Abstract
Background: Managing percutaneous coronary intervention (PCI) patients with atrial fibrillation (AF) presents challenges given that there are several potential antithrombotic therapy (ATT) strategies.
Aims: We examined ATT patterns, agreement between subjective physician ratings and validated risk scores, physician-patient perceptions influencing ATT and 1-year outcomes.
Methods: The AVIATOR 2 prospective registry enrolled 514 non-valvular AF-PCI patients from 11 sites. Treating physicians selected ATT and completed smartphone surveys rating stroke and bleeding risks, compared against CHA2DS2-VASc and HAS-BLED scores. Patients completed surveys regarding treatment understanding. Primary outcomes were 1-year major adverse cardiac or cerebrovascular events (MACCE: composite of death, myocardial infarction, definite/probable stent thrombosis, stroke, target lesion revascularisation) and actionable bleeding (Bleeding Academic Research Consortium 2, 3 or 5).
Results: The mean patient age was 73.2±9.0 years, including 25.8% females. Triple therapy (TT: 1 anticoagulant and 2 antiplatelet agents) was prescribed in 66.5%, dual antiplatelet therapy (DAPT) in 20.7% and dual therapy (1 anticoagulant+1 antiplatelet agent) in 12.8% of patients. Physician ratings and validated risk scores showed poor agreement (stroke: kappa=0.03; bleeding: kappa=0.07). Physicians rated bleeding-related safety (93.8%) as the main factor affecting ATT choice. Patients worried about stroke over bleeding (50.6% vs 14.8%). No group differences by ATT strategy were observed in 1-year MACCE (TT 14.1% vs dual therapy 12.7% vs DAPT 18.5%; p=0.25), or actionable bleeding (14.7% vs 7.9% vs 15.1%, respectively; p=0.89).
Conclusions: The AVIATOR 2 study is the first digital health study examining physician-patient perspectives on ATT choices after AF-PCI. TT was the most common strategy without differences in 1-year outcomes in ATT strategy. Physicians rated safety first when prescribing ATT; patients feared stroke over bleeding. ClinicalTrials.gov: NCT02362659
Introduction
Patients with atrial fibrillation (AF) undergoing percutaneous coronary intervention (PCI) represent 5-10% of the overall PCI population1. Despite improvements in contemporary stent technology, PCI patients typically require a short duration of antiplatelet therapy with aspirin and a P2Y12 receptor inhibitor to prevent stent related events in the early vascular healing period. In addition to antiplatelet therapy, anticoagulation is essential for stroke prevention in AF patients and is prescribed based on expected stroke risk2. Recent randomised trials comparing different antithrombotic strategies after AF-PCI have demonstrated the safety and efficacy of non-triple therapy (TT) options after PCI34567. Risk scores may aid in the prediction of future stroke and bleeding events and assist with decision-making on the optimal antithrombotic strategy in AF patients. The CHADS2 and CHA2DS2-VASc scores have been widely validated for stroke risk28, and HAS-BLED and ATRIA scores910 for risk of bleeding. Despite the availability of these scores, physicians may not routinely utilise them in busy clinical practice, rather relying on bedside assessment. Furthermore, these scores have not been validated in a large PCI population. In addition, patient values and preferences can impact the ultimate selection of antithrombotic regimens to ensure adherence over long-term follow-up.
Smartphone technology can assist with rapid assessment of physician and patient perceptions at point-of-care after PCI. Although research studies have examined the actual prescription of anticoagulation in all-comer AF patients compared with expected anticoagulation usage based on risk scores11, no study has assessed physician perception and patient feedback at the time of index PCI.
The Antithrombotic strategy variability in ATrial fibrillation and obstructive coronary disease revascularized with PCI (AVIATOR 2) international study is a prospective multicentre observational study of AF patients undergoing PCI, utilising a custom-built smartphone application (Health Promise Survey) at the time of index PCI with follow-up of clinical outcomes to 1 year12. In this study, we examined (i) the patterns of ATT usage after AF-PCI and changes over follow-up, (ii) patient characteristics by ATT strategy, (iii) agreement between subjective physician-rated risks and empiric estimates of risk, (iv) self-reported patient concerns and physician-rated clinical factors with respect to provision of ATT and (v) 1-year clinical events.
Methods
The AVIATOR 2 Registry is an international prospective multicentre observational study of patients with AF undergoing PCI12. The study was conceived by the global principal investigator with the steering committee and coordinated by the Icahn School of Medicine at Mount Sinai. The study was conducted according to the international guidelines of Helsinki and Good Clinical Practice. The ethics committees at each participating site approved the site protocol, and all enrolled patients provided written informed consent. Partial funding support was received from Bristol-Myers Squibb; however the funding source had no role in data analysis, interpretation or results reporting.
Study patients and set-up
Patients with a history of AF undergoing PCI were eligible for enrolment in the study. The study design and eligibility criteria have been previously published12. In the early enrolment period between June 2015 and August 2016, the main exclusion criteria were valvular AF as well as significant renal insufficiency (estimated glomerular filtration rate [eGFR] <30 ml/min/1.73 m2 or need for dialysis) and prior stroke, which limit the choice of potential ATT combinations. Due to slow enrolment, the eligibility criteria were broadened in August 2016, removing the last 2 exclusion criteria. The steering committee decided to stop study enrolment in November 2017, after 514 patients were enrolled in the study, due to slow enrolment and lack of funding support.
The study was conducted across 11 international sites: 5 in the United States, 4 in Italy, 1 in Germany, and 1 in Greece (Supplementary Table 1). The principal investigators at all sites were experienced clinical researchers and all sites had a dedicated research team to facilitate enrolment in the registry. Monitoring of patient data was done remotely by the clinical coordinating centre at the Icahn School of Medicine at Mount Sinai.
Smartphone surveys
Smartphone surveys were completed at point-of-care after PCI by physicians and participating patients, as previously described12 (Supplementary Figure 1). For each patient, physicians completed a questionnaire indicating perceived risk of stroke and bleeding on a 5-point Likert scale and factors contributing to the selection of discharge ATT. Patient surveys provided information on perceived concerns linked with their diagnosis and agreement on the need for prescribed medications12.
All data were recorded in a dedicated electronic database capture system developed and maintained in the Mount Sinai School of Medicine.
