Abstract
Aims: The aim of this study was to assess whether the culotte technique could be improved by an additional kissing dilation prior to main branch (MB) stenting.
Methods and results: Double-kissing (DK) culotte was compared to the culotte and DK-crush techniques in a bench model (n=24). Results were evaluated for stent apposition, luminal opening and flow dynamics. The total procedure duration of DK-culotte was 18.3±3.4 minutes, significantly lower than for DK-crush (24.3±5.7 min; p=0.015), but similar to culotte (21.6±5.9 min, p=0.104). In DK-culotte the overall rate of moderate (200-500 µm) and significant (>500 µm) malapposition was 2.1±1.9% and 0.4±0.2%, similar as compared to culotte (3.7±3.8%, p=0.459 and 1.0±1.0%, p=0.517, respectively), and lower as compared to DK-crush (8.1±2.5%, p<0.001 and 3.7±5.3%, p=0.002, respectively). The lower malapposition rate of DK-culotte as compared to DK-crush was due to less moderate and significant malapposition in the proximal MB (0.0±0.0% vs 14.0±7.6%, p<0.001 and 0.0±0.0% vs 4.2±9.1%, p=0.026, respectively). Micro-computed tomography did not show a difference in luminal opening at the proximal MB, distal MB or SB. There was no difference either in the maximum shear rate or in areas of high shear or recirculation.
Conclusions: Bench test data suggest that the DK approach facilitates the culotte technique. The clinical validity and relevance remain to be confirmed in a larger in vivo population.
Introduction
Coronary bifurcations represent one of the most challenging settings for interventional cardiologists. This is due to the fact that conventional stents are designed and shaped to restore tubular geometry, while bifurcation anatomy is far more complex with different diameters and non-tubular cross-sections1. In addition, despite the fact that percutaneous coronary interventions (PCI) have evolved with different techniques using a single stent, two stents, or dedicated devices, the optimal treatment is still a matter of discussion in each individual case due to the highly complex and specific morphology of each bifurcation lesion2.
Provisional T-stenting has generally been considered as the gold standard technique because it is relatively simple and has also demonstrated excellent short- and long-term outcomes3,4. Nevertheless, its applicability might be limited in more complex coronary anatomies, when intentional double stenting techniques should be considered instead.
A wide variety of two-stent techniques has been described and evaluated. Among them, recent trials have demonstrated a favourable procedural and long-term outcome associated with the double-kissing crush (DK-crush) technique5. The specificity of this technique, as compared to the conventional crush technique, is the performance of an additional kissing balloon dilation of the side branch (SB) prior to main branch (MB) stenting. The advantage of this is that MB stenting should not cause relevant deformation towards the SB, and in the SB stent itself. Therefore, after MB stenting the access to the SB is more predictable and straightforward for the final kissing balloon dilation.
Single final kissing balloon dilatation is also foreseen for culotte stenting. The aim of the present study was to assess in bench models and human cases whether the culotte stenting technique could be improved by performing a “double-kissing approach”, i.e., by optimising the SB result with additional kissing balloon dilation before stenting the MB.
Methods
TESTED BIFURCATION TECHNIQUES
Reverse double-kissing (DK) culotte was investigated both in a bench model and in patients with amenable stenosis in bifurcations. The results of the reverse DK-culotte were compared to DK-crush or reverse culotte as reference techniques.
DK CULOTTE
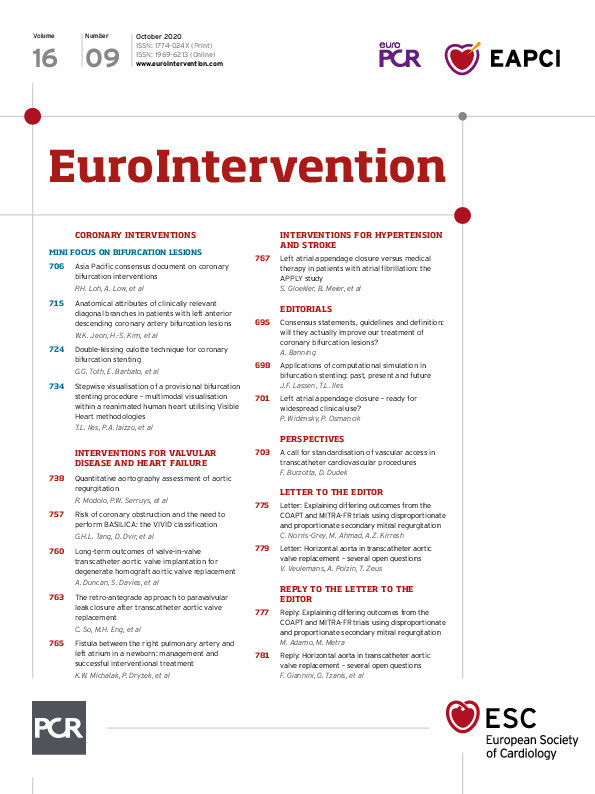
This technique differs from conventional reverse culotte by having one additional kissing balloon dilation, performed after SB stenting, prior to MB stenting. The technique has the following steps (Figure 1). Two guidewires (GW) are used, i.e., the “MB-GW” and the “SB-GW” (A). The SB-GW is advanced into the SB (B), and the stent is deployed in the continuity of the MB to the SB (C). The stent is then proximally optimised in the proximal MB (D). The MB-GW is introduced into the distal MB, crossing the previously implanted stent at the most distal cell (E). The cell can be first opened with a small balloon (F). Next, the first kissing dilation is performed using balloons fitted to the diameter of the distal branches. First, the SB balloon is inflated to maintain the stent architecture, followed by MB balloon inflation. Deflation is simultaneous (G). Next, the SB-GW is removed and a stent deployed in the continuity of the proximal to distal MB (H). The stent is then proximally optimised (I). Then the SB-GW is introduced into the SB, crossing the previously implanted stent at the most distal cell (J). The cell can be first opened with a small balloon (K). Next, the second kissing balloon dilation is performed, using balloons fitted to the distal branch diameters. First, the MB balloon is inflated in order to maintain its architecture, followed by the SB balloon. Deflation is simultaneous (L). As a final step, proximal optimisation is performed.
