Abstract
Aims: Virtual reality (VR) has been used successfully in different clinical settings to treat anxiety. This prospective, randomised pilot study aimed to investigate the feasibility and safety of VR in patients undergoing conscious sedation during transfemoral transcatheter aortic valve implantation (TAVI).
Methods and results: Thirty-two patients were included and randomised to VR intervention (n=16) or control (n=16). In the intervention group, patient-selected relaxing 3D videos were projected during the TAVI procedure; pain and anxiety before and after TAVI were measured using visual analogue scales (VAS; 0-10). The median age was 83 years (IQR 78.25-87). Patients’ baseline characteristics did not differ significantly between the groups. During TAVI under conscious sedation, the median duration of VR intervention was 30.5 minutes (IQR 23.5-46); 81.3% of the patients watched the videos until device implantation, 37.5% during the whole procedure. The VR intervention group reported significantly less anxiety after the procedure (VAS 2 [IQR 0-3.75] vs 5 [IQR 2-8], p=0.04) than patients randomised to control. In the intervention group, 93.8% would use VR during TAVI again. Nausea and vomiting did not occur more frequently compared to control.
Conclusions: VR interventions during TAVI to assist conscious sedation are safe and feasible, even in very old and frail patients. In this small cohort, there was a significant reduction in periprocedural anxiety.
Introduction
Transcatheter aortic valve implantation (TAVI) is an established therapy for patients with severe, symptomatic native aortic valve stenosis at high operative risk1. More and more trials show equal or superior results compared to surgical aortic valve replacement even in intermediate- and low-risk patients2,3,4. Periprocedural pain and anxiety remain an unsolved issue5. The use of benzodiazepine and opioid administration should be minimised in the elderly populations6,7,8. Therefore, innovative non-pharmacological strategies to treat pain and anxiety are needed. Such a strategy could be the use of virtual reality (VR). VR has been used successfully in several clinical settings in order to reduce anxiety9,10,11. The main problem that limits the use of VR is “cybersickness”, defined as nausea, disorientation, blurred vision, and headaches – a malady during VR experience12. In addition, TAVI patients, due to their advanced age and fragility, might be very hostile to the use of such novel technologies. We thus hypothesised that VR interventions during TAVI procedures could be beneficial for periprocedural and post-procedural patient wellbeing. The aim of this prospective randomised clinical trial was to prove the feasibility, safety, and acceptance of VR interventions in patients undergoing conscious sedation for TAVI.
Methods
STUDY DESIGN
This study was designed as a single-centre, prospective, open-label, randomised controlled trial. It was approved by the Ethics Committee of the Medical Faculty of the University Hospital Düsseldorf, Germany (date of approval: 8 August 2019; 2019-425). The study flow chart is shown in Figure 1.
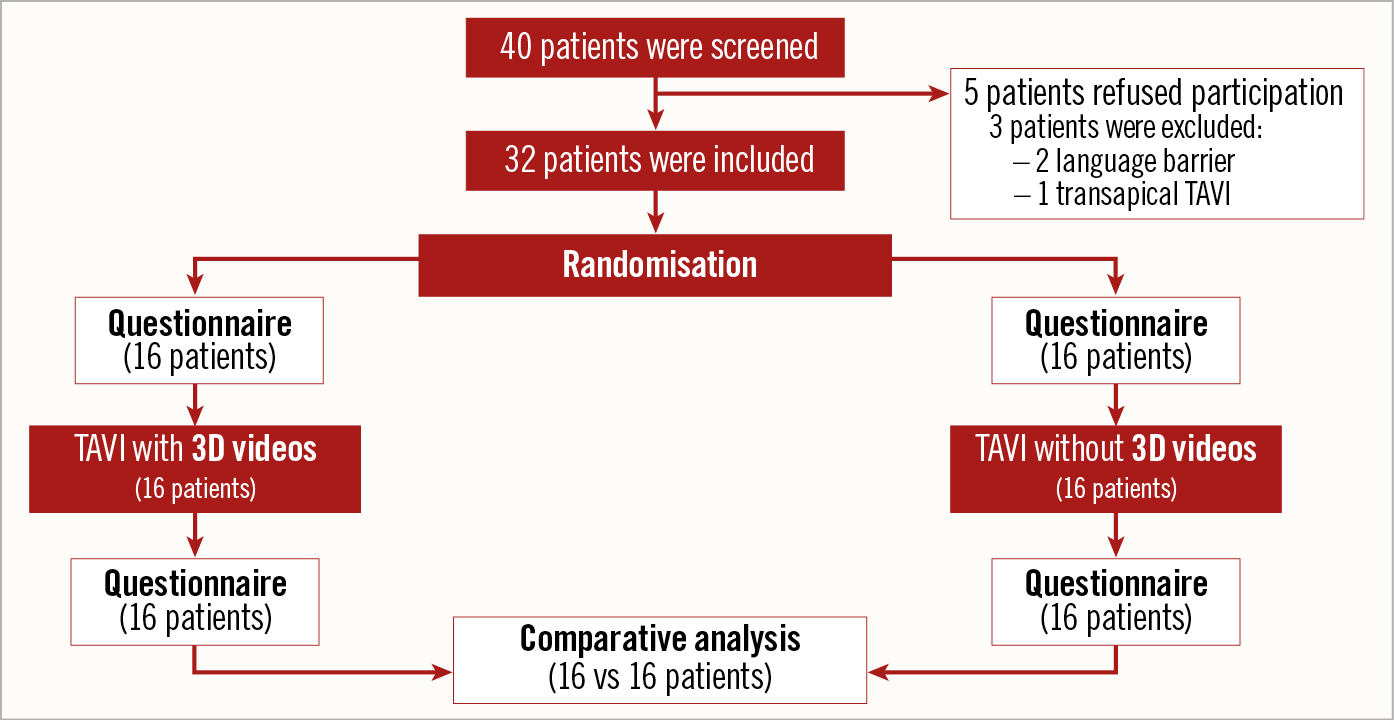
Figure 1. Study flow chart showing the screening, the inclusion and the randomisation of the patients.