Clinical outcomes
The primary outcomes were 1-year major adverse cardiac and cerebrovascular events (MACCE: composite of all-cause death, myocardial infarction [MI], definite/probable stent thrombosis, stroke, target lesion revascularisation) and major actionable bleeding (Bleeding Academic Research Consortium [BARC] 2, 3 or 513). All ischaemic endpoints were adjudicated using the Academic Research Consortium guidelines14. MI was adjudicated using the Third Universal definition15.
We included all events reported by patients, and triggered by research staff at the sites, based on haemoglobin drop or admission to hospital, for adjudication by an independent clinical events committee.
Data analysis
Antithrombotic strategies were categorised as TT (1 anticoagulant+2 antiplatelet agents), dual antiplatelet therapy (DAPT) and dual therapy (1 anticoagulant+1 antiplatelet agent). Baseline characteristics and clinical outcomes between these groups were compared. We calculated CHA2DS2-VASc score for stroke risk2 and HAS-BLED score for bleeding risk in all patients9. Categorical data are reported as numbers and percentages and compared across the ATT groups using the chi-square test. Continuous data are reported as means and standard deviations and compared using the Student’s t-test. One-year clinical outcomes are presented in a time-to-event manner using Kaplan-Meier curves and compared across groups using the log-rank test.
Smartphone survey data for physician and patient perceptions are reported with frequencies of responses in each category. We correlated physician-rated risks via the smartphone survey with the validated CHA2DS2-VASc score for predicted stroke risk and with the HAS-BLED score for predicted bleeding risk. Agreement between the physician-rated risks and validated scores is reported.
We used logistic regression methods to explore predictors of triple therapy at discharge and to examine associations between physician-perceived risk or empirical scores and 1-year clinical events.
All analyses were performed using SAS, version 9.4 (SAS Institute).
Results
Over the study period, a total of 514 AF-PCI patients were enrolled, and ATT strategy could be accurately reported in 508 patients. The median follow-up was 365 (353-365) days. Figure 1 shows the patterns of ATT use. TT was used in 66.5% (n=338), dual therapy in 12.8% (n=65) and dual antiplatelet therapy in 20.7% (n=105) of patients at the time of discharge. In the TT group, use of vitamin K antagonists (VKA) and non-VKA (NVKA) was similar (45.9% and 54.1%, respectively), whereas in dual therapy patients NVKA use was greater (27.7% VKA vs 72.3% NVKA), and no anticoagulant was used in the DAPT group (p<0.001). Clopidogrel was the most common P2Y12 inhibitor used in all groups. Aspirin was used in 100% of DAPT and triple therapy patients but only in 3.1% of the dual therapy group.
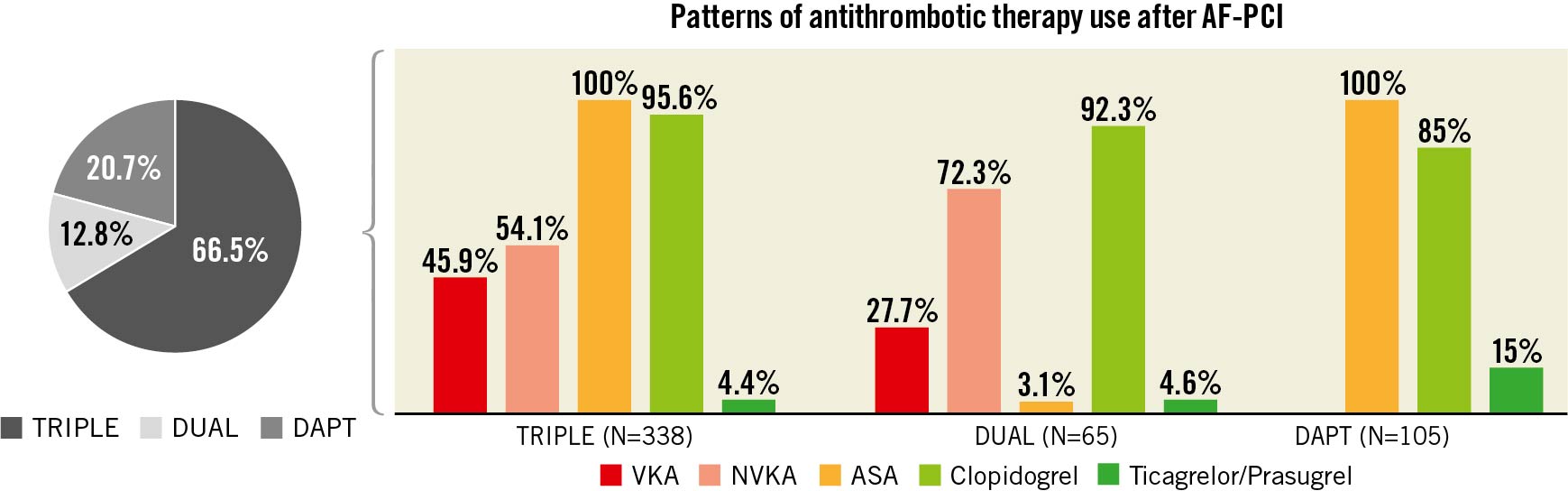
Figure 1. Prescription patterns of antithrombotic therapies after PCI in patients with atrial fibrillation. Antithrombotic strategies were categorised as triple therapy (1 anticoagulant+2 antiplatelet agents), dual therapy (1 anticoagulant+1 antiplatelet agent) or DAPT (dual antiplatelet therapy). AF: atrial fibrillation; ASA: acetylsalicylic acid; NVKA: non-vitamin K antagonist; PCI: percutaneous coronary intervention; VKA: vitamin K antagonist
Table 1 shows the baseline characteristics and Table 2 shows the procedural characteristics of patients treated with the 3 different ATT strategies.