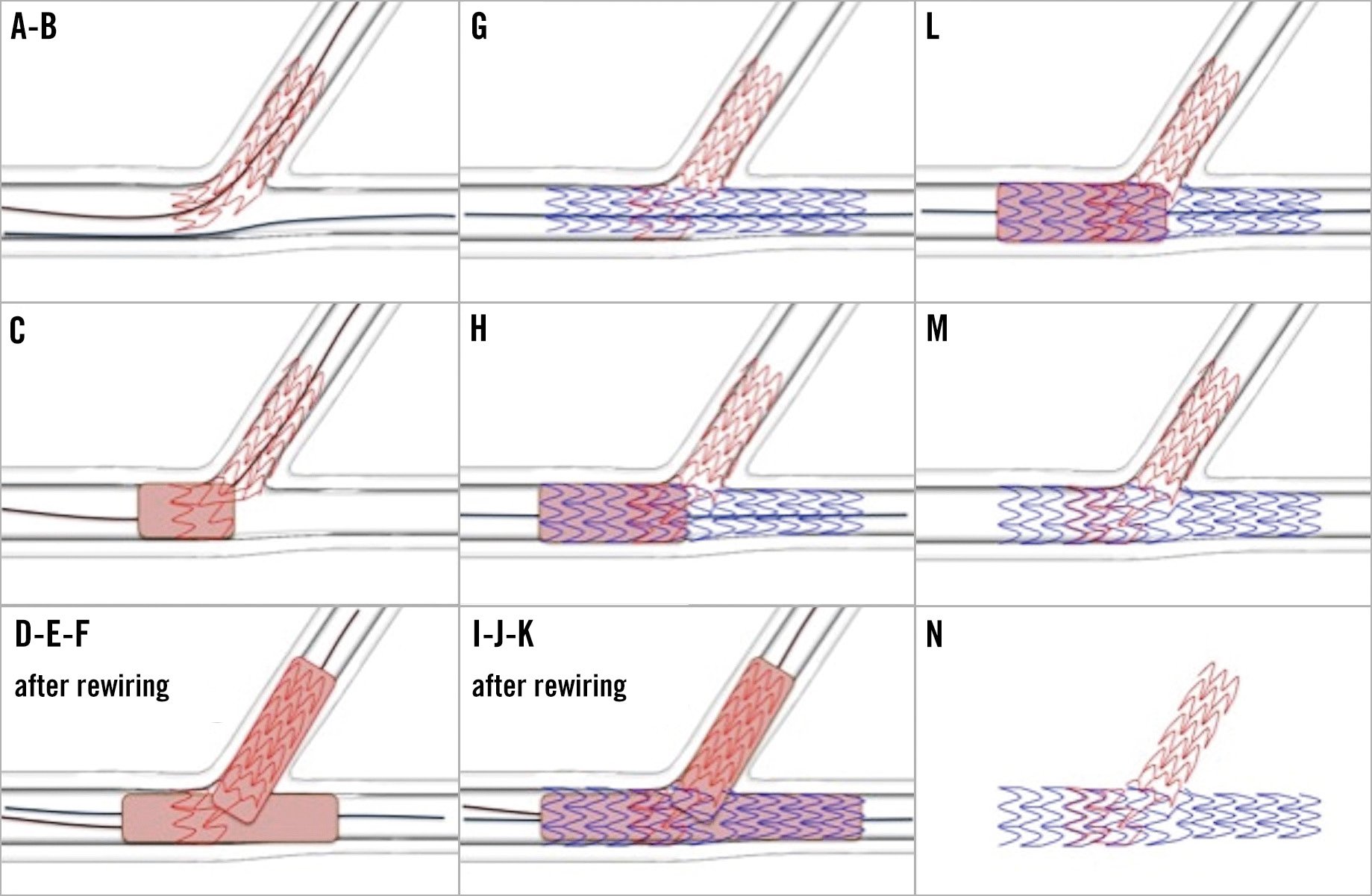
Figure 1. Steps of the DK-culotte technique. A)-L) Steps of the DK-culotte technique. Detailed description is in the main text. M) & N) Final constitution of the two stents.
REVERSE CULOTTE
This procedure is performed as previously described6, with additional proximal optimisation after each stenting step.
DK CRUSH
The procedure is performed as previously described7, with an additional proximal optimisation after crushing the SB stent.
For all three techniques the aim was to have 3 mm protrusion of the SB stent into the true proximal MB beyond the polygon of confluence, so far accurately achievable.
BENCH TEST
A total of eight tests were performed for each of the three techniques (DK-culotte, culotte, and DK-crush) in 3D printed, two-side polished, pure saline-filled silicone vessel phantoms. 3D bifurcation models were produced by a polyjet printer, using a rubber-like elastomeric material, called TangoPlus™ (Sirris Inc., Brussels, Belgium). Exact parameters are shown in Supplementary Figure 1. The procedures were performed by operators who had sufficient practical (human and bench) experience with both the DK-crush and culotte techniques. Accordingly, no trend of “improvement” in procedural times was observed over the period of the bench procedures, which suggests that cases were performed after the learning curve.
Procedural time was defined as the total duration between entering the bench model with the first GW until completing the last step of the procedure, as described above. Rewiring times were defined as the duration from the GW entering the bench model until it reached an optimal distal position in the branch being aimed for, through the aimed for cell.
OPTICAL COHERENCE TOMOGRAPHY
OCT imaging was carried out systematically at the end of each procedure for evaluation of apposition. Pullback runs were performed at 20 mm/s with a Dragonfly™ Duo OCT catheter (Abbott Vascular, Santa Clara, CA, USA) and analysed using a dedicated workstation (C7-XR™ OCT intravascular imaging system; Abbott Vascular). Images were recorded at 100 frames per second. Note that OCT pullback was only documentary and not meant to guide PCI. Bifurcations were analysed in six areas, namely: (1) 3 mm of the proximal MB; (2) 3 mm of the distal MB; (3) 3 mm of the SB; (4) polygon of confluence – abostial area; (5) polygon of confluence – roof; and (6) polygon of confluence – carina (Supplementary Figure 1).
Malapposition of stent struts was calculated as described previously8, graded as: (1) full apposition (no malapposition can be observed); (2) incomplete apposition (0-200 microns); (3) moderate malapposition (200-500 microns); and (4) significant malapposition (>500 microns). Note, OCT analysis was performed in parallel by two different groups (L. Di Stefano and D. Franco; V. Sasi and G. Szanto), blinded to the procedure and to the results of the other group.
MICRO-COMPUTED TOMOGRAPHY (µCT)
Final stent deformations were visualised at a voxel resolution of 15 microns/voxel. Scanned volumes were segmented using ITK-SNAP9, smoothed and reconstructed using a finite element meshing technique. Diameter and area stenosis in the proximal MB, in the distal MB and in the SB, as well as angulation between the MB and the SB axes were measured. Stenosis was quantified in a planar projection perpendicular to the segments’ axis, as appropriate following the definition proposed by Ormiston et al10, taking the largest circle fitting in the smallest luminal strut-free area as the luminal opening. Note, µCT analysis was performed blinded for the technique performed.
COMPUTATIONAL FLUID DYNAMICS (CFD) ANALYSIS
Flow patterns and shear rate were analysed to identify segments with higher risk of flow disturbance being induced. Two-dimensional longitudinal geometries were obtained from OCT. These were subsequently meshed and simulated with flow conditions similar to experimental conditions using fluid computational software (Fluent; Ansys, Canonsburg, PA, USA). Boundary conditions for this simulation included steady flat profile inlet flow velocity, simulating a flow rate of 200 mL/min. Inlet and outlet ends were extended based on respective diameters to allow flow development simulation. The area of high shear rate (>1,000 s−1), maximum shear rate and area of flow recirculation were obtained.
