Abstract
Aims: Atherosclerosis accelerates with increasing age; however, young women presenting with acute coronary syndromes (ACS) have adverse outcomes compared to men despite less obstructive coronary artery disease. We sought to evaluate the in vivo plaque characteristics and composition of untreated non-culprit lesions (NCL) at two ages (<65 years old and ≥65 years old) in patients with ACS and examine the effect of sex in both groups.
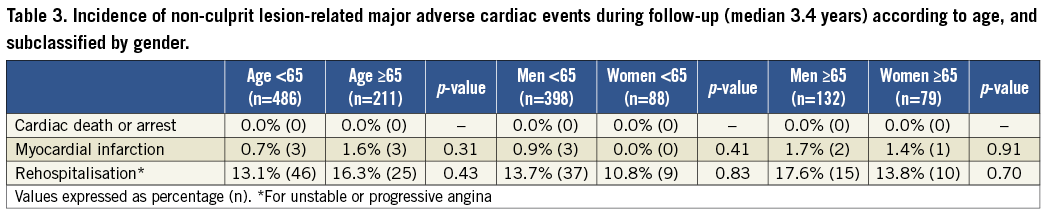
Methods and results: Untreated NCLs from 697 patients with ACS were imaged with greyscale and radiofrequency intravascular ultrasound. NCL plaque morphology, burden, composition, and major adverse cardiac events (MACE) were analysed in both age groups, and a posterior sex-based sub-analysis was performed. Plaques from patients ≥65 (n=974) vs. <65 (n=2,275) years old were longer (median 12.62 mm vs. 10.75 mm, p=0.008) and had greater plaque burden (48.2% vs. 47.5%, p=0.001), necrotic core (12.5% vs. 11.0%, p=0.001) and dense calcium (5.7% vs. 4.0%, p<0.0001). Men <65 years old also had a greater number of fibroatheromas (3.0 vs. 2.0, p=0.007) and NCLs per patient (5.0 vs. 4.0, p=0.004) with larger plaque volumes (47.7% vs. 46.8%, p=0.04), and fewer fibrotic plaques (2.2% vs. 4.4%, p=0.03) than women in the same age group. These sex differences were not observed in patients ≥65 years old. The incidence of MACE during median 3.4 year follow-up did not significantly differ according to age in this study.
Conclusions: The current study confirms in vivo that, with aging, plaque burden, necrotic core and calcium content increase significantly. Moreover, gender-specific differences in the extent and composition of coronary plaque are present in patients <65 years (but not ≥65 years) of age, which suggest differential sex-related effects on atherosclerosis development and progression.
Abbreviations
ACS: acute coronary syndrome
CAD: coronary artery disease
DC: dense calcium
FA: fibroatheroma
FF: fibro-fatty
FT: fibrous tissue
IVUS: intravascular ultrasound
MACE: major adverse cardiac events
MI: myocardial infarction
NC: necrotic core
NCL: non-culprit lesion
NSTEMI: non-ST-segment elevation myocardial infarction
PIT: pathological intimal thickening
PCI: percutaneous coronary intervention
STEMI: ST-segment elevation myocardial infarction
TCFA: thin-cap fibroatheroma
ThCFA: thick-cap fibroatheroma
UA: unstable angina
VH-IVUS: virtual histology intravascular ultrasound
Introduction
Advancing age is a major risk factor for symptomatic and silent atherosclerosis disease. In addition to the greater likelihood of other cardiovascular risk factors being present in the elderly, the aging process itself induces structural and functional changes in the vascular wall, including intimal thickening, increased arterial stiffness and endothelial dysfunction1. It has been suggested that plaque burden increases with advancing age2, but little is known about the impact of age on coronary plaque type and composition3. The pathophysiology, severity and clinical presentation of atherosclerosis also seem to differ between men and women throughout their different stages of life4-7. For instance, men continue to have more advanced coronary artery disease (CAD) at all ages8,9, although premenopausal women as compared to older women more frequently have plaques with greater cellular composition and lower lipid and calcium content which is more prone to erosion than rupture10,11. Younger women with acute coronary syndromes (ACS) have also been described as having an adverse short and long-term prognosis compared to men in the same age group12-15. Moreover, female sex and age <65 were both found to be independent predictors for clinical progression requiring percutaneous coronary intervention (PCI) of asymptomatic plaques previously not treated16. As has been noted17, a considerable number of questions regarding the sex-related differences in atherosclerosis as a function of age remain unanswered.
