Multivessel coronary artery disease (MVD) is a common clinical condition in patients undergoing percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI). To be precise, up to 65% of patients with STEMI have angiographically significant lesions beyond the culprit lesion causing the acute event1, which are typically a matter of debate in clinical practice. They may represent stable coronary plaques, with limited expected benefit from preventive revascularisation unless the subtended territory is relevant. On the other hand, lesions with the angiographic appearance of unstable plaques may trigger future events, and PCI in such non-culprit lesions may confer a prognostic benefit. Importantly, intravascular imaging may add further information to the clinical decision making2, and the indication for non-culprit vessel PCI should be based on physiological measures rather than on plain angiography3.
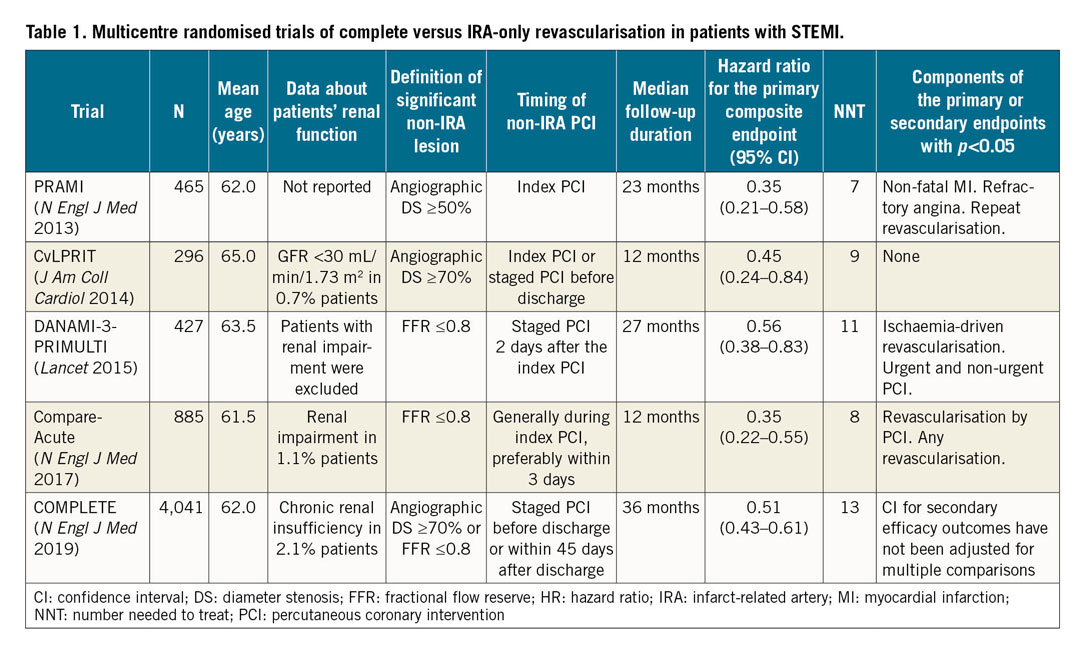
Multicentre randomised trials have suggested that complete revascularisation reduces adverse outcomes4. However, the debate is still open as to whether revascularisation should be completed in a staged procedure, to allow complete recovery (either before or after discharge), rather than to pursue it in a single session for the convenience of the patients and for economic efficiency5,6. Each trial (Table 1) demonstrated a consistent reduction in the composite ischaemic endpoint with a small number needed to treat (NNT). This was mainly driven by a lower number of softer events such as the need for urgent or subsequent revascularisation, but the pooled estimate (n=6,114 patients) shows a signal of reduced mortality (HR 0.75, 95% CI: 0.51-1.10, personal calculation). European guidelines now suggest considering completion of revascularisation in patients with STEMI and MVD before hospital discharge.
In the current issue of EuroIntervention, Song et al7 present a nationwide four-year prospective comparison of Korean patients with severe chronic kidney disease (CKD) receiving multivessel or culprit-only PCI for acute myocardial infarction and MVD.
In their final sample consisting of 326 propensity-matched patients, they found that the risk of one-year MACE was similar. Interestingly, at sensitivity analysis, the incidence of MACE was higher in patients with STEMI receiving multivessel intervention (adjusted HR 1.90, 95% CI: 1.12-3.22, p=0.017).
How can these data be reconciled with the current evidence in favour of multivessel intervention in patients with STEMI and MVD in the light of the largest study to date, the recently published COMPLETE trial6?
It should not be unexpected that patients with severe renal dysfunction and MVD did not receive a benefit from complete revascularisation over a one-year period. This is probably inherent with the high burden of comorbidities and the high risk of adverse events of patients with severe CKD, which in itself is a powerful predictor of early negative outcomes independently from the completeness of revascularisation (overall MACE and mortality rates were 40.8% and 27.6%, respectively)7. In addition, the theoretical advantages of multivessel PCI in patients with severe CKD may be offset by a higher risk of periprocedural and post-procedural complications8: patients receiving multivessel PCI had a trend towards worsening of renal function (adjusted OR 2.13, 95% CI: 0.98-4.67)7. On the other hand, as the decision for complete revascularisation was made on a selective clinical basis, we might speculate that a selective strategy of complete revascularisation in patients with severe CKD is safe, although apparently useless. Also, taking into account the prospective cohort design of the study7 and the small final sample size, as compared with the available randomised trials (Table 1), the actual interaction between procedures and outcomes cannot be clearly ascertained.
However, the authors should be commended for their attempt to fill a major gap in knowledge in a very high-risk population (notably, mean age and eGFR were 75.4 years and 19.1 mL/min/1.73 m2, respectively)7. Elderly patients with such advanced CKD are mostly unrepresented in trials of complete revascularisation (Table 1), and the recently published CULPRIT-SHOCK trial demonstrated that single session complete revascularisation in patients with cardiogenic shock leads to an early excess in adverse renal outcomes and mortality9. Therefore, it is intuitive that patients with severe CKD are particularly prone to adverse outcomes10 after having received complex multiple PCI, especially if they are haemodynamically unstable.
Given the lack of randomised data, which will hardly ever be available, clinical judgement3 plays a central role in the decision making regarding whether to proceed to multivessel PCI in patients with acute myocardial infarction and severe CKD. Although some tight non-culprit lesions might prompt early treatment6, anatomical and functional data should be weighed against the high frailty of these patients.
Conflict of interest statement
G. Andò reports personal fees and non-financial support from Bayer, personal fees from Daiichi Sankyo, personal fees and non-financial support from Pfizer-Bristol Myers Squibb, personal fees and non-financial support from Boehringer Ingelheim, personal fees from Menarini, personal fees from AstraZeneca, personal fees from Chiesi, personal fees from Biosensors, non-financial support from Terumo, outside the submitted work. The other authors have no conflicts of interest to declare.