STATISTICAL ANALYSIS
All analyses were performed with GraphPad Prism 5.0 (GraphPad Software Inc., San Diego, CA, USA). Summary descriptive statistics are reported as mean±SD or number (%), as appropriate. Results of different techniques or models were compared by Mann-Whitney tests or the Kruskal-Wallis test, and categorical variables were compared with Fisher’s exact or chi-square tests, as appropriate. When analysing the malapposition rates, the average of the two groups’ results was taken on procedure and segment level. A probability value of p<0.05 was considered significant.
Results
All procedures with DK-crush (n=8), culotte (n=8), and DK-culotte (n=8) were successfully performed (Table 1, Figure 2). Total procedure duration of DK-culotte was 18.3±3.4 minutes, significantly lower than for DK-crush (24.3±5.7 minutes; p=0.015), but similar to culotte (21.6±5.9 minutes, p=0.104) (Figure 3). The duration of first rewiring through stent #1 was similar for DK-culotte and culotte (20.4±6.8 versus 23.8±9.5 seconds, respectively; p=0.440), with a trend for shorter duration as compared to DK-crush (30.5±13.3 seconds; p=0.086). There was a trend for shorter duration of second rewiring for DK-culotte compared to DK-crush (17.9±10.6 versus 28.1±12.9 seconds, respectively; p=0.087), while it was significantly shorter than for culotte (33.6±15.9 seconds; p=0.050).
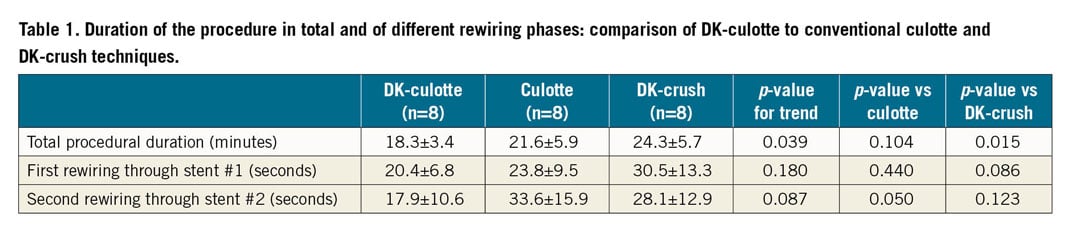
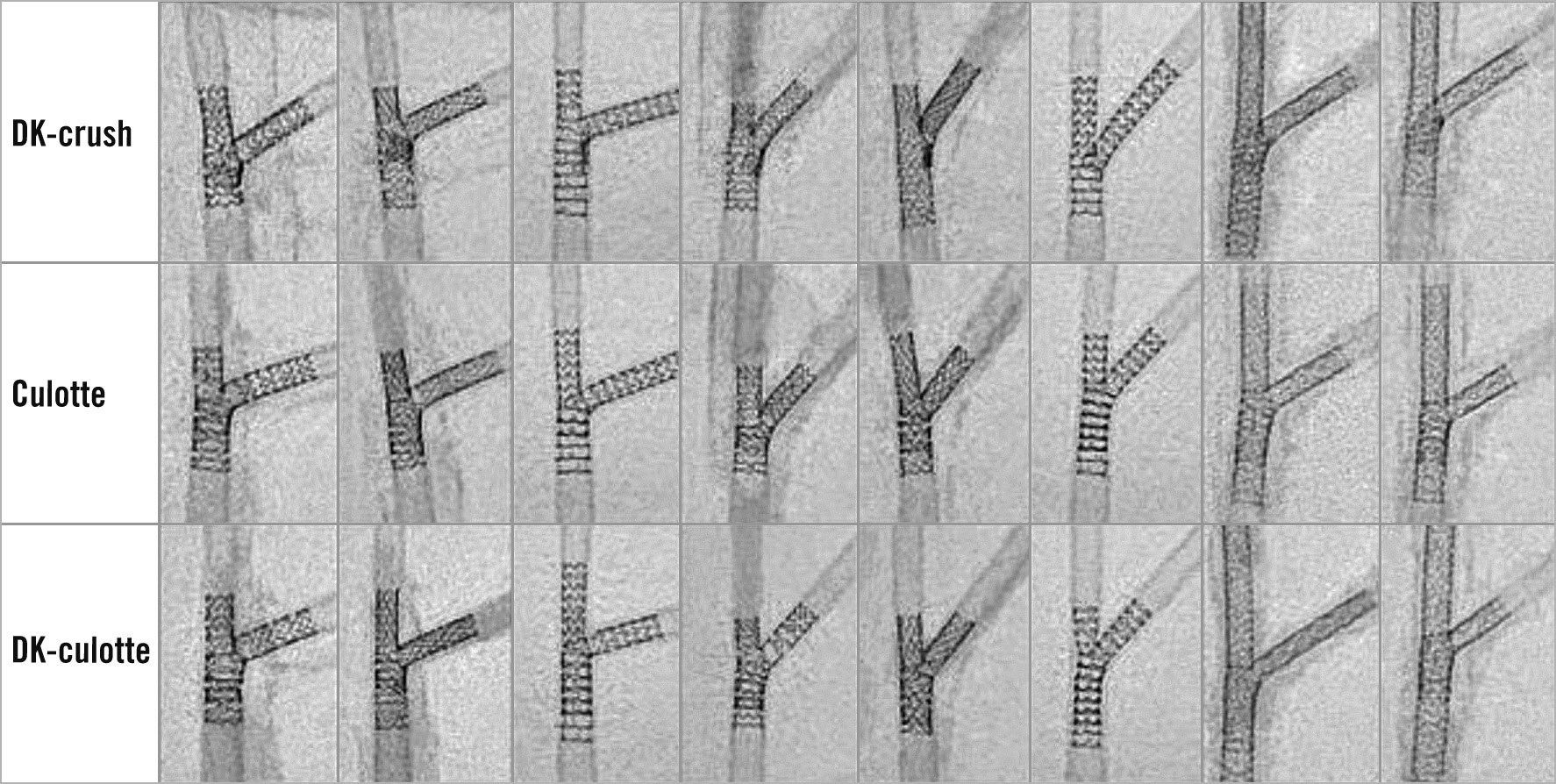
Figure 2. Final result of the in-bench procedures (n=8 for each technique).