RECRUITMENT AND RANDOMISATION
Patients undergoing transfemoral TAVI for severe aortic valve stenosis at Düsseldorf Heart Center from December 2019 to January 2020 were screened for eligibility and included after informed consent. Patients limited in communication (e.g., language barrier), suffering from cognitive impairment (e.g., dementia) or uncorrectable eyesight were excluded, as well as all patients undergoing general anaesthesia during transapical TAVI. Patients were then randomly assigned either to the intervention group (3D glasses with videos during TAVI) or to the control group (no 3D glasses).
DATA MANAGEMENT
All data were recorded for subsequent analysis. Medical history, clinical and laboratory parameters were available from the in-hospital patient data management system (Medico®; Cerner Deutschland GmbH, Idstein, Germany) and/or direct patient contact. Frailty was assessed with the Clinical Frailty Scale (CFS). All data were anonymised and handled according to the local data protection requirements.
PERIPROCEDURAL PATIENT MANAGEMENT
For anxiety management, all patients were offered an oral dose of 1 mg lorazepam or 3.25 mg midazolam prior to the intervention. No additional sedative intravenous drugs (e.g., propofol, midazolam) were used periprocedurally. No general anaesthesia was used in any patient. For analgesic management, all patients received regular local analgesia of the vascular access at the groin with xylocaine. Signs of pain were monitored closely. If needed, local analgesia was supplemented with low-dose intravenous remi-fentanil in non-sedative doses (maximum 0.06+0.05 µg/kg/minute). Thus, all patients were awake, responsive and oriented during the procedure (“conscious sedation”). The continuous invasively measured blood pressure values were recorded. To assess blood pressure fluctuations, blood pressure differences were calculated between every two consecutive time points to assess the relative deviation (shown as [%]). Thus, the maximum relative increase and decrease were calculated for every patient.
VIRTUAL REALITY
For the VR intervention, MEDION® ERAZER® X1000 MR Glasses, 7.34 cm (2.89’’) LC-Display (Medion AG, Essen, Germany) were used and demonstrated to patients the day before the TAVI procedure. To use this technology, a modern notebook was needed. The VR glasses cost approximately 250 €. The videos were open-source and were freely available on the internet. All these items represented a one-time investment. Videos were presented using “Windows mixed reality for Steam® VR” (Windows [Microsoft Studios, Microsoft Corporation, Redmond, WA, USA], and Steam [Valve Corporation, Bellevue, WA, USA]) and “Bigscreen Beta” (Bigscreen Inc., Berkeley, CA, USA). Patients could choose one of the following videos: nature scenery, an aquarium, flying over a green landscape, diving underwater or walking through a calm forest. Intervention duration was recorded, as well as whether the glasses were worn until implantation or until the end of the procedure. Patients using the three-dimensional (3D) glasses were able to turn or lift their head easily but were not able to move independently through 3D virtual space (Figure 2). Controllers for manual commands by patients were not used for safety reasons.
