Introduction
Despite the established usefulness of optical coherence tomography (OCT) guidance in percutaneous coronary intervention (PCI), the quality of the OCT images obtained is sometimes poor due to inadequate clearance of blood flow in cases involving extremely tight stenotic lesions. Increasing the volume of contrast media, generally used for blood flow clearance, is also a problem. A novel OCT procedure, the “low molecular weight dextran (LMWD) infusion followed by catheter push (D-PUSH)” procedure, in which an OCT catheter is advanced from the proximal to distal target lesion segment after initiating LMWD infusion from a guiding catheter, may improve image quality compared with conventional OCT procedures. The aims of the current study were to evaluate image quality obtained by the D-PUSH procedure compared with the conventional OCT procedure in patients with acute coronary syndrome (ACS).
Methods
STUDY POPULATION
A total of 50 ACS patients who underwent the novel D-PUSH OCT procedure by pre-specified operators (Y. Shibata and H. Okazaki) were prospectively enrolled. These two operators had previously performed the D-PUSH procedure 10 times and thus were well trained. Patient enrolment details are shown in Supplementary Figure 1.
ANGIOGRAPHIC ANALYSIS
Qualitative coronary angiographic analyses were performed for the initial coronary angiography to evaluate lesion location, lesion complexity, and Thrombolysis In Myocardial Infarction (TIMI) flow grade. After obtaining a TIMI flow grade of ≥2, quantitative coronary angiography (QCA) analyses were performed to measure variables, including lesion length, minimal lumen diameter (MLD), reference vessel diameter, % diameter stenosis, and TIMI flow grade.
OCT PROCEDURE
For cases with initial coronary angiography TIMI flow grades <2, we first performed intracoronary thrombectomy before OCT examination. The OCT imaging of the culprit lesion was acquired by frequency-domain OCT (Abbott Vascular, Santa Clara, CA, USA) after administering intracoronary nitroglycerine. First, we performed the novel OCT procedure, D-PUSH, followed by the conventional OCT procedure. When performing D-PUSH and conventional procedures, “flush mediums” on the OCT system (OPTIS™ mobile; Abbott Vascular) were set to “1:1 (contrast:saline)” where the refractive index was 1.393, and “contrast” where the refractive index was 1.449. Supplementary Figure 2 and Moving image 1 show a representative case where the middle portion of the right coronary artery lesion (Supplementary Figure 2A) was evaluated by D-PUSH and conventional OCT procedures. The D-PUSH procedure involves four steps: i) an OCT catheter is placed proximal to the lesion (Supplementary Figure 2B, Moving image 2); ii) LMWD is infused via an automated injector (Zone Master SR Fusion; Sugan Co. Ltd., Osaka, Japan) into the right coronary artery at a rate of 3 mL/s for 6 seconds from the guiding catheter and, if the culprit lesion is in the left coronary artery, LMWD is infused at a rate of 4 mL/s for 6 seconds; iii) two seconds after initiating infusion, the catheter is advanced distal to the lesion (Supplementary Figure 2C, Moving image 2); and iv) the optical lens is then automatically pulled back proximally from distal to the lesion for 75 mm at 36 mm/s (0.2 mm/frame). Conventional OCT examination was performed following the D-PUSH procedure using the current protocol. An OCT catheter has already been placed distal to the lesion (Supplementary Figure 2D, Moving image 3), after which an optical lens is automatically pulled from the distal to proximal sections of the lesion for 75 mm at 36 mm/s (0.2 mm/frame) while infusing contrast media into the right coronary artery at a rate of 3 mL/s for 4 seconds (Supplementary Figure 2E, Moving image 3). In the case of a left coronary artery lesion, contrast media is infused from the guiding catheter at a rate of 4 mL/s for 4 seconds. Lesions were examined using both the D-PUSH and conventional procedures up to two times each at the operator's discretion.
OCT IMAGE ANALYSIS
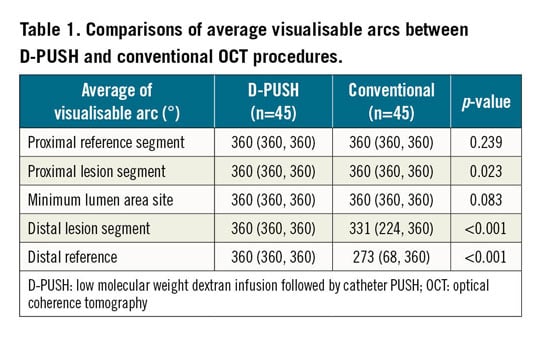
All OCT images were analysed by an independent cardiologist (N. Kobayashi) who was blinded to the clinical presentation and OCT procedure protocols. An analysed vessel was divided into five segments, as shown in Supplementary Figure 2A. We performed further quantitative OCT analyses to compare the image quality of D-PUSH with conventional OCT examination. Supplementary Figure 2F and Moving image 4, and Supplementary Figure 2G and Moving image 5 demonstrate representative OCT images obtained by D-PUSH and conventional procedures, respectively. Degrees of visualisable arcs were assessed every 1 mm, and the average degree of visualisable arc in each segment was compared between D-PUSH and conventional procedures (Supplementary Figure 2H) for each patient using the paired Wilcoxon signed-rank non-parametric test. Cases where the average visualisable arc of the distal lesion segment was ≥45° wider in the D-PUSH procedure compared with the conventional procedure were defined as D-PUSH-preferred cases.