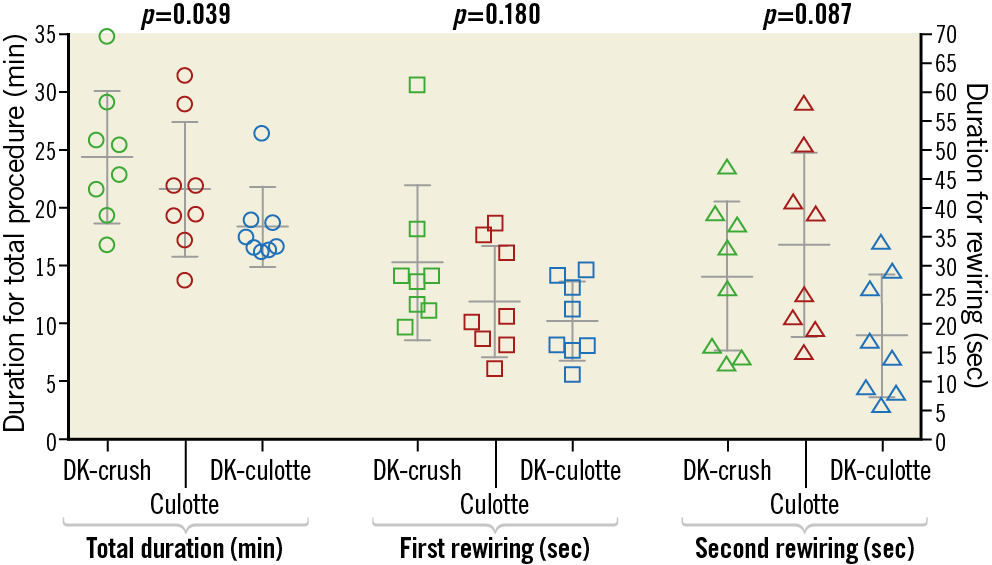
Figure 3. Duration of the procedure in total and of different rewiring phases: comparison of the DK-crush, culotte and DK-culotte techniques.
On average, 3.5±0.8 balloons were used per procedure for DK-culotte, similar to culotte (3.9±0.8) and DK-crush (4.0±0.5). Importantly, a smaller balloon(s) was needed for opening stent struts towards the jailed branch in 3 out of 8 DK-culotte, 3 out of 8 culotte and 7 out of 8 DK-crush cases. This might also be translated into longer procedural durations.
OPTICAL COHERENCE TOMOGRAPHY
OCT runs were obtained in all bench models. Image quality in one DK-crush case was not sufficient for proper assessment; it was therefore excluded. In total, 1,356 OCT frames were analysed and 12,735 struts were identified (Table 2). In DK-culotte, perfect apposition was seen in 69.2±12.2% of the struts, similar to culotte (69.6±14.5%) and to DK-crush (66.6±7.0%). The rate of moderate malapposition was 2.1±1.9%, while 0.4±0.2% of the struts were significantly malapposed in DK-culotte. These rates were found to be similar to culotte (3.7±3.8% and 1.0±1.0%, respectively), and significantly lower than in DK-crush (8.1±2.5% and 3.7±5.3%, respectively).
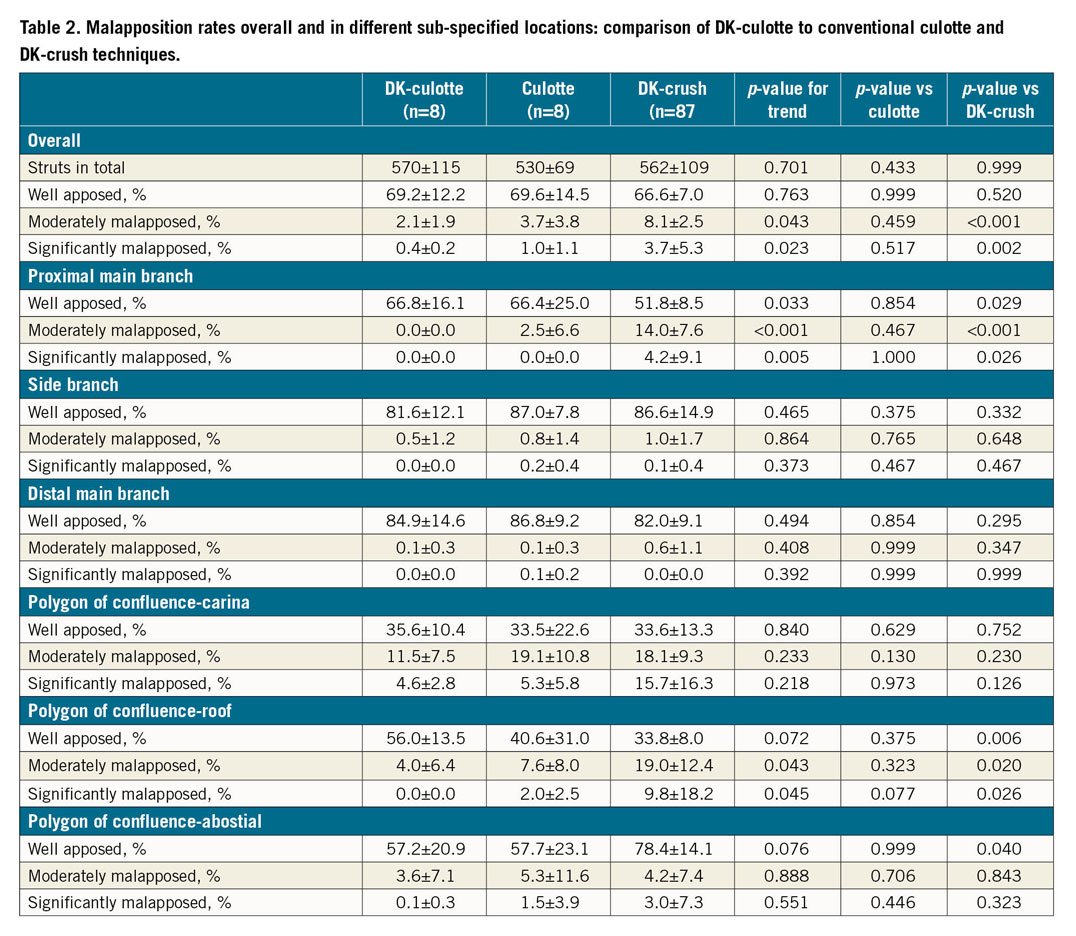
In the proximal MB, DK-culotte resulted in fewer moderately and significantly malapposed struts compared to DK-crush (0.0±0.0% vs 14.0±7.6%, p<0.001 and 0.0±0.0% vs 4.2±9.1%, p=0.026, respectively) with no difference compared to culotte (2.5±6.6%, p=0.467 and 0.0±0.0%, p=1.000). Moderate and severe malapposition was mainly detected in areas with multiple layers of struts and at their edges where the most inner stent layer “descends” towards the wall. Note, here multiple layers of stents were identified in 2.7±0.3 mm versus 2.6±0.3 mm versus 2.8±0.2 mm (p=0.438), respectively.
At the roof of the polygon of confluence, DK-culotte had less moderate or significant malapposition as compared with DK-crush and culotte. At the abostial site of the polygon of confluence, DK-crush had the highest rate of perfect apposition; however, the rate of moderate or significant malapposition was similar for all techniques. In the distal MB, SB and carina results were comparable for all techniques.