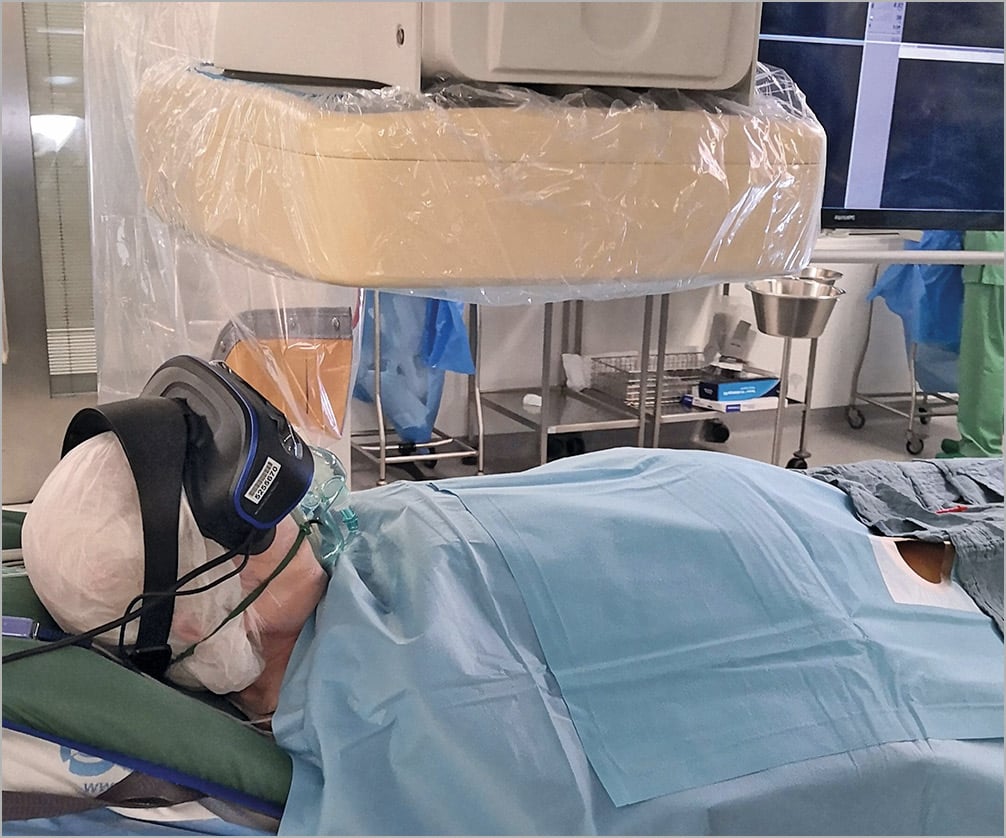
Figure 2. Example image for the use of VR glasses in the operating room.
PATIENT QUESTIONNAIRES
All patients underwent a preprocedural educational talk, where they were asked for previous experiences with VR glasses and their use of a mobile phone, smartphone or personal computer at home. They were also questioned about their expectations on how 3D-VR interventions would help to calm them down during the procedure (yes/no/maybe) (Supplementary Figure 1, Supplementary Figure 2). All patients completed a questionnaire assessing anxiety, once the day before and again one day after the TAVI procedure, which was measured by a simple visual analogue scale (VAS, 0=no anxiety, 10=worst imaginable anxiety). In addition, all patients were questioned after the procedure as to how much pain they had experienced during the intervention (0=no pain, 10=worst imaginable pain).
SAFETY ISSUES
No acoustic stimulation was used in order to allow verbal communication between the team and the patient. Hence, the patient could be regularly informed about the status of the procedure and questioned about his/her condition. Patients were allowed to quit the VR intervention at any time point. Throughout the procedure, they were repeatedly asked about nausea (yes or no) or other side effects of VR. All adverse events during the intervention, including “vomiting”, were protocolled. Patients were asked not to move their arms during the procedure for safety reasons.
STATISTICAL ANALYSIS
Continuous data are expressed as mean ± standard deviation (SD) or median ± interquartile range depending on the distribution. Differences between independent groups were calculated using the Student’s t-test or Mann Whitney U test as appropriate. Categorical data are expressed as counts and percentages. Chi-square tests were applied to calculate differences between groups and the Wilcoxon rank test for paired data. All tests were two-sided, and a p-value of <0.05 was considered statistically significant. SPSS, Version 23.0 (IBM Corp., Armonk, NY, USA), was used for all statistical analyses.
