Coronary artery disease (CAD) and aortic stenosis (AS) share a number of risk factors and pathogenetic pathways underlying their frequent coexistence1. Indeed, CAD is present in a large number of patients with severe AS requiring valve replacement2,3.
The presence of CAD has been consistently associated with impaired clinical outcomes after surgical aortic valve replacement (SAVR)4. Accordingly, current guidelines recommend coronary revascularisation of all significant stenoses in patients undergoing SAVR5. Conversely, the prognostic implications of CAD in patients with severe AS undergoing transcatheter aortic valve implantation (TAVI) are subject to ongoing debate. TAVI patients are frequently elderly with relevant comorbidities beyond CAD, such as diabetes mellitus, chronic kidney disease, pulmonary hypertension, and heart failure6. In view of this high baseline risk profile, it is debated whether the presence of CAD has any impact on clinical outcomes or whether the severe valvular heart disease and the extent of comorbid conditions make any prognostic impact of myocardial ischaemia ignorable in patients undergoing TAVI. Several authors have investigated the effect of CAD on clinical outcomes after TAVI with conflicting results7,8. However, the extent and complexity of CAD in patients undergoing TAVI is very heterogeneous, ranging from simple single-vessel to complex multivessel disease. It is therefore reasonable to hypothesise that the prognostic impact of CAD after TAVI may vary based on the anatomic extent and complexity of the disease.
In this issue of the journal, Khawaja and colleagues9 report the findings of a retrospective, single-centre, observational investigation on the effect of CAD on outcomes in 271 consecutive patients with severe AS undergoing TAVI. Ninety-three patients (34.3%) had significant CAD, defined as ≥70% stenosis in an epicardial coronary vessel (≥50% for left main or saphenous vein graft lesions) by quantitative coronary angiography on angiograms acquired prior to TAVI. Patients with CAD had a similar risk of all-cause mortality as compared to patients without CAD at 30 days and at one year of follow-up (7.5% vs. 6.7% and 23.7% vs. 21.5%, p=0.805). The authors also performed a secondary analysis to evaluate the impact of CAD on outcomes according to disease extent and complexity as assessed with the SYNTAX score. Patients with the highest SYNTAX score (≥32) had a significantly increased risk of all-cause mortality as compared to patients with intermediate (23-32) and low (≤22) SYNTAX scores at 30 days (14.3% vs. 11.1% vs. 5.2%) and one year of follow-up (57.1% vs. 22.1% vs. 23.3%, p=0.007). Of note, the SYNTAX score calculation was based on coronary anatomy at the time of TAVI after any revascularisation procedure – namely the “residual” SYNTAX score.
The authors should be praised for such an accurate work. They aimed to address a relevant clinical question by retrospectively investigating a well-conducted institutional registry, applying a rigorous methodological approach for the definition of CAD and the assessment of CAD complexity by the use of the SYNTAX score. The study findings suggest that the presence of any extent of CAD has no apparent impact on mortality after TAVI, whereas complex CAD has a negative prognostic impact in patients with severe AS undergoing TAVI. These results are in line with previous evidence from two observational cohort studies that applied the SYNTAX score to quantify CAD extent and complexity in TAVI patients (Figure 1). In a retrospective analysis of 445 patients from the Bern TAVI registry, higher baseline SYNTAX scores (>22 prior to coronary revascularisation performed in the setting of TAVI) as well as higher residual SYNTAX scores (>14 at the time of TAVI) were associated with significantly increased risks of cardiovascular mortality, stroke and myocardial infarction at one year8. In a cohort study of 263 patients undergoing TAVI at the Erasmus Medical Center in Rotterdam, a revascularisation strategy based on Heart Team decisions was associated with favourable clinical outcomes10. Specifically, patients with incomplete revascularisation with a median residual SYNTAX score of five (interquartile range: 0.13 to 9.88) had survival rates comparable to those with complete revascularisation at one year (77.4% vs. 79.9%, p=0.85), suggesting that a judiciously incomplete revascularisation strategy may suffice in TAVI patients with CAD10.
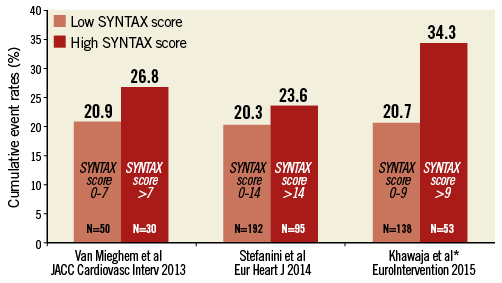
Figure 1. One-year all-cause mortality after TAVI according to residual SYNTAX score. Residual SYNTAX score cut-off used in each different study is indicated on the relative column. Number of patients included per group is specified at the bottom of each column. All studies applied the Kaplan-Meier method to calculate cumulative event rates. *For the purpose of the SYNTAX score stratification, Khawaja et al included patients with no CAD in the low SYNTAX score group, whereas Van Mieghem et al and Stefanini et al included only patients with CAD in the low SYNTAX score group.
Khawaja and colleagues9 went one step further, identifying a SYNTAX score of nine as the optimum cut-off point for predicting mortality, by the use of receiver operating characteristic curves. Patients with a SYNTAX score >9 had a higher risk of all-cause mortality as compared to those with a SYNTAX score ≤9 at 30 days (11.3% vs. 3.7%) and at one year (34.3% vs. 20.7%, p=0.005). This suggests that a SYNTAX score greater than nine might represent a target for revascularisation prior to TAVI in order to reduce the risk of ischaemic events after TAVI.
Taken together, the available observational evidence consistently indicates that complex CAD is associated with impaired clinical outcomes in TAVI patients, who might benefit from a selective revascularisation strategy based on Heart Team decisions with the aim of reducing the burden of disease. It remains to be determined, however, whether there is a causal relationship between residual CAD and mortality after TAVI. Future trials, such as the ongoing ACTIVATION11, will certainly shed more light on the optimal management of CAD in TAVI patients. For the time being, the study by Khawaja and colleagues further supports the current guidelines of the European Society of Cardiology12 which recommend percutaneous coronary revascularisation of proximal stenosis in major epicardial vessels in patients with significant CAD undergoing TAVI.
Conflict of interest statement
G. Stefanini has received speaker/consultant fees from Abbott Vascular, AstraZeneca, Biotronik, and The Medicines Company. C. Panico has no conflicts of interest to declare.