Performance in bifurcations angled 40° versus 60° versus 70° was similar in terms of moderate and significant malapposition in culotte (7±7% vs 3±0% vs 4±4%; p=0.896), in DK-culotte (4±2% vs 2±2% vs 2±0%; p=0.286) and in DK-crush (10±5% vs 19±6% vs 5±5%; p=0.221).
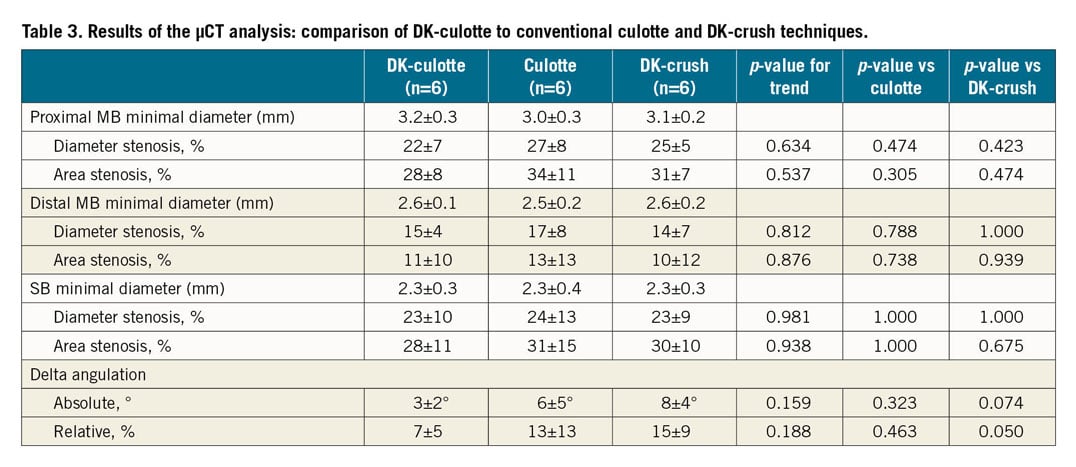
MICRO-COMPUTED TOMOGRAPHY
µCT analysis did not show any difference among the three investigated techniques in terms of luminal opening in the proximal MB, in the distal MB or in the SB (Figure 4, Table 3). However, DK-culotte changed the native SB angulation significantly less as compared to DK-crush (7±5% vs 15±9%, respectively; p=0.050). Compared to the culotte technique, the difference was statistically not significant (13±13%; p=0.463).
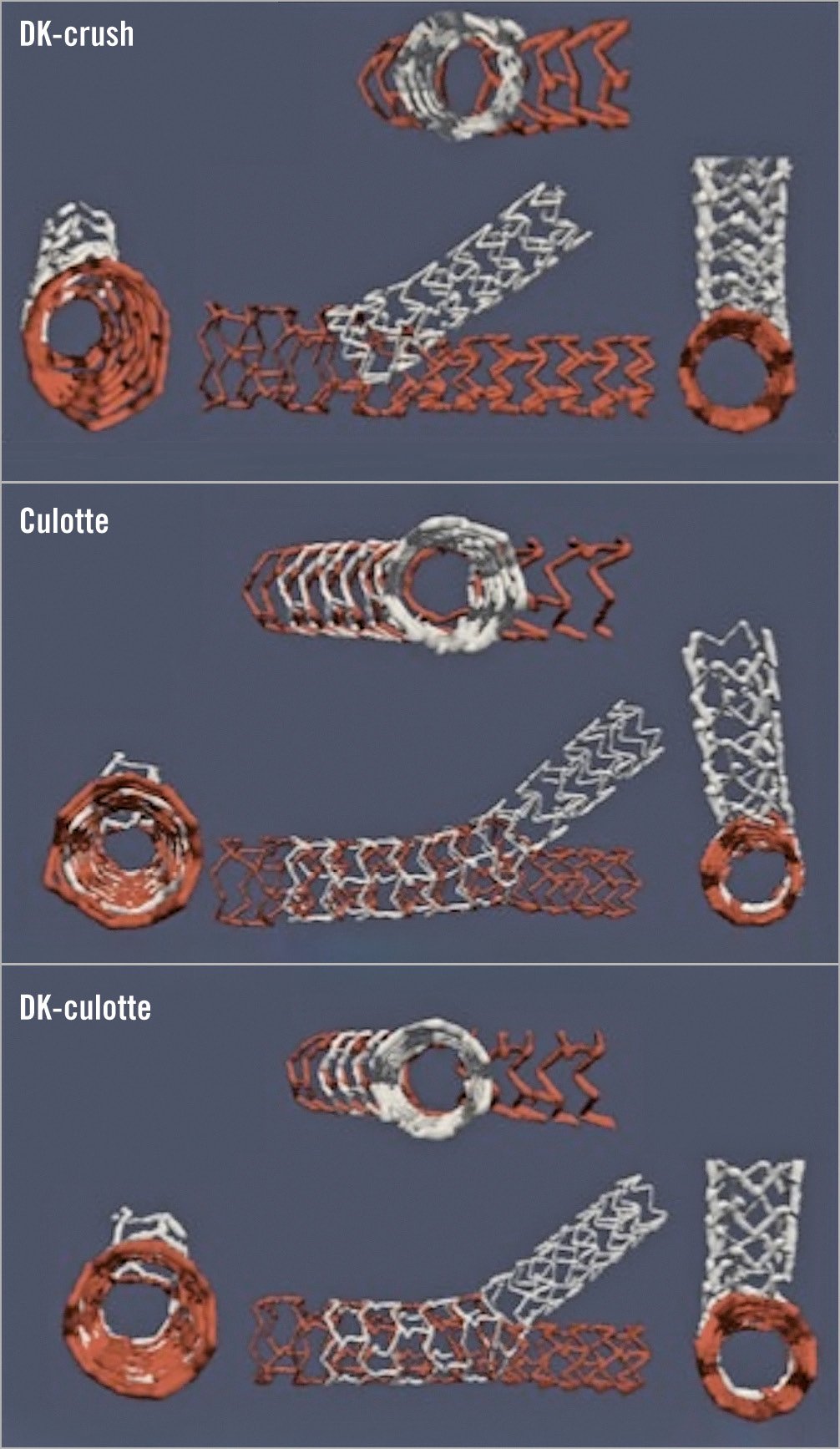
Figure 4. Representative cases from the 3D µCT reconstruction of DK-crush, culotte and DK-culotte procedures.
COMPUTATIONAL FLUID DYNAMICS (CFD) ANALYSIS
CFD analysis did not show any statistical difference among the techniques in terms of overall maximum shear rate, area of high shear or area of recirculation (Figure 5, Table 4). However, at the polygon of confluence, maximum shear rate was significantly higher for culotte as compared to DK-culotte (3,933±57 s−1 vs 2,590±580 s−1, respectively; p=0.041), while there was just a trend when compared to DK-crush (3,933±571 s−1 vs 2,593±293 s−1, respectively; p=0.055). Similarly, the area of high shear rate was also markedly higher for culotte than for DK-culotte (0.388±0.009 mm2 vs 0.175±0.004 mm2, respectively; p=0.050), showing just a trend when compared to DK-crush (0.388±0.009 mm2 vs 0.181±0.004 mm2, respectively; p=0.063) (Figure 6).
