Introduction
Percutaneous coronary intervention (PCI) has evolved from femoral arterial access predominance to radial arterial access. Despite the widespread use of the radial and femoral approaches, there remains a small but consistent subgroup of patients in whom the brachial approach is still chosen1. The study hypothesis was that, although clinical outcomes of patients undergoing PCI using brachial access might be inferior to other access sites, in procedures utilising brachial access undertaken by default radial operators clinical outcomes might be similar to procedures utilising femoral access.
Methods
Study design and participants
We analysed data from the British Cardiovascular Intervention Society (BCIS) National PCI Audit of all patients undergoing PCI in the UK between 2006 and 2017 (study consort flow in Supplementary Figure 1). The study was approved by the National Institute for Cardiovascular Outcomes Research (NICOR) ethics committee. The final study population consisted of 861,773 PCI procedures. Study definitions were used as in the BCIS National PCI Audit (available at https://www.bcis.org.uk/resources/bcis-ccad-database-resources/datasets-history/). The clinical outcomes of interest were in-hospital mortality, major adverse cardiac and cerebrovascular events (MACCE), major bleeding, emergency coronary artery bypass surgery (CABG) or repeat PCI, acute coronary procedural complications, and access-site complications (Supplementary Appendix 1).
Data analyses
Statistical analysis was performed using the R coding environment (Open Source, RStudio version 3.5.1; RStudio, Boston, MA, USA). We tested for associations between each categorical variable and access site using a chi-squared test, and for continuous variables using the Wilcoxon-Mann-Whitney test. Multiple imputations were carried out using the Multivariate Imputation by Chained Equations (mice) package to reduce the potential bias from missing data (Supplementary Table 1). We performed an analysis of the predictors of access site using multivariate inverse probability of treatment weighting (IPTW) analysis (Supplementary Appendix 2). .We examined the influence of brachial access on PCI outcomes using the IPTW-adjusted model to investigate the independent odds of adverse outcomes by access site. Using the same methodology, we performed a sensitivity analysis on default radial operators (defined as having performed more than 75% of their cumulative procedures through radial access) and for the most recent study years (2013-2017)(Supplementary Figure 2)2.