Traditional approaches for plaque characterisation - angiography and greyscale intravascular ultrasound (IVUS) - provide limited information about plaque morphology and composition. The addition of ultrasound-derived radiofrequency signal analysis (virtual histology [VH]–IVUS) enables a more detailed and accurate description of the atherosclerotic plaque components18. The use of these imaging modalities in the multicentre, prospective, international Providing Regional Observations to Study Predictors of Events in the Coronary Tree (PROSPECT) study provides a unique opportunity to analyse in vivo the differences in coronary plaque composition and prognosis of untreated non-culprit lesions (NCL) in men and women at two particular periods of life (<65 years old and ≥65 years old).
Methods
The PROSPECT study has been described in detail previously, including major inclusion and exclusion criteria, endpoints and definitions19. In brief, 697 patients with ACS (ST-segment elevation myocardial infarction beyond 24 hours [STEMI], non STEMI [NSTEMI], or unstable angina [UA]) undergoing PCI of one or two major epicardial coronary arteries underwent three-vessel multimodality intracoronary imaging (quantitative coronary angiography [QCA], greyscale IVUS imaging, and VH-IVUS; Volcano Corporation, San Diego, CA, USA) in order to prospectively characterise the proximal 6-8 cm of the coronary tree. Patients were enrolled (and imaging was performed) only after performance of successful and uncomplicated PCI of all coronary lesions responsible for the index event, and after completion of any other planned interventions. Exclusion criteria included serum creatinine >2.5 mg/dl, presentation with hypotension, shock or left ventricular ejection fraction <30%, left main coronary artery culprit lesion or necessity for PCI in all three major epicardial coronary vessels.
Angiographic qualitative and quantitative measurements were obtained for the entire coronary tree. All angiographic lesions with at least 30% visible diameter stenosis were analysed. An IVUS lesion was defined as at least three consecutive frames with a plaque burden of at least 40%. Such lesions were further classified by means of VH-IVUS as one of the following: thin-cap fibroatheroma, thick-cap fibroatheroma, pathological intimal thickening, fibrotic plaque, or fibrocalcific plaque. Each greyscale and VH-IVUS frame and lesion was co-registered to the angiographic roadmap using fiduciary branches for alignment, as previously described19,20. Plaque rupture was defined as a plaque ulceration with a tear detected in a fibrous cap. Percentage of plaque volume was calculated as {[total EEM volume (mm3) – total lumen volume (mm3)]/total EEM volume (mm3)} * 100.
The primary endpoint of interest in the PROSPECT study was NCL-related major adverse cardiac events (NC-MACE) defined as the composite of cardiac death, cardiac arrest, myocardial infarction, or rehospitalisation due to unstable or progressive angina. The study was approved by the institutional review board at each participating centre, and all patients signed a written informed consent.
Statistical methods
For the present analysis patients enrolled in PROSPECT were divided into two age groups (<65 years and ≥65 years), and then subdivided according to gender. Statistical analysis was performed with the use of SAS software, version 9.2 (SAS Institute, Cary, NC, USA). Continuous variables (expressed as median [IQR]) were compared using the Kruskal-Wallis test. Categorical variables (expressed as percentage) were compared using chi-square or Fisher’s exact test, as appropriate. A p-value <0.05 was considered statistically significant, and all p-values are two-sided.