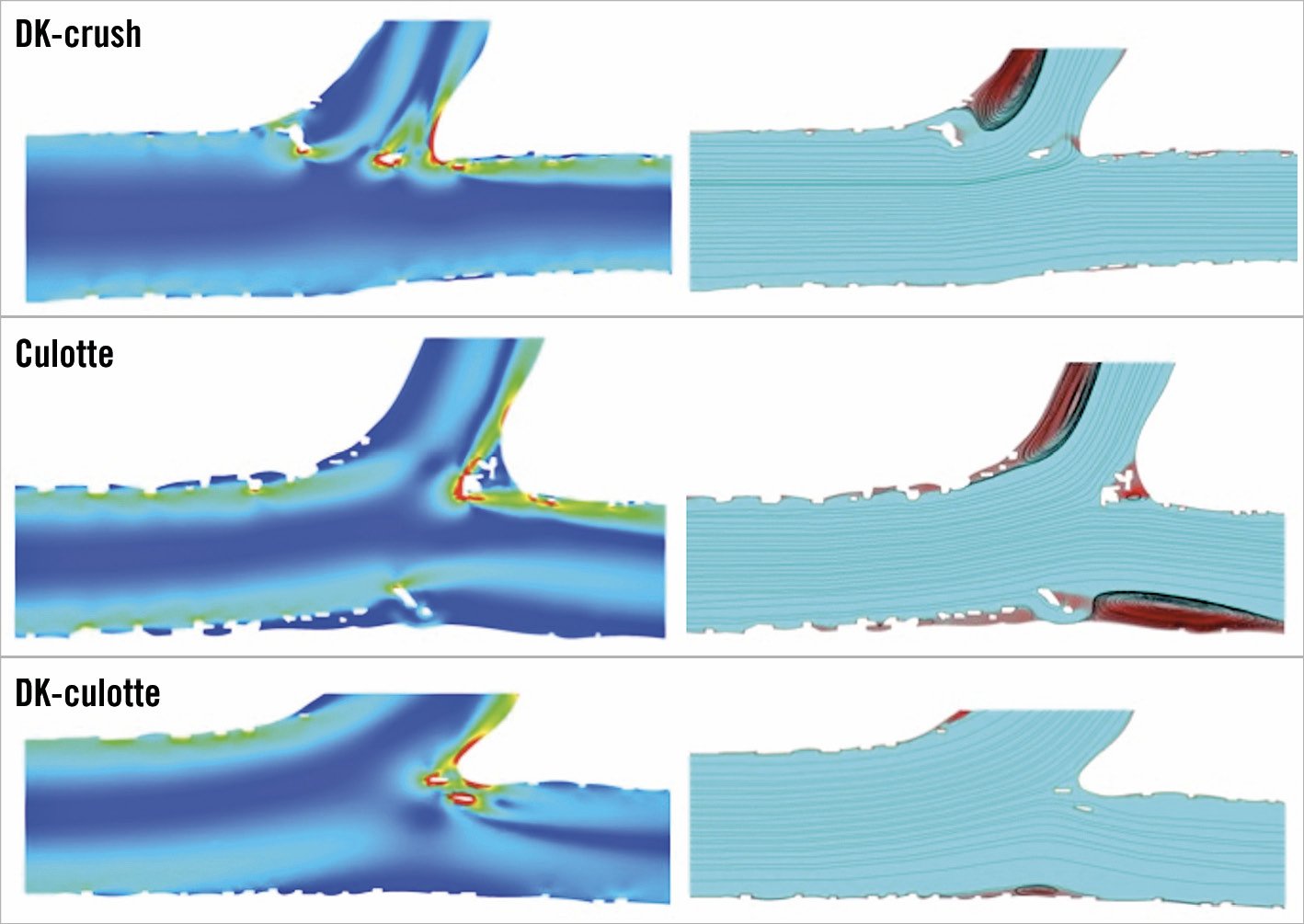
Figure 5. Representative cases for computational fluid dynamics analysis of DK-crush, culotte and DK-culotte procedures.
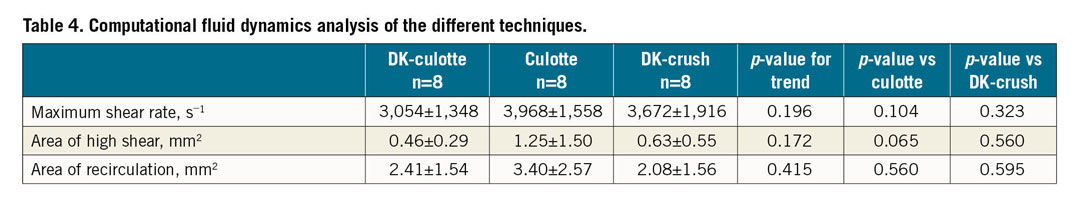
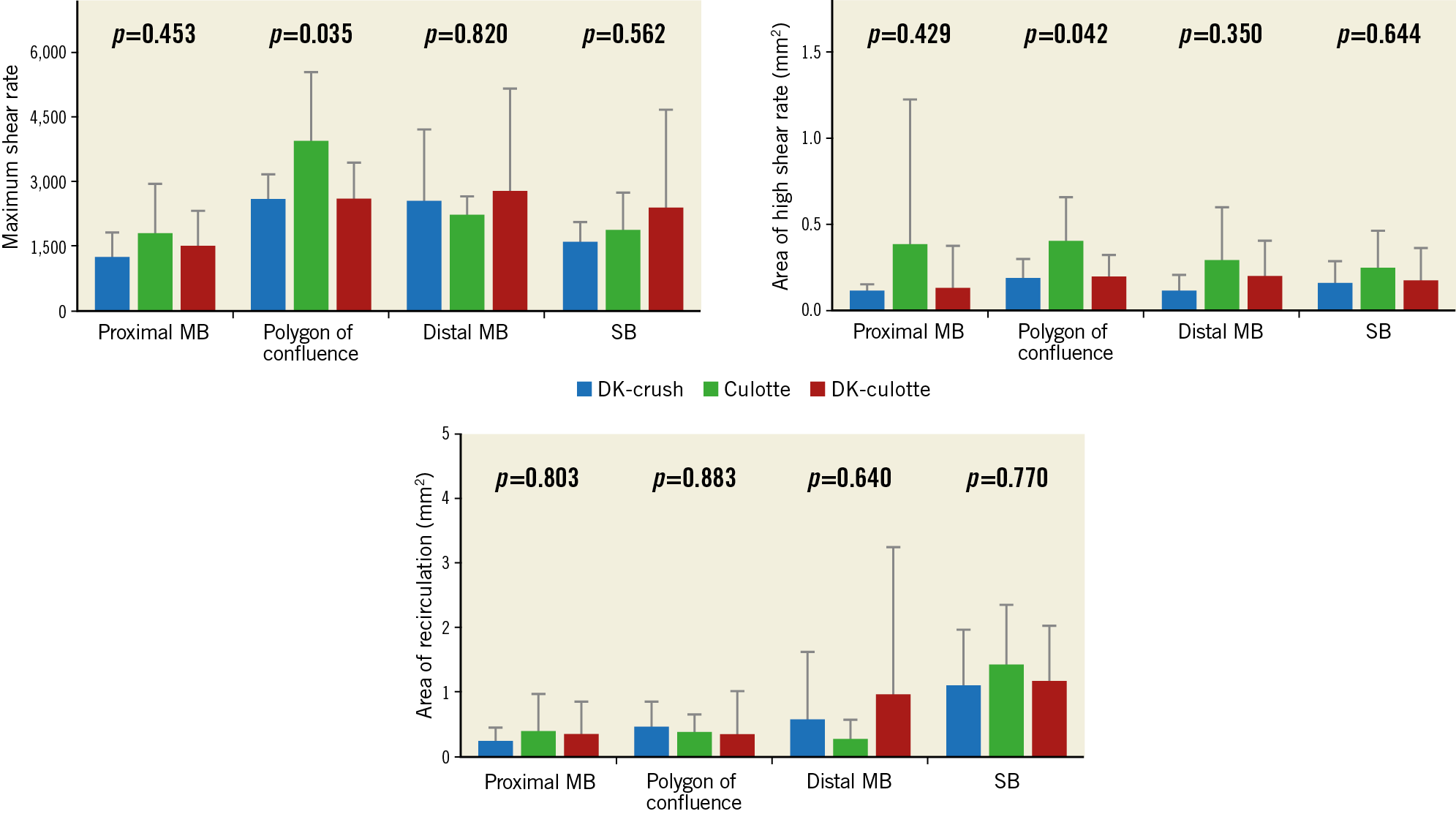
Figure 6. Segmented analysis of computational fluid dynamics in different areas of interest.