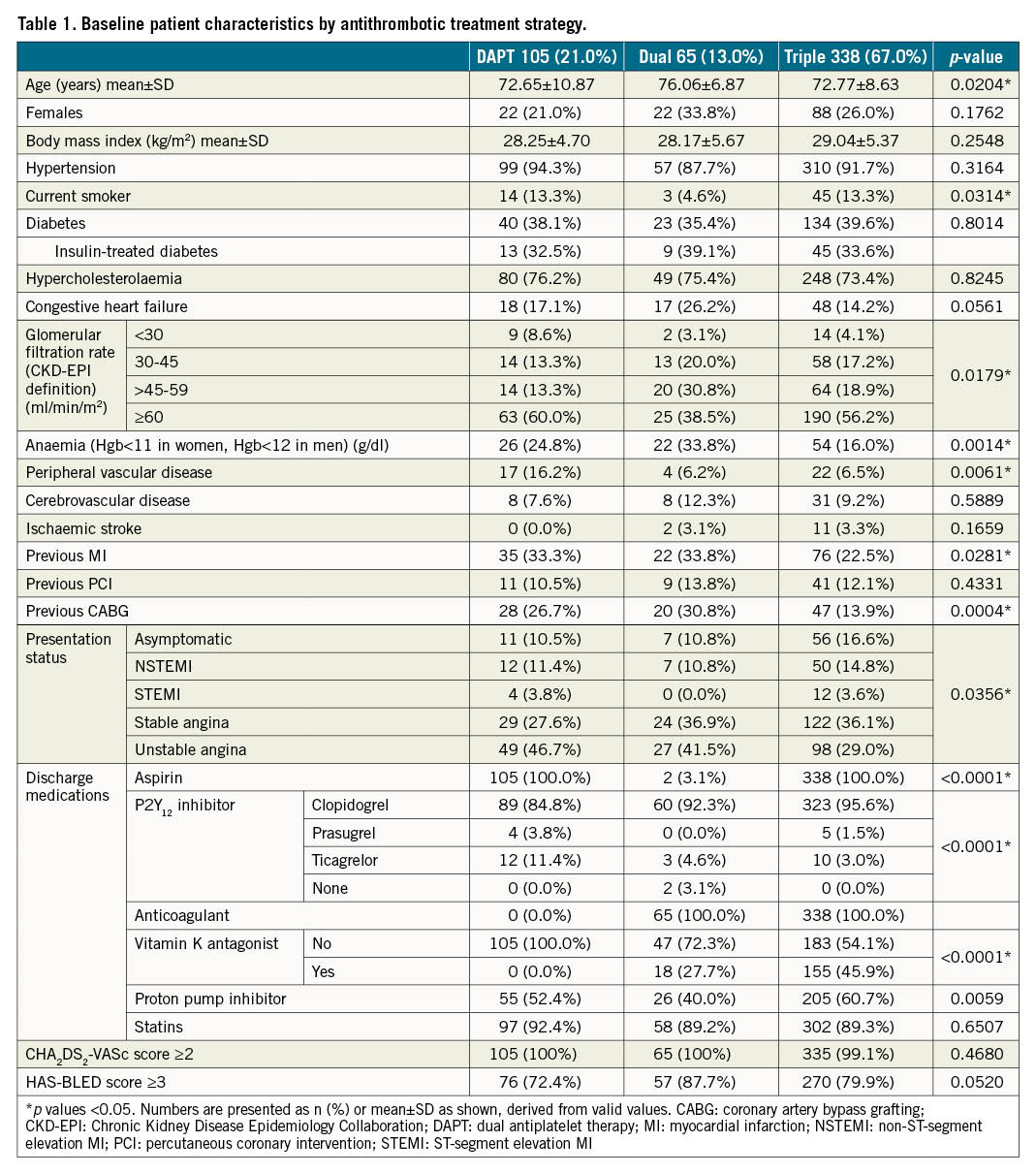
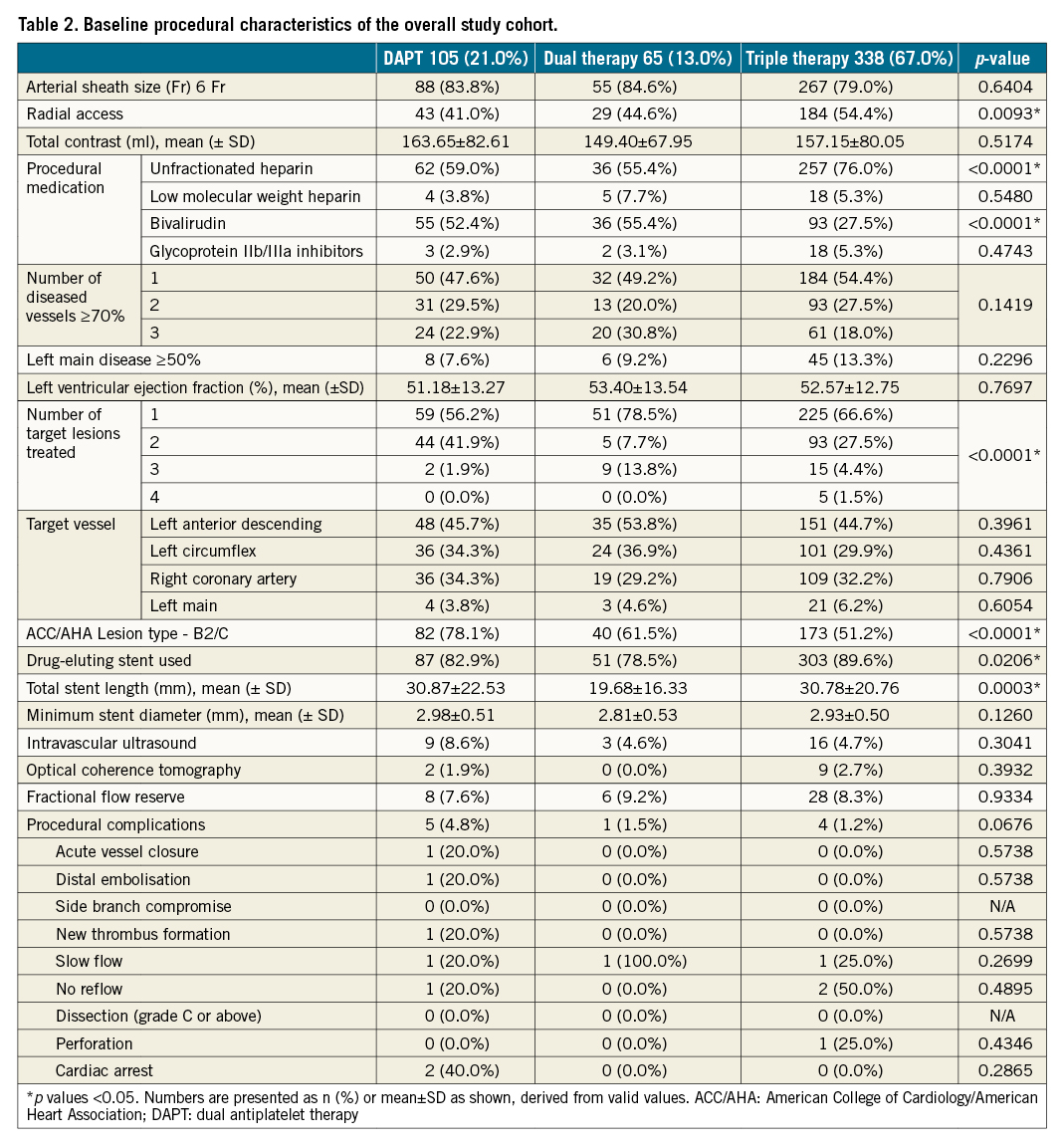
The mean age of enrolled patients was 73.2±9.0 years, and 25.8% were females. Patients on dual therapy were older than the others with a higher prevalence of chronic kidney disease (CKD) (eGFR <60ml/min/1.73m2), prior coronary artery bypass grafting (CABG), anaemia (haemoglobin <11 g/dl in women and <12 g/dl in men), and a lower prevalence of current smokers. DAPT patients had a higher prevalence of peripheral arterial disease (PAD), and DAPT and dual therapy patients had a higher prevalence of prior MI. The mean CHA2DS2-VASc score was 4.23±1.32 and the mean HAS-BLED score was 2.99±0.7 in the overall sample. There were no statistical differences in CHA2DS2-VASc and HAS-BLED scores between patients discharged on the different ATT strategies, although qualitative differences were noted. The rate of procedural complications was low, with no difference between the different ATT groups.