Results
PATIENTS <65 YEARS OF AGE VS. PATIENTS ≥65 YEARS OF AGE
The demographic and clinical characteristics of the 697 patients according to age are shown in Table 1.The length of coronary tree analysed with greyscale IVUS was significantly longer in patients <65 compared to ≥65 years old (176.70 mm[137.65, 219.15] vs. 165.89 mm[120.63, 203.51], p=0.007), but no differences were found in the number or total length of NCLs per patient. Comparing younger to older patients, the percentage of plaque volume in the NCL segments was greater in the older group (49.0%[46.5, 51.9] vs. 49.7%[47.2, 52.9] respectively, p=0.01). VH-IVUS analysis also demonstrated a greater percentage of dense calcium volume (4.6%[2.6, 7.5] vs. 6.9%[3.6, 10.3], p<0.0001) and a lower percentage of fibrous tissue volume (60.3%[56.2, 64.6] vs. 58.0%[52.9%, 61.6], p=0.0001) in the non-culprit segments of patients ≥65 years old. The NCLs in older compared to younger patients were also longer and had greater plaque burden (Table 2). As in the case of non-culprit segments, significant variations were present in the components of the NCLs (Figure 1). NCLs in older patients were also more likely to be classified as thick-cap fibroatheromas (ThCFA) (Table 2). No differences were observed in the rates of NCL-associated MACE incidence during the median 3.4 years follow-up period as a function of age (Table 3).
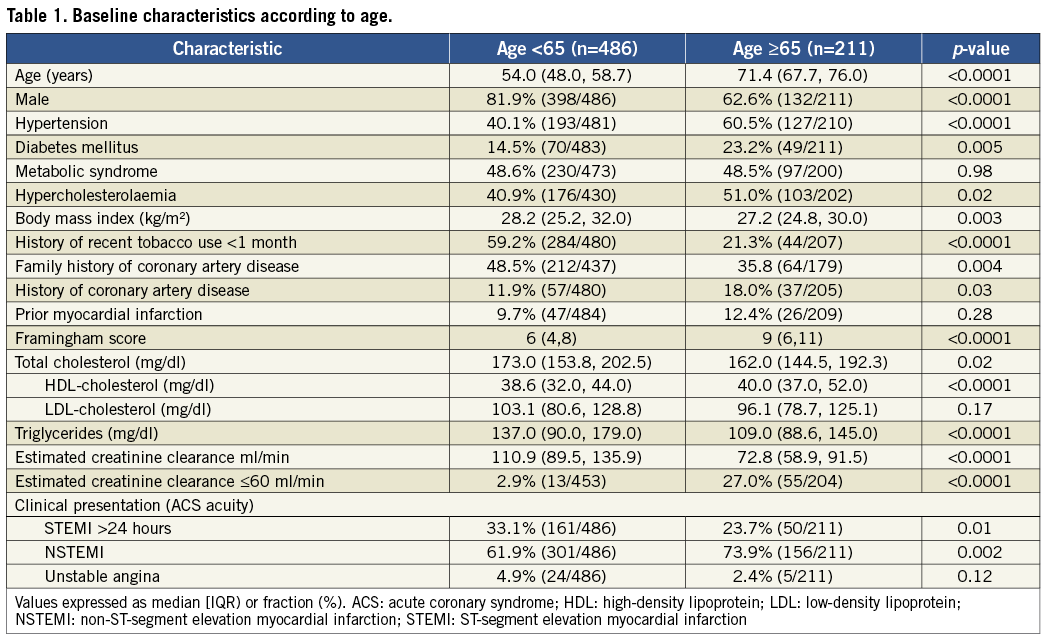
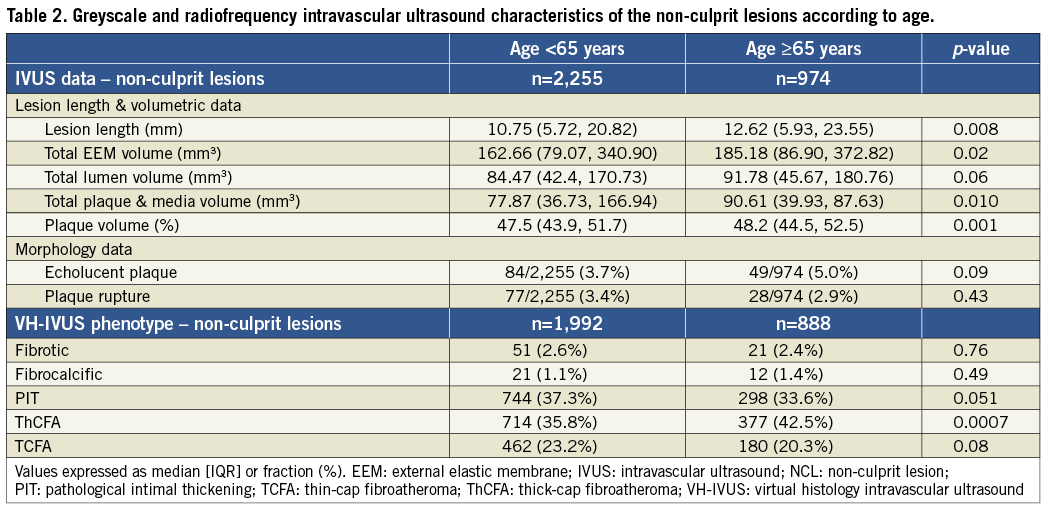
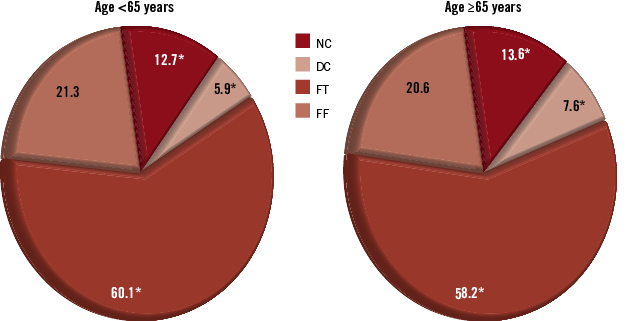