Results
Temporal changes in brachial access site choice for PCI between 2006 and 2017
In total 1,133 procedures were undertaken from the brachial artery (0.13%). Annual numbers of brachial access increased through the study period, driven by an increase in overall PCI volume (Central illustration, left panel).
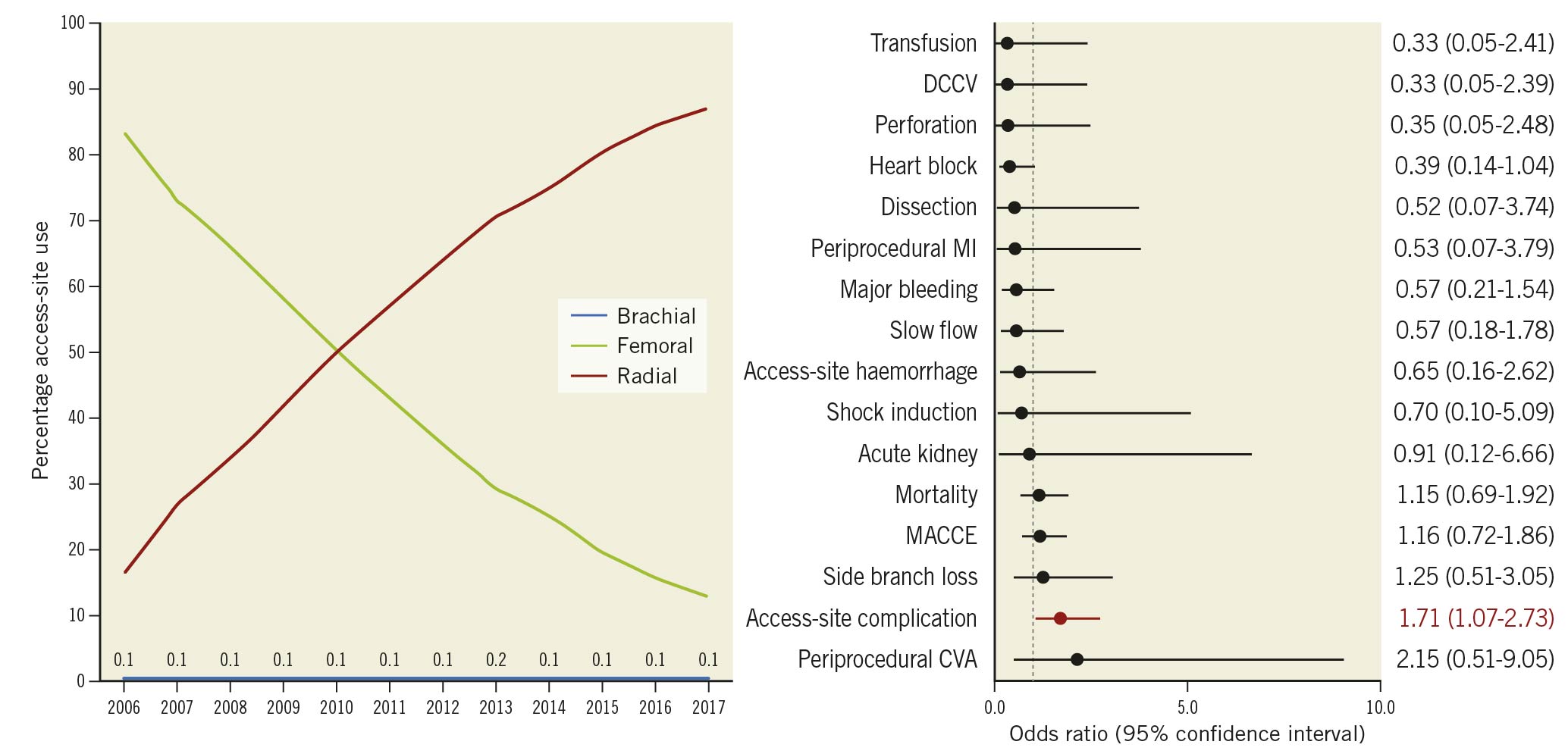
Central illustration. Access site changes and brachial artery predictors. Left panel: temporal changes in access site for PCI in the United Kingdom 2006-2017. Right panel: IPTW weight-adjusted procedural and clinical outcomes of brachial access procedures compared to femoral access in default radial operators for PCI in the United Kingdom 2006-2017.
Baseline demographics and procedural details by access site
In comparison to both radial and femoral access, those patients treated using brachial access were older, and had significantly greater baseline comorbidity (Supplementary Table 2). In comparison to radial access, patients treated using brachial access were more likely to present with stable angina, to have undergone previous CABG, and to present in cardiogenic shock (Supplementary Table 2). Brachial access for PCI was also associated with characteristics representing PCI complexity compared to femoral and radial access, including greater baseline disease severity, left main and chronic total occlusion (CTO)-PCI (Supplementary Table 3). Baseline demographics, and procedural details for brachial and femoral cases undertaken by default radial operators are presented in Supplementary Table 4 and Supplementary Table 5.
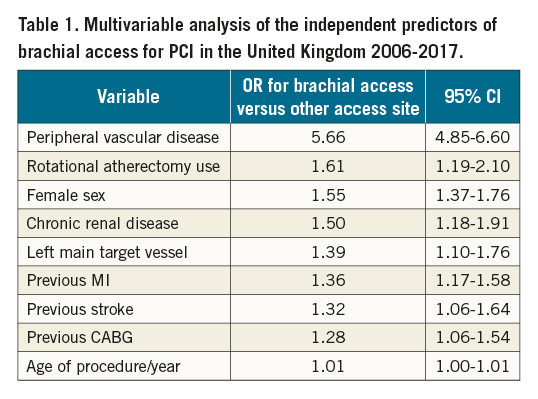
Independent associates of brachial access use for PCI from 2006 to 2017
The independent predictors of brachial access use for PCI are presented in Table 1. The strongest independent associates of brachial access included peripheral vascular disease, rotational atherectomy, female sex, chronic renal disease, left main target vessel and age per year.