Results
Of 50 enrolled patients, 84% were male. The median age was 69 years and median creatinine level on admission was 0.83 mg/dL. Detailed baseline clinical characteristics and laboratory data are shown in Supplementary Table 1. There was no statistical difference between creatinine levels before and after the procedures (median 0.83 mg/dL vs 0.74 mg/dL, p=0.069). Among the 50 enrolled cases, analysable OCT images could be obtained in 45 cases (Supplementary Figure 1). On average, we performed D-PUSH and conventional procedures 1.2 and 1.3 times per patient, respectively. Angiography and OCT findings are shown in Supplementary Table 2. Of the 45 lesions, we were unable to use either D-PUSH or conventional procedures to evaluate plaque morphologies (i.e., ruptured or unruptured) in two cases due to massive residual thrombi. Of the remaining 43 lesions, plaque morphologies in 11 lesions could not be assessed by the conventional procedure whereas D-PUSH was able to assess all cases (23 were plaque rupture and 20 were non-plaque rupture). A comparison of OCT image quality between D-PUSH and conventional procedures is shown in Table 1. Average visualisable arcs evaluated by D-PUSH were wider compared with conventional procedure in proximal (p=0.023) and distal (p<0.001) lesion segments, as well as in distal reference segments (p<0.001). Receiver operating characteristic (ROC) curve analysis showed a required MLD cut-off value of 0.49 mm to predict D-PUSH-preferred cases (Supplementary Figure 3).
Discussion
OCT exhibits superior axial resolution compared with intravascular ultrasound. Conversely, OCT has disadvantages, such as requiring complete blood clearance from the lumen for imaging, as well as increased amounts of contrast media to eliminate blood. Contrast media infused from the guiding catheter fails to eliminate blood flow in cases of severely stenotic lesions, e.g., lesions with an MLD ≤0.49 mm, due to the OCT catheter becoming wedged in the lesion. OCT-guided PCI is not recommended for patients with unknown renal function, as it requires additional contrast media. Therefore, in these cases, we recommend the novel OCT procedure, D-PUSH, which more reliably eliminates blood flow and avoids using large volumes of contrast media. A recent report described the safety of OCT-guided PCI using LMWD compared with intravascular ultrasound guidance on renal function1. Because LMWD and contrast media have different refractive properties, the flush medium setting on the OCT system is changed if available. If a change of setting is not available, area and length measurements of images acquired with LMWD are corrected by multiplying by 1.117 and 1.057, respectively2.
In real clinical practice, contrast media infusion followed by catheter push (C-PUSH) can be applied to patients with tight stenotic lesions, who do not exhibit renal insufficiency (Supplementary Figure 4, Supplementary Figure 5, Moving image 6–Moving image 12). Because understanding the catheter advancement timing is comparatively easier in C-PUSH than D-PUSH, C-PUSH can be an initial step for D-PUSH training.
Limitations
This study demonstrated the usefulness of D-PUSH in a limited number of ACS subjects. Lesions with severe calcification or tortuosity, as well as patients with critical conditions, were excluded. Currently, the reproducibility of the D-PUSH procedure for stable (non-thrombotic) lesions remains uncertain. In addition, the advantage of using LMWD instead of contrast media to avoid renal damage was not proven in the current study.
Conclusions
OCT image quality obtained by D-PUSH was higher compared with conventional procedures, particularly in cases involving extremely tight stenotic lesions with an MLD ≤0.49 mm.
|
Impact on daily practice When performing primary PCI for patients with kidney disease or unknown renal function, D-PUSH OCT is useful to evaluate tight stenotic lesions without the use of large volumes of contrast media. The biggest advantage of D-PUSH is obtaining information from the distal part of the lesion, which helps operators when deciding PCI strategies, e.g., stent length and diameter. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Angiography image from severely tight stenotic lesion in the middle portion of the right coronary artery.
Moving image 10. OCT image for the stenotic and tortuous right coronary artery lesion obtained by the conventional OCT procedure.
Moving image 11. Angiography image from the C-PUSH OCT procedure for long, tandem, partially calcified lesions in the middle portion of the left anterior descending artery.
Moving image 12. OCT image of long, tandem left anterior descending artery obtained by the C-PUSH procedure.
Moving image 2. Angiography image from the D-PUSH OCT procedure.
Moving image 3. Angiography image from the conventional OCT procedure.
Moving image 4. OCT image for severely tight stenotic right coronary artery lesion obtained by the D-PUSH OCT procedure.
Moving image 5. OCT image for severely tight stenotic right coronary artery lesion obtained by the conventional OCT procedure.
Moving image 6. Angiography image from severely tight stenotic lesion in the distal portion of the right coronary artery with partial tortuousness.
Moving image 7. Angiography image from the C-PUSH OCT procedure.
Moving image 8. Angiography image from the conventional OCT procedure.
Moving image 9. OCT image for the stenotic and tortuous right coronary artery lesion obtained by the C-PUSH OCT procedure.