Figure 1. Distribution of the four VH-IVUS plaque components in the non-culprit lesions from both age groups. Proportion provided using mean percentages. DC: dense calcium ; FF: fibro-fatty tissue; FT: fibrous tissue; NC: necrotic core; *p-value <0.05 for the difference
PATIENTS <65 YEARS OLD ACCORDING TO GENDER
Among the 486 patients <65 years of age, women presented with a greater prevalence of cardiovascular risk factors and comorbidities, including more frequent hypertension, metabolic syndrome, cigarette smoking, lower creatinine clearance and a higher Framingham risk score than men (Table 4). Although the total length of coronary tree analysed with VH-IVUS was comparable in the young men and women, the median number of NCLs (5.0[4.0, 6.0] vs. 4.0[3.0, 6.0], p=0.004), fibroatheromas (FA) per patient (3.0[2.0, 4.0] vs. 2.0[1.0, 3.0], p=0.007) and total lesion length (74.13 mm[44.98, 104.99] vs. 56.93 mm[31.12, 82.84], p=0.0007] were greater in young men than women. In the non-culprit segments imaged, no differences were found in the percentage of necrotic core (NC) or dense calcium (DC), but lesions in young women compared to men had a greater percentage of fibrous tissue (FT) (61.7%[57.5, 65.3] vs. 60.0%[56.1, 64.4], p=0.04). NCLs in young men compared to women had greater plaque volume and more frequent plaque ruptures (Table 5). Significant differences were found in the percentage of fibrous and fibro-fatty tissue between both subgroups in NCLs according to gender (Figure 2), and NCLs in women were more likely to be classified as fibrotic plaques (Table 5). The NCL-related MACE rate during follow-up did not differ significantly between young men and women (Table 3).