Clinical outcomes by access site for PCI from 2006 to 2017
Crude unadjusted procedural and clinical outcomes are presented in Supplementary Table 6. After adjustment, brachial access remained strongly associated with adverse clinical outcomes compared to femoral access (Supplementary Figure 3, left panel). Similarly, in comparison with radial access, brachial access was associated with increased rates of these adverse outcomes but also increased rates of access-site haemorrhage and major bleeding (Supplementary Figure 3, right panel). The same associations were observed using multivariable logistic regression to adjust for baseline differences between groups (Supplementary Figure 4). In a sensitivity analysis for the study years 2013-2017 when radial access predominated as the default strategy, in a brachial versus femoral access comparison, there were no increased odds of MACCE associated with brachial access (Supplementary Figure 5). Within the group of patients who experienced an access-site vascular complication, the impact of this compared to patients without an access-site vascular complication on in-hospital outcomes was observed to be greater for patients in the brachial group (MACCE odds ratio [OR] 18.1, 95% confidence interval [CI]: 1.5-50.4, and mortality OR 35.0, 95% CI: 2.4-105.4) than in the femoral cohort (MACCE OR 2.5, 95% CI: 2.0-3.1, and mortality OR 2.6, 95% CI: 1.9-3.4), or radial cohort (MACCE OR 1.7, 95% CI: 1.2-2.3, and mortality OR 1.6, 95% CI: 1.1-2.4). In default radial operators, brachial arterial access was associated with similar IPTW weight-adjusted clinical outcomes to femoral access with only arterial complications observed to occur more frequently (OR 1.7, 95% CI: 1.1-2.7) (Central illustration, right panel).
Discussion
The current data suggest that brachial arterial access is used infrequently to facilitate PCI. Amongst the associates of its use identified in the predictive analysis, peripheral vascular disease predominates along with procedural factors consistent with large guide catheter use, including left main PCI and use of rotational atherectomy. These data would imply that brachial access is chosen as a bail-out option in patients without femoral access who have either small or absent radial arteries.
The existing evidence for brachial artery access for PCI is limited in contemporary practice. The only randomised trial of access site for PCI to include brachial artery use, the Randomized Comparison of Percutaneous Transluminal Coronary Angioplasty by the Radial, Brachial and Femoral Approaches: The Access Study, randomised 900 patients to radial, femoral or brachial access for PCI. Clinical outcomes were similar for all three groups and, although vascular access-site complications were more frequent in the femoral and brachial subgroups compared to the radial subgroup, the rates of vascular complications were similar between the femoral and brachial groups3. However, these data reflect the very early evolution of access-site practice for PCI and may not be relevant to current practice. In the current series, the observed vascular complication rate was 3.1%, a rate that is consistent with more contemporary case series published which report rates ranging from 2 to 8%4. These data also demonstrate that vascular complications occur more frequently with brachial access than with femoral or radial access.
The clinical outcomes of patients undergoing PCI using brachial access were also significantly worse than the radial and femoral cohorts. An excess of in-hospital death, stroke and access-site complications was observed compared to both cohorts, together with an excess of major bleeding and acute kidney injury compared to the radial cohort, perhaps driven by unmeasured comorbidity which could not be corrected for combined with an excess of access-site complications and of major bleeding. It is also interesting to note that a vascular complication from brachial access was associated with a greater impact on MACCE, compared to femoral and radial access-site complications, perhaps reflecting a combination of factors including significant underlying comorbidity and the nature of the vascular complication itself.
The most novel and noteworthy finding of the current study is that, when brachial access is undertaken by default radial operators, aside from a small excess of vascular complications, the clinical outcomes of these procedures were similar to the outcomes of femoral access procedures undertaken by default radial operators. Brachial artery access in such cases presumably reflects patients with small or non-patent radial arteries in whom femoral arterial access is complicated by peripheral arterial disease or other comorbidity.
Limitations
In considering the limitations of the present study, as with any database, the robustness of the conclusions is related directly to the quality of data entered. Secondly, the BCIS database does not capture sheath size and therefore the influence of this on the findings of the current study cannot be addressed. The current iteration of the BCIS data set does not capture the indication for access choice nor does it capture crossover; thus, we are unable to add further data on this aspect. Additionally, use of ultrasound to guide puncture is also not recorded. Finally, because of the observational nature of this study, any conclusions may be influenced by unmeasured confounders.
Conclusion
Patients undergoing PCI using brachial arterial access have significant comorbidity and undergo complex procedures. Although adjusted in-hospital clinical outcomes were significantly worse than in femoral or radial access cases, in default radial operators, clinical outcomes were similar between femoral and brachial access. Further studies are warranted.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.