Overall, functional results were better in bifurcations with 70° angulation as compared to bifurcations with less than 70° angulation in terms of maximum shear rate (2,731±496 s−1 vs 4,018 ±1,804 s−1, respectively; p=0.044) and area of high shear (0.33±0.19 mm2 vs 1.07±1.12 mm2, respectively; p=0.007) with no difference in area of recirculation (2.36±2.38 mm2 vs 2.79±1.76 mm2, respectively; p=0.360).
Discussion
In the present study, we described a modified culotte technique, the DK-culotte technique. In the bench tests, DK-culotte resulted in a markedly lower stent malapposition at at least one location of the bifurcation, as compared to both the culotte and DK-crush techniques.
Nearly 10-15% of all PCI procedures are performed in relevant bifurcations. Although provisional T-stenting represents a good solution in most cases, it might not be the right option for the most complex coronary bifurcation anatomies, such as true bifurcations when a large SB is stenosed over a long segment. In these cases, provisional T-stenting does not always provide optimal and predictable results, suggesting that intentional double-stenting techniques should be considered instead2,11.
A wide variety of two-stenting techniques has been described and evaluated, including T-stenting, T-and-protrusion, culotte and double-kissing crush (DK-crush), single string, reverse string stenting, etc. The main limitations with these techniques are related to the multiple metallic layers, frequent stent strut malapposition and neocarina formation, incomplete vessel coverage and major deformation of the stent architecture. However, among all these techniques, recent clinical data support DK-crush the most. Although a triple stent layer in the proximal MB and major deformation of the stent architecture are relevant criticisms of DK-crush, its major advantages are the minimal neocarina (as compared to the T-and-protrusion technique), the perfect SB ostium coverage (as compared to the T-stenting technique) and the good stent apposition at the level of the SB, achieved by the first and maintained by the second kissing dilation. These advantages are reflected by favourable outcome data5.
Considering that the physiological integrity of the vessel lumen plays a key role in the maintenance of normal flow patterns, during bifurcation PCI emphasis has to be placed on avoidance of any disturbance (i.e., ovoid shape, changed angulation, floating struts, massive stent deformation). Accordingly, the more the native tubular anatomy is reconstructed instead of construction of a neo-anatomy, the more physiologic flow patterns can be expected with less turbulence, lower loss in driving pressure, less impaired shear-stress patterns and eventually even less abnormal platelet activation12,13. From a structural point of view, the culotte technique might be considered as more “physiologic”, as it ensures full coverage in all three segments (as compared to T-stenting); there is minimal or no neocarina (as compared to T-and-protrusion); there is no triple layer (as compared to DK-crush); and the tubular architecture of the stents is maintained with fractal deformation only (as compared to DK-crush). Still, these structural advantages can be achieved only in case of perfect performance, which might often be limited by certain technical restraints, namely, while opening the struts of the first stent (i.e., the MB stent towards the SB in conventional culotte; the SB stent towards the MB in reverse culotte), major deformation is caused in the stent architecture by pulling multiple struts away from the SB and towards its ostium (Figure 7, Moving image 1). This causes major malapposition in the SB stent; however, it can probably be corrected with the final kissing. However, these malapposed struts can complicate the rewiring process or result in false rewiring, which jeopardises the feasibility and accuracy of the final kissing dilation. The latter can lead to major clinical consequences, since lacking final kissing balloon dilatation is one of the major conditions associated with target lesion failure in the long term in any double-stenting technique14.