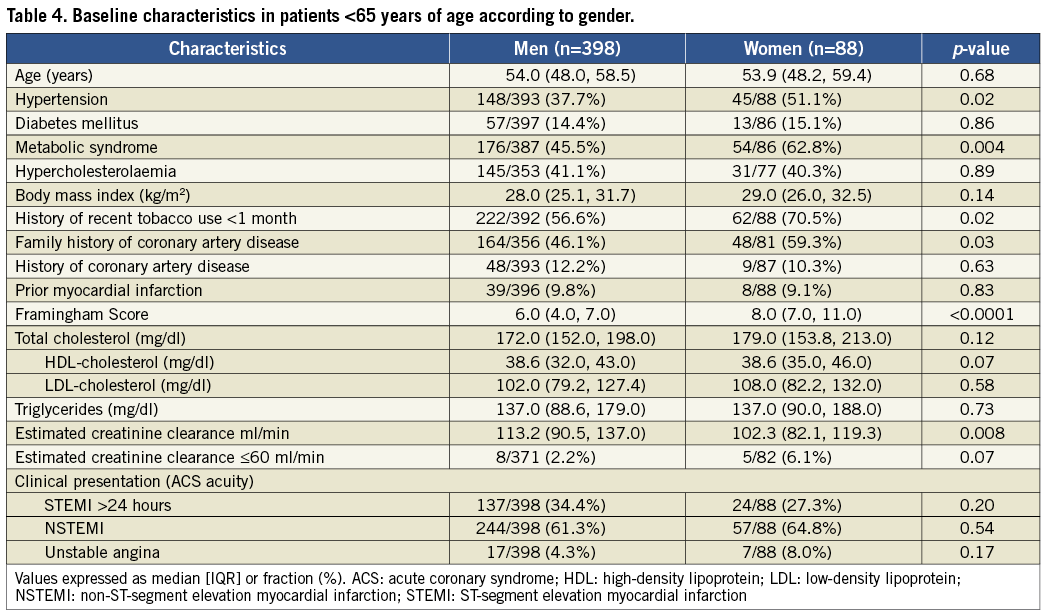
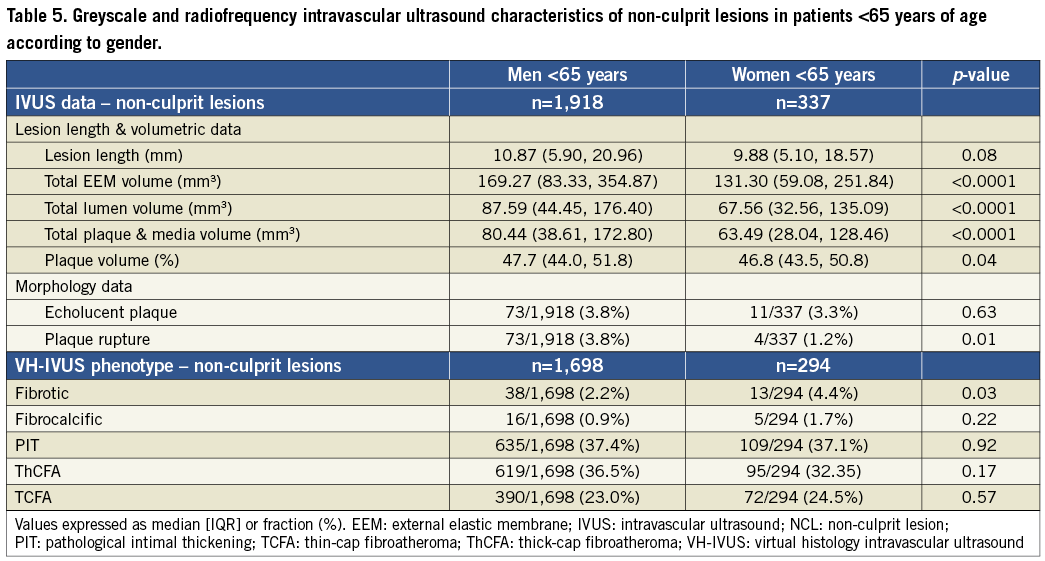
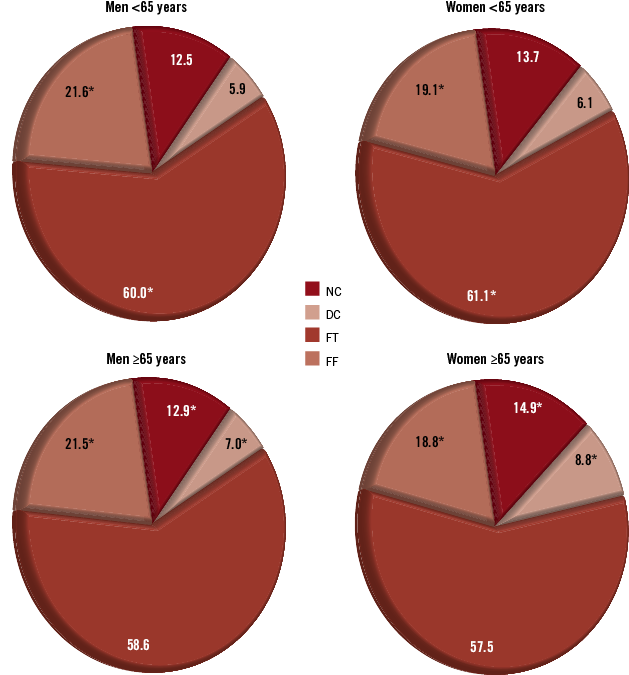
Figure 2. Distribution of the four VH-IVUS plaque components in the non-culprit lesions according to gender. Top: in patients <65 years of age. Bottom: in patients ≥65 years of age. Proportions provided using mean percentages. DC: dense calcium; FF: fibro-fatty tissue; FT: fibrous tissue; NC: necrotic core; *p-value <0.05 for the difference
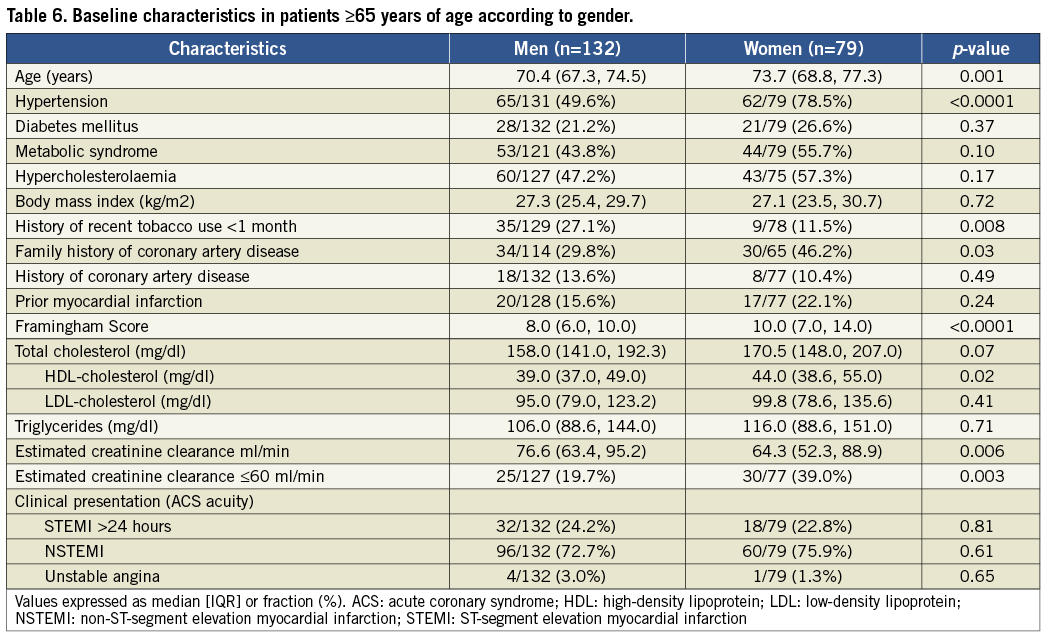
PATIENTS ≥65 YEARS OLD ACCORDING TO GENDER
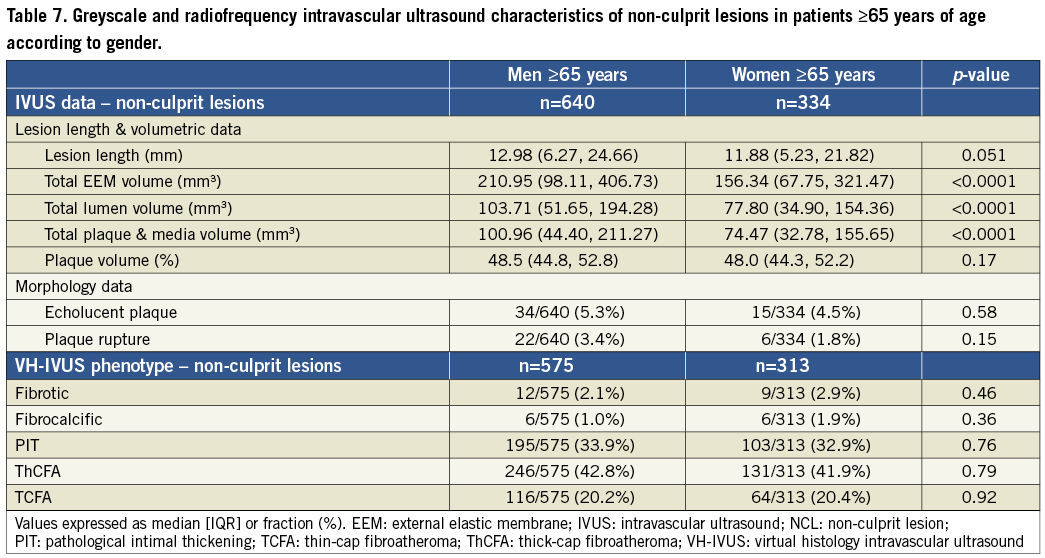
As in young patients, among the 211 patients ≥65 years of age, women compared to men also presented with a higher cardiovascular risk profile, being older, more likely to have hypertension and cigarette smoking, lower creatinine clearance and a higher Framingham risk score (Table 6). In this group, the length of coronary tree imaged with VH-IVUS and the number of NCLs identified per patient were not significantly different. Elderly men compared to women had longer diseased NCL segments (78.16 mm[51.63, 115.59] vs. 70.94 mm[43.98, 91.96] respectively, p=0.02) but a similar percentage of