In a multivariable model for predictors of TT versus other strategies at discharge we considered baseline imbalances including age, sex, current smokers, congestive heart failure, eGFR, prior MI, prior CABG, PAD, CAD presentation, radial access, number of lesions treated, B2/C type lesion and stent type (drug-eluting stent [DES] vs other). The final model for predictors of TT versus other strategies at discharge is shown in Supplementary Table 2. DES implantation increased the odds of TT use, whereas B2/C type coronary lesions decreased the odds, and PAD was associated with a trend for lower odds of TT use.
Adherence to the original ATT strategy prescribed decreased over time, regardless of the initial strategy selected, predominantly guided by physicians in follow-up (Figure 2). Among patients discharged on TT, 91% remained on TT at 30 days, 43% at 6 months and 35% at 1 year, with a major decrease in acetylsalicylic acid (ASA) usage (50.6% use at 6 months and 40.3% at 1 year).
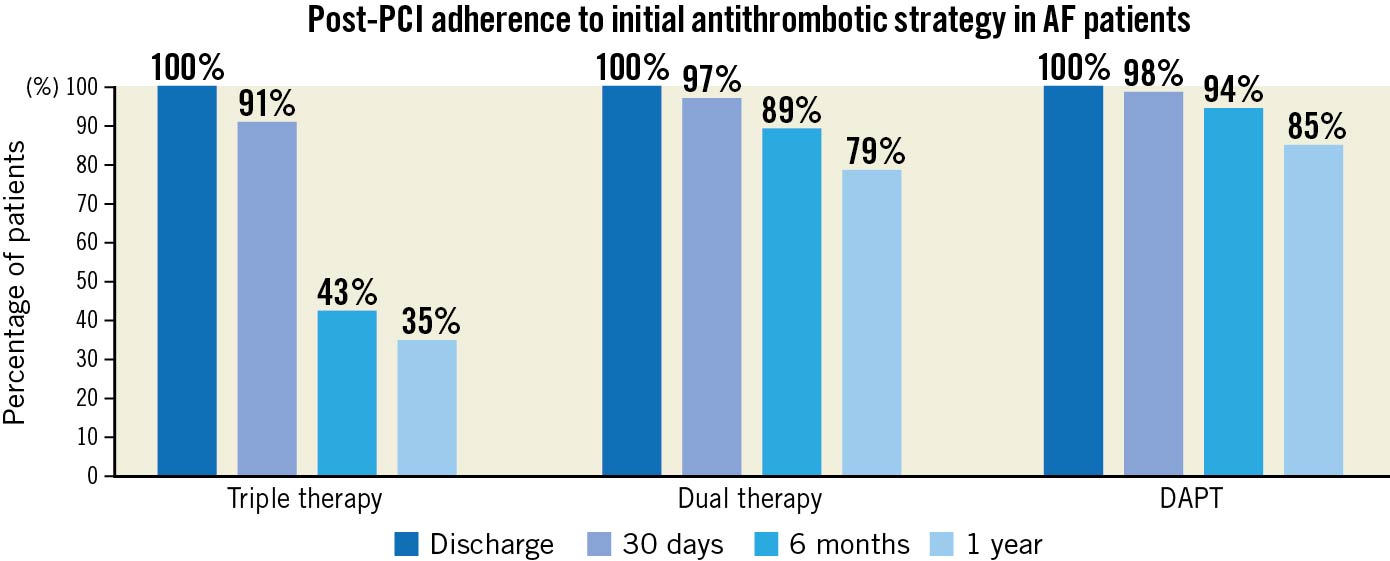
Figure 2. Temporal changes in adherence to initial antithrombotic strategy during follow-up. AF: atrial fibrillation; DAPT: dual antiplatelet therapy; PCI: percutaneous coronary intervention
Overall agreement between physician ratings and CHA2DS2-VASc score for stroke risk was poor, weighted kappa statistic=0.03. Analogously, agreement between physician ratings and HAS-BLED score for bleeding risk was poor, weighted kappa statistic=0.07. Among patients with CHA2DS2-VASc ≥2, clinicians perceived 41.1% as high or very high risk, and among patients with HAS-BLED ≥3, clinicians perceived 29% as high or very high bleeding risk (Figure 3).