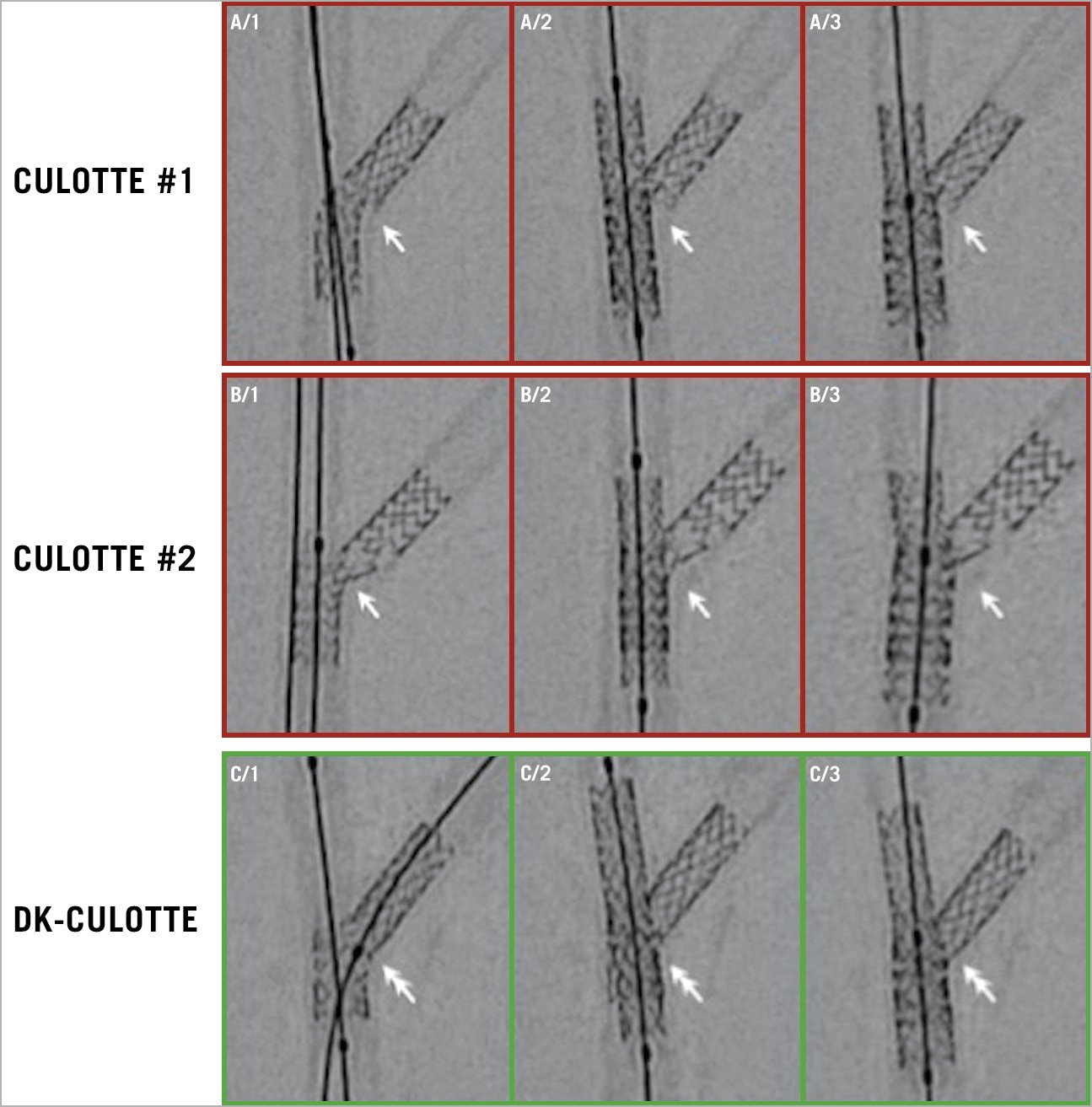
Figure 7. Typical SB stent behaviour during MB stenting with culotte vs DK-culotte techniques. A) & B) SB stent deformation during MB opening and MB stenting in the culotte technique, resulting in difficult SB access for final kissing dilation. C) DK-culotte allows the maintenance of the SB result during MB preparation and stenting, resulting in a favourable SB access for final kissing dilation.
The present feasibility study aimed to assess whether the “double-kissing” approach might be beneficial for the culotte technique as well. The rationale behind this is that first kissing balloon dilation could already produce the desired SB result while also preparing the MB access. Then, a second kissing balloon dilation completes the MB result, while maintaining the result in the SB (Figure 7, Moving image 2). As suggested by data derived from bench tests, the double-kissing approach for culotte shows benefits as compared to DK-crush but also as compared to culotte: DK-culotte resulted in a markedly lower rate of moderately or significantly malapposed struts. This finding was most pronounced in the proximal MB and in the roof of the polygon of confluence. In the latter location, DK-culotte demonstrated a trend for a better result as compared to culotte. As expected, both DK-culotte and culotte showed a lower rate of perfect apposition at the abostial site of the polygon of confluence (i.e., where stent opening might be limited by another stent); however, the rates of moderate or significant malapposition remained similar. As a consequence, even though statistical difference was not reached, the simulated flow patterns were closest to physiologic after DK-culotte with the lowest shear rates. Interestingly, the better structural performance could be achieved within a shorter procedural duration despite the additional step of kissing balloon dilation. This might be explained by the prepared and maintained access to the jailed branches and the simpler rewiring and balloon access as a consequence. We did not find statistical difference in the luminal opening, as assessed by µCT, even though there was a numerical trend, especially in the proximal MB, favouring DK-culotte. Interestingly, the native bifurcation angle was markedly less influenced by DK-culotte as compared to DK-crush, which could have relevance in fluid dynamics, as described above. These findings suggest that post-procedural anatomy after the DK-culotte procedure can be close to the native anatomic structure. Although detailed physiologic evaluation was beyond the scope of this project, one can speculate that a near-normal geometry will translate into near-normal haemodynamics, with potential pathophysiological benefits and better long-term outcomes. Still, computational flow dynamics analysis did not reveal any functional differences among the tested techniques.
Limitations
(1) During our bench tests we could not incorporate the impact of different plaque distribution and plaque composition. Even though high-precision 3D printing was used for preparing bench models, the variability between two models was not assessed and therefore cannot be excluded. (2) Due to geometric incoherence (namely the angulation between the plane of the OCT image and the true cross-sectional plane of the SB ostium), the accuracy of OCT in evaluating malapposition was hampered by marked overestimation, especially at the level of the carina. Additionally, in one DK-crush case, OCT had poor image quality; therefore, it was excluded from the analysis. (3) Computational flow dynamics allows assessment in one single longitudinal plane, neglecting the three-dimensional deformation of the stent structure during bifurcation PCI.
Conclusions
Bench tests suggest that the double-kissing approach can significantly facilitate the performance of the culotte technique. The additional kissing balloon dilation allows a significant reduction in the total procedural duration, while resulting in better optimised overall final strut apposition. In this respect, DK-culotte may be superior not only to conventional culotte, but also when compared to the DK-crush technique, which is currently often performed. The clinical validity of the present findings remains to be confirmed in a larger in vivo study population.
|
Impact on daily practice Understanding the structural benefits of the DK approach during culotte stenting can facilitate complex bifurcation stenting during everyday practice. In addition, it sheds new light on potential disadvantages of conventional culotte stenting, explaining historical clinical differences, when compared to DK-crush. |
Funding
Testing equipment, including guidewires, stents and balloon catheters, were provided by Abbott Laboratories Inc. (IL, USA), Medtronic Inc. (Minneapolis, MN, USA), Biotronik AG (Bülach, Switzerland) and Terumo Inc. (Tokyo, Japan), without financial involvement or intellectual restriction.
Conflict of interest statement
G. Toth has received personal fees from Abbott, Medtronic, Biotronik and Boston Scientific, outside the present work. E. Barbato has received speaker’s fees from Abbott Vascular, Boston Scientific, GE and Opsens, outside the present work. W. Wijns has received institutional research grants from MicroPort and Terumo. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. SB stent deformation during MB opening and MB stenting in the culotte technique, resulting in difficult SB access for final kissing dilation.
Moving image 2. DK-culotte allows the maintenance of the SB result during MB preparation and stenting, resulting in a favourable SB access for final kissing dilation.