plaque volume. Elderly men compared to women had a lower percentage of NC in the NCL segments (12.3%[8.3, 17.4] vs. 15.2%[9.9, 19.3], p=0.04) but a higher percentage of fibro-fatty tissue (21.4%[14.9, 26.6] vs. 16.7%[12.8, 23.8], p=0.02). The NCLs of elderly women also had a greater percentage of NC and DC volume (Figure 2), although the relative percentages of lesion phenotypes were not significantly different according to gender (Table 7). Finally, as in the younger group of patients, no differences were observed in the follow-up rates of NCL-related MACE between sexes in the elderly age group (Table 3).
Discussion
The current study demonstrates the existence of in vivo age-related differences in NCL plaque morphology and composition, as detected by VH-IVUS. While in the present study of stabilised patients with ACS the overall rates of NCL-related MACE did not vary significantly according to age, distinctive plaque composition and morphology were found in patients <65 years old vs. ≥65 years old, which further varied according to gender in each age group.
The aging process induces changes in the cardiovascular system, which accelerate atherosclerosis1. It has been hypothesised that age may make arterial walls more susceptible to hypercholesterolaemia, promoting plaque growth and a propensity towards intra-plaque haemorrhage21. However, the in vivo effects of age on plaque formation and composition have not been studied. Our analysis has shown several age-related differences in the coronary plaques of patients with ACS, which supports the idea of a modifier effect of age in atherosclerosis development and progression over time.
Consistent with previous findings from human autopsies2 and IVUS22, our study has also demonstrated greater coronary plaque burden with advancing age. Similarly, the larger percentage of dense calcium in NCLs in the group of patients ≥65 years old confirms prior reports with computed tomographic imaging that coronary atherosclerotic calcification increases with age23,24. While the present study did not demonstrate age-related differences in the distribution of high-risk plaques (e.g., ruptured plaques or TCFAs), the larger percentage of necrotic core and lower percentage of fibrous tissue in the NCLs from older patients may in part explain the higher prevalence of symptomatic CAD as age increases.