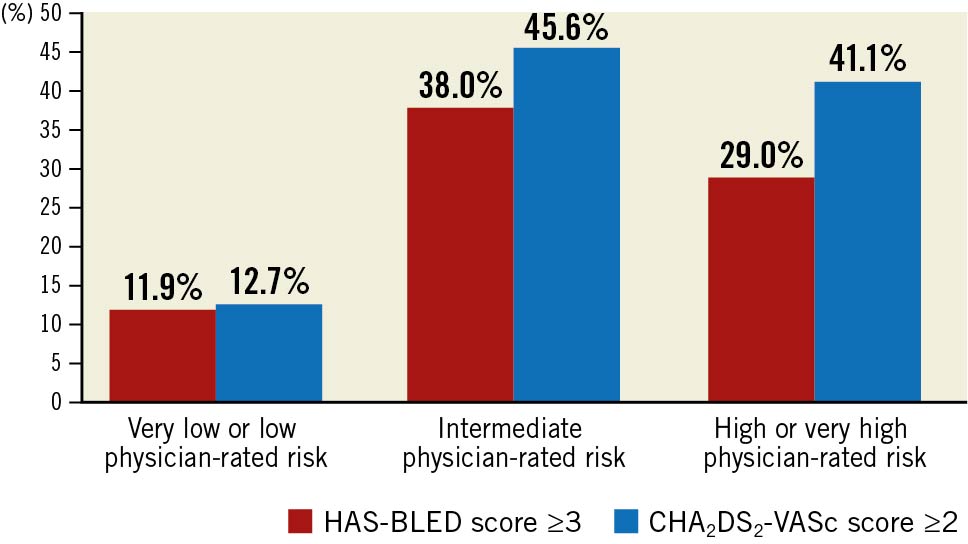
Figure 3. Distribution of (a) physician-rated stroke risk in AF-PCI patients with CHA2DS2VASc score ≥2, and (b) physician-rated bleeding risk in AF-PCI patients with HAS-BLED Score ≥3. AF: atrial fibrillation; PCI: percutaneous coronary intervention
Physicians reported using the CHA2DS2-VASc score more often than HAS-BLED during decision-making for ATT. Physicians also most frequently considered safety (93.8%) and efficacy (89.9%) as the main factor for decision-making on ATT. Other factors including drug availability (3.9%), familiarity (6.2%), cost (2.5%) or dosing frequency (2.5%) were less often considered most relevant. Patient survey responses showed that most patients agreed with the importance of their prescribed ATT (62.8% completely agreed, 30.2% mostly agreed). With respect to future adverse events patients were most concerned about the risks of MI, stroke or death and were less concerned about the risks of bleeding, frequent blood testing or stent failure (Central illustration). Physician and patient perceptions by the ATT group strategy are shown in Supplementary Table 3.
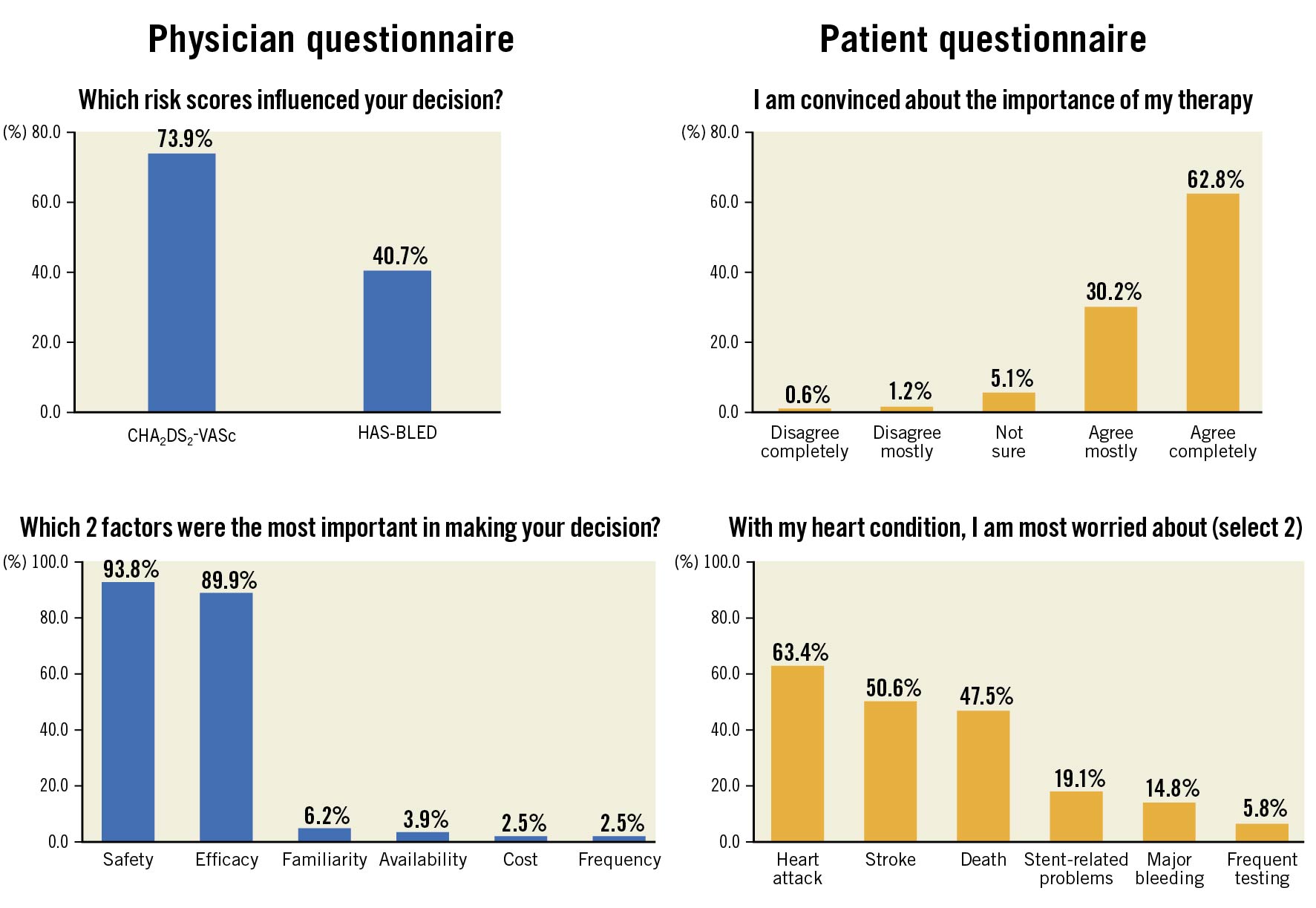
Central illustration. Physician and patient perceptions regarding use of antithrombotic therapy derived from smartphone survey responses in the overall patient sample
Table 3 and Figure 4 show the 1-year clinical outcomes. No significant differences were noted for 1-year MACCE or major bleeding. One-year MACCE occurred in 15.3% and BARC 2, 3 or or 5 major actionable bleeding in 13.8% of patients overall. There were no group differences in MACCE (14.1% with TT vs 12.7% with dual therapy vs 18.5% with DAPT; p=0.25), or major actionable bleeding (14.7% vs 7.9% vs 15.1%, respectively; p=0.89).
