This editorial relates to the article in this issue of EuroIntervention by Raphael Romano Bruno et al “Virtual reality-assisted conscious sedation during transcatheter aortic valve implantation: a randomised pilot study”1.
Whilst virtual reality (VR) is a technology that is relatively established in modern gaming, medical researchers and physicians are now realising its potential as a distraction therapeutic which may provide a reduction in emotion-based symptoms including anxiety and pain. Currently, VR is applied in contexts such as pain relief2, neurocognitive disorders such as stroke3, and psychiatric disorders4. From a patient perspective within interventional cardiology, VR is now fermenting interest in relation to anxiety and pain.
To achieve VR, a dedicated headset is required. Users are provided with a computer-generated three-dimensional surrounding. The headset comprises a stereoscopic head-mounted display where sensory information is delivered to the user. Head movements are tracked so that images and motion adapt in a natural manner, creating an impression of immersion. Hand controls provide interaction with the virtual surroundings. Archaic innovations with VR resemblance have existed previously. For instance, the first steps in stereographic photography were taken in 1939 with the View Master, a device with thin cardboard discs containing stereoscopic 3D pairs of small transparent colour photographs. This device was very popular with holidaymakers and was still used until the 1970s in medical education to portray complex anatomies. However, it was Morton Heilig who in an essay in 1955 describing “the cinema of the future” inspired the development of the Sensorama machine, an immersive primitive multimodal VR system which interestingly included separate odour and wind sensory tracks. The term “virtual reality” itself is credited to Jaron Lanier who, in 1989, developed a full body suit of sensors for body movement recordings, a technique which is extensively used in film and game productions5. In 1991, Sega, who produced the premium game console at the time, developed the ill-fated Sega VR headset which, due in part to the Oni-Sendai tracking element in the headset (which included a liquid gas-filled sphere causing nausea and headache), failed to enter the market.
In the mid 1990s, VR was more widely introduced in medicine for training and education and was, in particular, of interest for cardiology when 3D echocardiography became available6. It helped to create databases of different pathologies that could be used for the further development of VR models of the heart. Interestingly, within other medical specialties such as psychology, dentistry and neurology, VR technology has been used since its availability for anxiety reduction and rehabilitation. The use of VR to reduce or even replace the use of anaesthetics was first described in a case report by Wright et al in 20057.
More recently, we have seen an acceleration in developments in computer-based visualisations, and many new applications are becoming available within cardiology8. Within structural heart-based interventional cardiology, the use of computer simulations has so far mainly focused on creating patient-specific models that are used to determine the further treatment plan. An example of this is selecting the optimal aortic valve prostheses for TAVI procedures9.
In relation to anxiety and cardiovascular disease, a number of reports have focused on anxiety in the pre-procedure phase or as a predisposing factor in the progression of cardiovascular disease10 and others on rehabilitation post procedure. Of interest, one group investigated the levels of anxiety in 3,600 patients undergoing an angiogram or percutaneous coronary intervention at different times of their admission and found that anxiety is highest immediately around the procedure, particularly in patients aged <65 years11.
The use of VR to reduce anxiety and, thereby, the reduction of the use of sedatives during TAVI has not been described before, for which the authors are to be congratulated. It is a novel and potentially “mind-changing concept” for both the patient and the medical team. Anxiety induces a rise in cortisol levels, which can lead, among other things, to delirium. Delirium frequently occurs after TAVI; therefore, measures that reduce or eliminate contributing factors are welcome12. As shown in other medical specialties, this can possibly be achieved by using VR technology13. In a pilot randomised study, the authors compared the effects of VR on the occurrence of anxiety (visual analogue scale [VAS]) before and after TAVI between 16 who underwent TAVI with VR and 16 patients without VR support. During the procedure, the VR patients watched relaxing 3D videos the content of which was chosen beforehand by the patients themselves. Acknowledging the small scale and pilot nature of the study, the findings indicate that the use of VR during TAVI is feasible and reduces anxiety. The hypothesis that VR may reduce or even supplant the use of sedatives is interesting but needs further exploration.
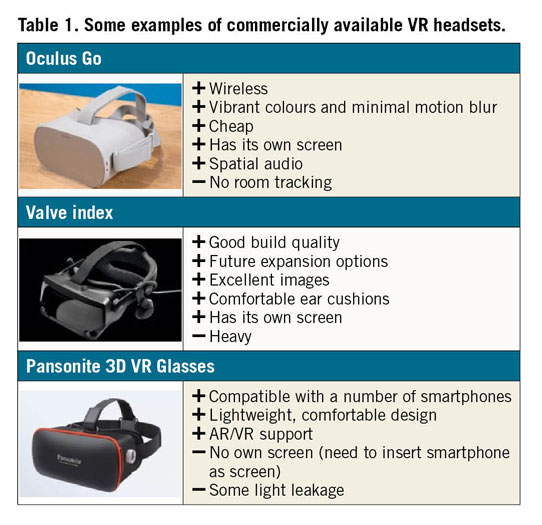
It is interesting to see that these elderly patients accepted the use of VR technology during a stressful intervention. To have a better understanding of the acceptance and feasibility of VR during TAVI, the number of patients in the index population from whom the 40 initially eligible patients were selected needs to be known. Selection most likely biases the findings of acceptance and tolerance of VR during TAVI. Notwithstanding the fact that the use of VR is currently less complicated and more “customer-friendly”, a headset still needs to be worn (Table 1). This may be cumbersome and, more importantly, it creates a loss of visual contact of the patient with his/her surroundings that in itself may induce psychological discomfort. The acceptance of VR by the medical team was different. In this small-scale experiment, VR was perceived both as an intrusion and as an opportunity. The authors report no occurrence of “cyber sickness”. It should be acknowledged that the patients in this study were exposed to 2D films and not a true VR that has been reported to cause cyber sickness.
Anxiety was measured using the VAS the instrument of which is a questionnaire that captures the subjective characteristics of phenomena that cannot be directly measured. It is true that pain and fear or anxiety are difficult not only to define but also to measure directly. An objective and quantitative surrogate for this may be the measurement of the changes in blood pressure, heart and respiratory rates and why not the amount and qualitative analysis of transpiration and cortisol levels.
It has been said that a “house that does not change is a dead house” (Phantom Thread, 2017) but the question is whether regular care that consists of a careful preoperative planning including – among others – risk assessment of fear, anxiety and postoperative delirium followed by a skilled and serene execution of TAVI under local anaesthesia by a dedicated and disciplined team has the same or even a more pronounced effect on perioperative psychological discomfort, obviating the need for technological support such as VR12. This does not exclude the role of VR during TAVI in patients refractory to this fundamental principle of care or in more complex interventions such as brain surgery.
This innovative project touches on the important topic of patient wellbeing supported by modern computer techniques to reduce or prevent anxiety during cardiac intervention and TAVI in particular. While more studies are needed to prove its true effectiveness, we are confident that we will see many more such initiatives. Benjamin Franklin already knew in the 18th century that “An ounce of prevention is worth a pound of cure”.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.