We also observed gender-specific changes in young vs. older patients which deserve comment. Women have a higher cardiovascular risk profile than men when presenting with an ACS25, and these sex differences are more marked at younger ages15,26. In our study, both younger and older women presented with a larger number of traditional risk factors and a higher Framingham risk score compared to men. A greater burden of coronary atherosclerosis may therefore possibly be expected in women compared to men27. However, not only did we not find any differences in the percentage of plaque volume in the non-culprit segments, but men in the same age group had a greater frequency of FAs and NCLs, with larger plaque volume. Plaque ruptures were also observed more frequently in younger men than women. These findings are concordant with previous observations from pathological and in vivo studies28-31.
Another notable finding in younger women when compared to younger men was the higher percentage of fibrous tissue in their non-culprit segments and NCLs, as well as a greater number of fibrotic plaques. Conversely, a propensity toward excessive fibrous tissue in elderly women compared to elderly men was not noted. Consistent with these findings, sex-based differences in fibrous plaque composition has been previously reported from a cohort of patients with a mean age of death <65 years11. It has been speculated that one of the effects of oestrogen might be stabilisation of the fibrous cap, given that premenopausal women compared to postmenopausal women were shown to have a thicker fibrous cap10. Recently, fibrous tissue as characterised by VH-IVUS has also been related to the plaque stability in in vivo studies, as fibrotic or fibrocalcific plaque rarely evolves into FAs over a 12-month period32.
As previously suggested31-33, many of the vessel and plaque-specific differences between men and women present in patients <65 years old tended to disappear with increasing age. Thus, in our older group of patients, the percentage of NC and DC in NCLs increased in women. It is known that women have a delay in the presentation of obstructive CAD, and that the rates for men and women become almost equal only in the seventh decade of life34. Our findings support the idea of a modifying effect of sex in the pathophysiology of atherosclerosis; endogenous oestrogen might modify the growth of the plaque inducing less stenotic lesions35. However, the present study suggests that the combination of smaller coronary arterial volumes and the particular distribution of lesions and plaque components might increase relatively the risk in younger women.
It has also been established that traditional risk factors do not play the same role in men and women, and that their effects vary according to the age of the patient34. In the general population, these factors have a differential impact on atherosclerotic burden36 and the amount of NC in plaque as assessed with VH-IVUS37. Our study also raises the concern about the possible lack of accuracy of the traditional risk factors and scores to predict the degree of CAD and lipid content in younger women.
Finally, despite both female subgroups having a higher cardiovascular risk profile than men of a comparable age, the cardiac prognosis in the present study was similar in men and women in each age group. Traditionally, the general assumption has been that younger women presented with greater mortality and complication rates after ACS than men12-15, although recently this belief has been questioned17. While the absence of age and gender-related follow-up MACE differences in the present study might be due to its modest size, coupled with excellent adherence to secondary preventative measures and close clinical follow-up, this report is also consistent with the findings of recent studies demonstrating improvements in the prognosis of women with ACS26,38 and after PCI39-40.
There are other limitations to the present study. Although data were collected prospectively, and events were adjudicated blinded to the VH-IVUS results, the present findings represent the results from a post hoc analysis and thus should be considered hypothesis-generating. Our results also only apply to the patient population enrolled, i.e., those with a recent ACS treated with successful PCI. Whether these results would apply to asymptomatic patients and to those with stable coronary syndromes deserves further study. Finally, the axial resolution of VH-IVUS is ~150 um, and thus we were unable to assess whether differences in fibrous cap thickness as a function of age exist.
In summary, our findings suggest that age and sex have a modifying effect on the extent and composition of CAD. Furthermore, traditional risk factors overestimate the burden of atherosclerosis in younger women. Further research is required to ascertain the mechanisms of these age and sex-based differences in atherosclerosis progression, and to improve our models to predict which patients will develop symptomatic CAD.
Funding sources
The study was funded by Abbott Vascular and Volcano.
Conflict of interest statement
The authors have no conflicts of interest to declare.