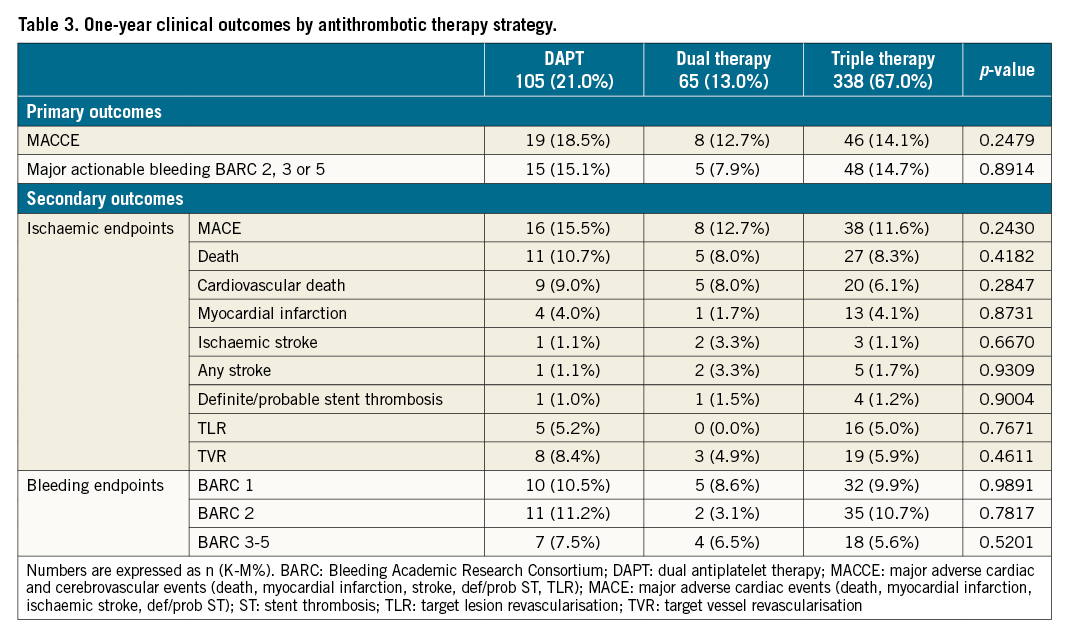
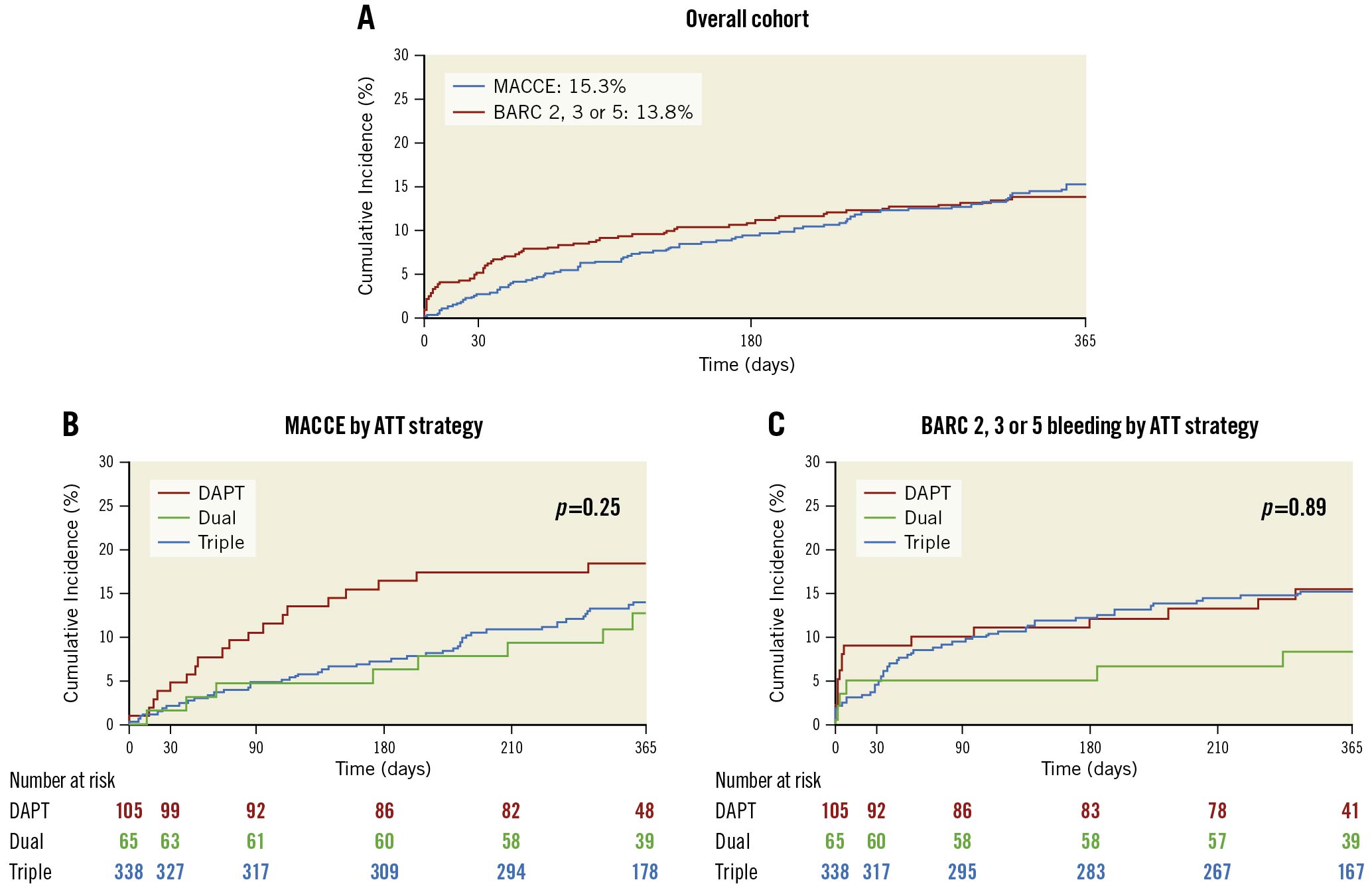
Figure 4. Cumulative incidence of 1-year primary outcomes in the overall cohort and by antithrombotic therapy strategy. ATT: antithrombotic therapy; BARC: Bleeding Academic Research Consortium; DAPT: dual antiplatelet therapy; MACCE: major adverse cardiac and cerebrovascular events
Figure 5 shows the incidence of 1-year clinical events (MACCE or major actionable bleeding) by physician-perceived risk and calculated scores.
