A variety of catheter-based repair solutions are currently employed or in development to treat mitral valve regurgitation, the most common form of valvular heart disease globally. Such treatments aim to mimic surgical techniques - leaflet plication, annuloplasty, and neochordae placement. Commercially available devices include MitraClip® (Abbott Vascular, Santa Clara, CA, USA), Carillon® (Cardiac Dimensions, Kirkland, WA, USA), NeoChord (NeoChord, Inc., St. Louis Park, MN, USA), Mitralign (Mitralign, Inc., Tewksbury, MA, USA), and Cardioband (Edwards Lifesciences, Irvine, CA, USA). The MitraClip remains an outlier as the only widely studied device, including a large randomised controlled trial comparing it to surgical valve repair1. Other devices have demonstrated early safety with mortality rates of <5% among high-risk patients, but efficacy has not been definitively established. Indeed, residual mitral regurgitation (MR) remains a concern with all mitral repair devices; MR grade ≤2 is achieved in 45-90% of patients with secondary MR2.
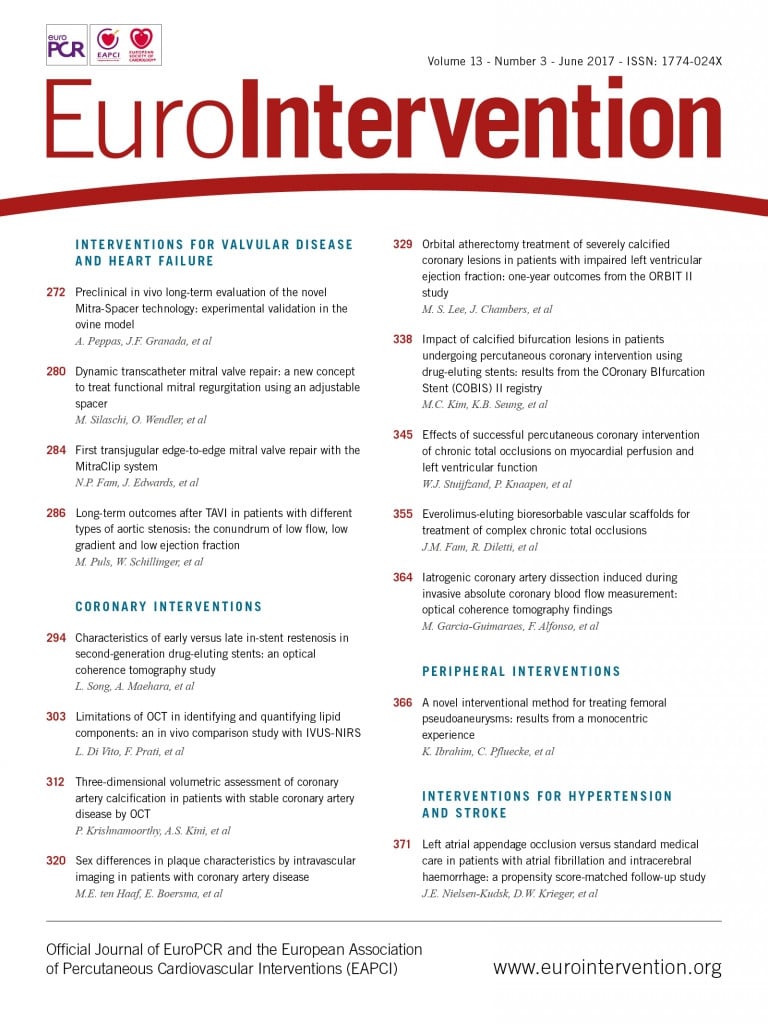
It is not unexpected that early human experiences with these devices have been suboptimal. The devices themselves are complex and require iteration; patient selection needs refinement, the patients selected are often futile, and the individual patient’s anatomy may not be best suited to a particular device; preoperative imaging assessment frequently provides more questions than answers; and the procedural technique itself is by definition untested in humans. Careful design, exhaustive bench testing, and animal studies can mitigate these obstacles. In this context, it is most interesting to read two articles in the current edition of EuroIntervention relating to the Mitra-Spacer™ (Cardiosolutions Inc., West Bridgewater, MA, USA) system.
The Mitra-Spacer consists of an apically tethered partially fluid-filled balloon for implantation in the mitral valve position that reduces the regurgitant orifice area and provides a surface for leaflet coaptation. Peppas and colleagues present the results of chronic ovine studies with the Mitra-Spacer system3.
All procedures were successfully performed with improvements in mitral parameters. At 90 days, however, four of seven euthanised sheep demonstrated thrombus on the shaft or balloon of the device, and five of seven had evidence of renal infarction, possibly due to systemic embolisation.
Silaschi and colleagues from King’s College Hospital London then report the first human implant of the Mitra-Spacer4.
The device was implanted on a compassionate basis in a young patient (58 years old) with severe functional MR and cardiac failure post recent myocardial infarction. The clinical impact of the procedure was impressive and, while clinically relevant device thrombosis necessitated explant at eight months (despite oral anticoagulation), the intervention afforded this critically ill patient a bridge to curative surgical mitral valve replacement.
These remarkable reports reflect a crucial dichotomy in the medical device innovation field: weighing the potential for harm against the potential for benefit. The Mitra-Spacer animal studies suggested feasibility but raised concerns of device thrombosis, which subsequently came to pass in the first human case. Nevertheless, the device may have saved the patient’s life. This brave soul has just reward for his courage in undergoing the procedure. The potential for harm was also seen in early studies of transcatheter aortic valve implantation (TAVI), with procedural mortality as high as 50%. A decade of device iteration, procedural refinement, improving operator experience, and imaging insights have, however, led to procedural mortality rates as low as 1-2% in contemporary TAVI series. Difficult choices are frequently encountered along the development pathway of transformative medical devices (such as bioresorbable scaffolds). Do we iterate, refine, develop, and change? Or cut and run? The medical device development process from conceptualisation to commercialisation is rarely straightforward. A complex, costly, and protracted pathway can be expected for most devices. This process requires rigour and strict adherence to ethical practices.
Peppas and colleagues should be congratulated for performing careful animal experimentation with the Mitra-Spacer and for publishing these results. Animal models rarely reflect the complexity of disease in humans, and designing robust translational experimental pathways for novel devices remains challenging. Nevertheless, animal experimentation with the Mitra-Spacer undoubtedly informed procedural technique for the first patient, while also highlighting the importance of anticoagulation and close post-procedural imaging follow-up in the case performed by Silaschi. These reports remind us of the importance of rigorous preclinical testing and the perils and possibilities of transformative medical devices.
Conflict of interest statement
The authors have no conflicts of interest to declare.