failures by intracoronary imaging. The major finding was that 2-stent techniques are associated with a disturbingly high rate of technical imperfections (53.7%), even when performed in healthy coronary artery bifurcations by expert operators. In this field, comparisons between different proposed stenting techniques are often undertaken with the aim of determining which technique has a better clinical performance18. Yet, in the present experimental model where experts practised the techniques they subsequently came to master, imperfect stent implantantion results were not significantly different between the three major families of techniques (crush, culotte and T/TAP), which are often regarded as completely different from an operative point of view. This finding fits with other experimental studies19 and supports the concept of the inherent imperfection shared by 2-stent techniques (all are affected by the need to completely change the DES geometry). Moving from technique selection to the specific modality of its realisation, different operators practise the same techniques using different ballooning steps. For instance, the ballooning steps are recognised to be pivotal for stent deformations needed during bifurcation stenting35. Accordingly, we found that multiple POT and KBI are useful during all 2-stent techniques to achieve the best technical result. In this regard, the sequence of ballooning steps might have a pivotal role. Over the years, the EBC has reviewed available data on technical steps and developed recommendations regarding best practices for popular 2-stent techniques35. Such recommendations comprised the use of multiple POT and KBI and also highlighted sequences for their application that might facilitate the achievement of the optimal result. The value of such recommendations is supported by the present study in which the performance of PCI in accordance with them was significantly associated with reduced occurrence of imperfect stent implantation results. Figure 4 shows micro-CT examples of successful bifurcation techniques that adhered to EBC recommendations. As a final remark, the overall clinical impact of the suboptimal stent configurations found in the present study cannot be established. Indeed, when high resolution imaging is applied in clinical practice, post-PCI imperfections are often seen in successful bifurcation stenting procedures using 1-stent techniques as well20.
Limitations
This preclinical ex vivo model derived from reanimated swine hearts has intrinsic limitations, considering that bifurcation PCI were performed on healthy porcine coronary arteries, characterised by increased elasticity and/or compliance of the vessel wall that might have increased the stress to the stents and emphasised the effects of balloon-induced modifications. Furthermore, balloon and stent placement were monitored using angiography and angioscopy according to the operators’ discretion, but familiarity with angioscopy cannot come from clinical practice so its eventual use during procedural steps might have represented a possible confounder. Finally. this is a retrospective study of prospectively recorded procedures performed without a dedicated research protocol, so the occurrence of unrecognised bias cannot be ruled out.
Conclusions
This study using the unique preclinical environment offered by VHL shows that, despite the absence of atherosclerosis, different 2-stent bifurcation techniques in a beating heart might commonly result in imperfect stent configurations. A higher number of POT/KBI and best practice recommendations might reduce the occurrence of suboptimal stent configurations. These findings might be useful in bifurcation PCI practice and need to be further evaluated in clinical settings.
Impact on daily practice
PCI for complex coronary bifurcation lesions is a clinical challenge and 2-stent techniques requiring multiple steps are often needed. The MOBBEM study evaluated the stent configuration achieved after PCI with 2-stent techniques in explanted beating hearts via micro-CT. Despite a favourable experimental environment for 2-stent techniques (no atherosclerosis, no clinical environment), suboptimal stent implantation was observed in as many as 53.7% of cases and should call maximum attention to the clinical practice of 2-stent techniques. In the study, neither baseline anatomy nor the stenting strategy influenced the occurrence of suboptimal stent implantation. However, less frequent usage of bifurcation PCI-specific ballooning techniques (POT and KBI) was more closely associated with suboptimal stent implantation. Finally, a series of recommended sequences for POT and KBI, developed during the past years and recommended by expert consensus, might enhance the efficacy of popular techniques like crush, culotte and T/TAP.
Funding
This research was supported in part via an educational grant from the University of Minnesota’s Medical School as well as from the Institute for Engineering in Medicine. The work was also supported via a research contract with Medtronic PLC, who also donated all the stenting supplies.
Conflict of interest statement
F.Burzotta received speaker fees from Abbott Vascular, Abiomed, Medtronic, and Terumo. C.Trani received speaker fees from Abbott Vascular, Abiomed, Medtronic, Chiesi, Boston Scientific, and Terumo. C.Aurigemma received speaker fees from Abbott Vascular, Abiomed, Medtronic, Terumo, and Daiichi Sankyo. E.Romagnoli received speaker fees from Abbott Vascular and Terumo. T.Valenzuela has acontract with Medtronic. J.F.Lassen has received speaker fees from Medtronic, Boston Scientific, and Abbott. G.Stankovic has received speaker fees from Medtronic, Abbott, Boston Scientific, and Terumo. P.A.Iaizzo has aresearch contract with, and serves as an educational consultant for Medtronic. F.Bianchini receives aresearch grant from Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.