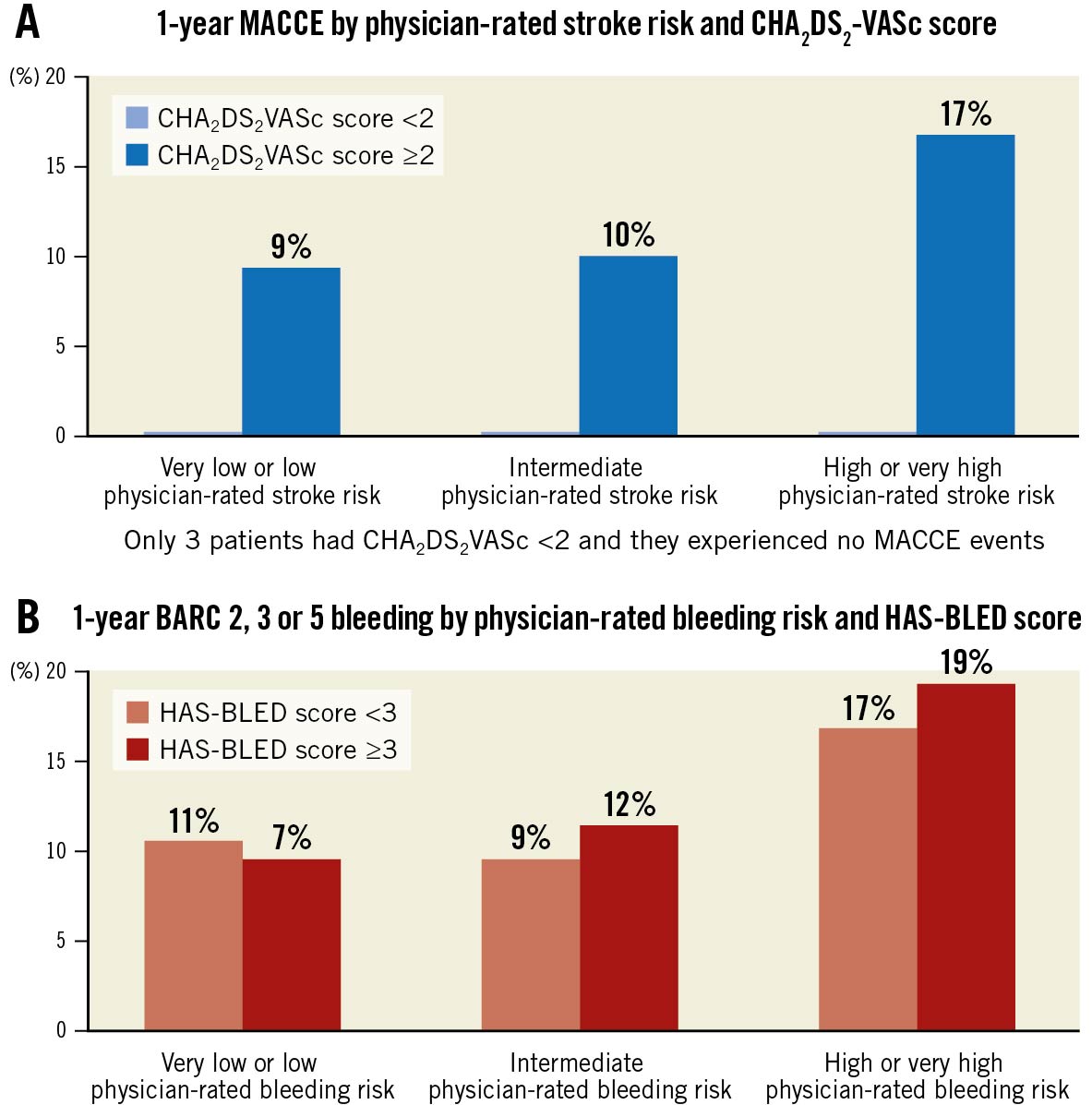
Figure 5. Incidence of 1-year clinical events (MACCE or major actionable bleeding) by physician-perceived risk and calculated scores. BARC: Bleeding Academic Research Consortium; MACCE: major adverse cardiac and cerebrovascular events
For ischaemic events, increasing physician-perceived ischaemic risk (odds ratio [OR] 1.52, 95% confidence interval [CI]: 1.07-2.16; p=0.019; area under the curve [AUC] 0.59) and CHA2DS2-VASc score (OR 1.29, 95% CI: 1.06-1.57; p=0.011; AUC 0.59) were moderately discriminatory for increased risk of MACCE. In a multivariable model adjusted for age, sex and body mass index, both physician-perceived ischaemic risk and CHA2DS2-VASc score were associated with a trend for greater risk of MACCE (Supplementary Table 4).
For bleeding events, increasing physician-perceived bleeding risk (OR 1.39, 95% CI: 1.03-1.89; p=0.034; AUC 0.58) but not HAS-BLED score (OR 1.07, 95% CI: 0.75-1.54; p=0.70; AUC 0.51) was moderately discriminatory for increased risk of major actionable bleeding. In a multivariable model adjusted for age, sex and body mass index, increasing physician-perceived bleeding risk and not HAS-BLED score was associated with a greater risk of major actionable bleeding (Supplementary Table 4).
Discussion
The AVIATOR 2 international study is the first digital health study to analyse physician preferences and patient perspectives at point-of-care in AF patients undergoing PCI. The main findings of this analysis are as follows: 1) triple therapy was the most common strategy used at discharge after AF-PCI, in 66.5% of patients, followed by DAPT in 20.7% and dual therapy in 12.8%. However, de-escalation of TT over time was common, primarily driven by the discontinuation of ASA, thus shifting the majority of TT patients to a dual strategy; 2) subjective perceptions of both ischaemic and bleeding risks by clinicians were poorly calibrated with empiric estimates of the same; 3) physicians rated safety most highly followed by efficacy in decision-making of ATT, whereas patients expressed greater concern regarding risk of stroke and MI rather than bleeding; 4) 1-year MACCE occurred in 15.3%, and BARC 2, 3 or 5 major actionable bleeding in 13.8% of patients without statistically significant differences in clinical outcomes between the ATT groups.
We noted that 78% of patients in the current study were discharged on an anticoagulant and the most common strategy was TT in two-thirds of patients followed by DAPT and dual therapy. Dual therapy combinations utilised higher rates of NVKA, rather than VKA, and very low rates of aspirin. Significant baseline differences were noted in patients across the 3 ATT strategies, with greater clinical comorbidities in the dual therapy group with respect to age, CKD, anaemia, prior PCI and CABG. Procedurally, however, the rate of radial access was lower with fewer complex lesions, greater use of bare metal stents, and lower use of proton pump inhibitors in dual therapy patients. Validated scores did not appear to impact decision-making on ATT use after PCI, with no differences in calculated scores between the groups. Importantly, though, our study demonstrates temporal changes in ATT strategy following AF-PCI with de-escalation of TT in keeping with contemporary guidelines. The greatest change occurred in patients receiving TT, with aspirin discontinuation occurring in over 50% of patients by 6 months. These results are consistent with recent consensus statements supporting a limited duration of TT in such patients to minimise comorbidity related to bleeding16.
We noted a significant discrepancy between validated scores and physician ratings for stroke and bleeding in the current study cohort. Prior research comparing physician and objective assessments for stroke in AF patients has shown similar discordance11. Steinberg et al also showed that physician determination of bleeding risk was not aligned with calculated ATRIA bleeding scores, albeit we did not report on this score in the current analysis11. In general, physicians place greater emphasis on bleeding over stroke risk and may avoid anticoagulation to minimise major or fatal bleeding outcomes17. However, anticoagulants may also be inadvertently avoided due to incorrect determination of stroke risk18. These results highlight a lack of adequate calibration between subjective and empiric estimates of ischaemic and bleeding risk. Integrating decision-support tools within electronic health records is one strategy that might improve decision-making and clinical outcomes19.
Conversely to our findings, prior studies have shown anticoagulant undertreatment in nearly 50% of patients with AF, which is a major concern2021 since undertreatment can result in greater stroke and mortality22. In our study survey, while physicians rated the need for both safety and efficacy highly in their prescription practices, patients were more concerned about ischaemic rather than bleeding risk. Approximately 50% of patient responses expressed concern regarding stroke risk, compared with 15% of responses expressing concern regarding the risk of bleeding and 6% of responses regarding the need for frequent blood tests. These results suggest that clinical priorities are not always aligned with patient values and preferences, and emphasise the need for shared decision-making in such patients.
With respect to clinical outcomes, the incidence of bleeding and ischaemic events was similarly high in this cohort, occurring in approximately 1 in 7 to 1 in 8 patients. These observed bleeding rates are in keeping with results from randomised trials. Moreover, our results confirm the susceptibility of AF-PCI patients to both ischaemic and bleeding adverse outcomes4567, emphasising the scope of the problem and the need for tailored treatment regimens. Despite the lack of statistical differences and within the limitations of a small sample size, it may be noteworthy that 1-year major bleeding events were numerically lower in the dual therapy group without an increase in ischaemic outcomes.
In exploratory models, physician-perceived ischaemic and bleeding risk as well as CHA2DS2-VASc score were moderately discriminatory for clinical events in our cohort, whereas HAS-BLED score was not, suggesting the need for customised approaches and discussion, combining clinical expertise and risk scores but not relying on the latter alone.
Limitations
AVIATOR 2 was an observational study with limitations inherent to the study design. Treatment was at the discretion of the managing physician. The observational registry design of the study results in enrolment bias, and, as such, study findings should be considered exploratory and hypothesis-generating. The results of the current analysis are impacted by the small sample size secondary to slow recruitment and the study was thus underpowered to show differences in clinical outcomes between the groups compared. Premature interruption of the study precluded enrolment of the desired patient numbers per the statistical design limiting the power to report on the hypothesis. In addition to patient reported events, we reported research staff and clinical events committee triggered events based on hospital presentation or drop in haemoglobin, however events may be under-reported. One-year triple therapy is not the standard-of-care after PCI. At the time of study design randomised trial data were not available. The results from major randomised trials analysing ATT strategies were not available at the time of enrolment (except for PIONEER-AF), which today have a significant influence on decision-making regarding ATT prescriptions in AF-PCI patients. The study remains novel however, in reporting patient and physician factors relevant to antithrombotic prescription and the mismatch between subjective physician risk assessment and objective empiric risks for stroke and bleeding.
Conclusions
The AVIATOR 2 study is the first digital health real-world study to examine physician and patient perspectives at point-of-care and choice of ATT in patients with atrial fibrillation undergoing PCI. Triple therapy was the most common discharge strategy after AF-PCI, followed by DAPT and dual therapy; and de-escalation of triple therapy in follow-up was high. Despite baseline differences between the ATT groups there were no significant differences in clinical outcomes up to 1 year. Agreement between physician-assessed risks and CHA2DS2-VASc and HAS-BLED scores was modest. Physicians rated safety first when prescribing ATT, whereas patients feared stroke more than bleeding. These results highlight the mismatch between physician-perceived and calculated risks, as well as emphasising the importance of shared decision-making between physicians and patients. Dynamic risk stratification in follow-up after AF-PCI and a “patient-centred” approach is crucial to managing ATT beyond the early post-procedural period.
Impact on daily practice
The AVIATOR 2 study findings indicate the patterns of antithrombotic therapy usage in clinical practice after non-valvular AF-PCI in recent years, prior to availability of major randomised trials, with triple therapy usage at discharge in 66.5% patients. Importantly, the study also demonstrates temporal changes in antithrombotic therapy strategy during follow-up. The greatest change occurred in patients receiving triple therapy, with aspirin discontinuation occurring in over 50% patients by 6 months. This study highlights the discrepancies between subjective physician ratings for stroke and bleeding assessed at point-of-care during index PCI and objective risk scores in non-valvular AF-PCI patients. The study underscores the mismatch in patient and physician concerns vis-à-vis stroke risk versus bleeding post-PCI. Shared decision-making and a patient-centred approach is required to ensure adherence.
Acknowledgements
The authors thank participating patients, physicians and research teams for their contributions to this study.
Guest editor
This paper was guest edited by Fernando Alfonso, MD; Hospital Universitario de La Princesa, Madrid, Spain.
Funding
Partial funding for this study was received from Bristol-Myers Squibb.
Conflict of interest statement
R. Mehran has received institutional research grant support from Eli Lilly/Daiichi Sankyo Inc., AstraZeneca, The Medicines Company, and Bristol-Myers Squibb. The other authors have no conflicts of interest to declare. The Guest Editor has no conflict of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.