Results
PATIENT CHARACTERISTICS
Forty patients were screened. Five patients refused participation and three patients had to be excluded (two patients due to language barrier, one due to transapical procedure) (Figure 1). The majority of patients were male (62.5%) with a median age of 83 years (IQR 78.25-87). The median CFS was 4.5 (IQR 3-6), which corresponds to a vulnerable to a mildly frail patient population. The baseline echocardiographic parameters did not differ between the groups regarding ejection fraction, valvular diseases, pulmonary hypertension and the values for the end-diastolic septal diameter, end-diastolic left ventricular diameter and the end-systolic left atrial volume (Supplementary Table 1). There were no statistical differences between the interventional and the control group in the patients’ characteristics and comorbidities (Table 1).
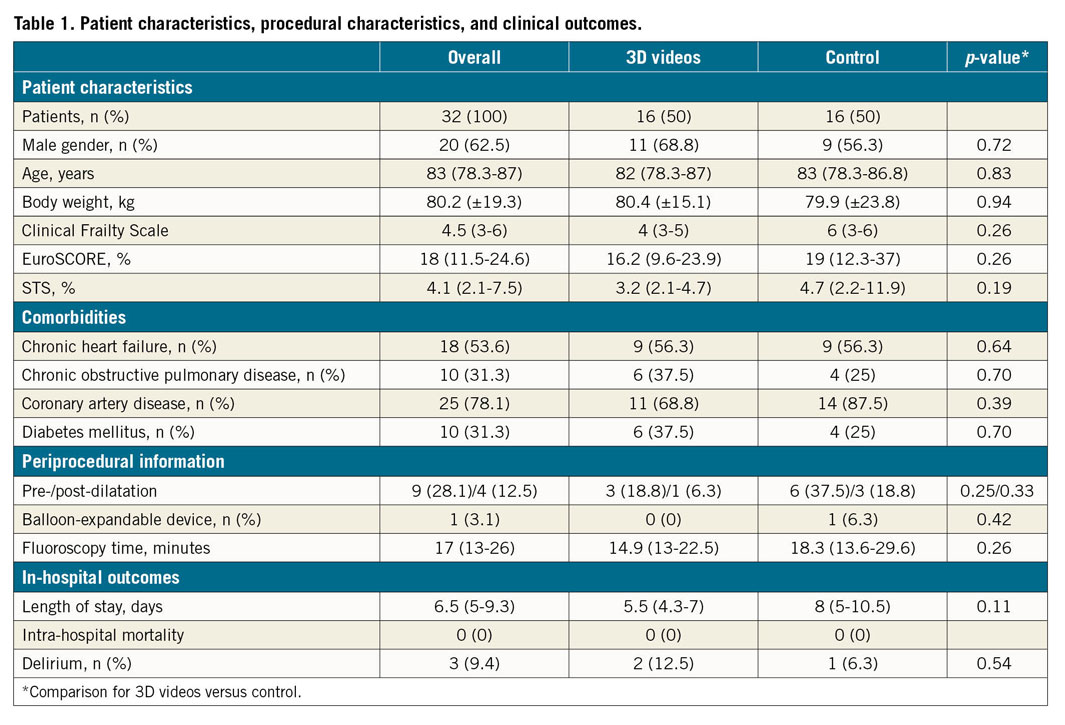
PROCEDURAL CHARACTERISTICS AND IN-HOSPITAL OUTCOMES
In all patients, femoral vascular access was used. The contralateral femoral artery was used for secondary vascular access; no radial access was used. One patient in the control group received a balloon-expandable valve; all other patients were treated with self-expanding devices (p=0.48). Rates of predilatation (6 patients in the control group vs 3 patients in the interventional group, p=0.23) and post-dilatation (3 patients vs 1 patient, p=0.33) were equivalent in both groups. Fluoroscopy time was equal in both groups (14.9 [13-22.5] minutes vs 18.3 [13.6-29.6] minutes; p=0.26). There was no difference in vascular complications (3 minor bleedings according to VARC in the control group and 2 in the interventional group; p=0.65). The median length of stay was 6.5 days (IQR 5-9.25); there was no significant difference between the groups (5.5 days [IQR 4.25-7] in the interventional group vs 8 days [IQR 5-10.5] in the control group, p=0.11). Delirium was reported for one patient in the control group and two patients in the interventional group (p=0.54). No patient died during the hospital stay.
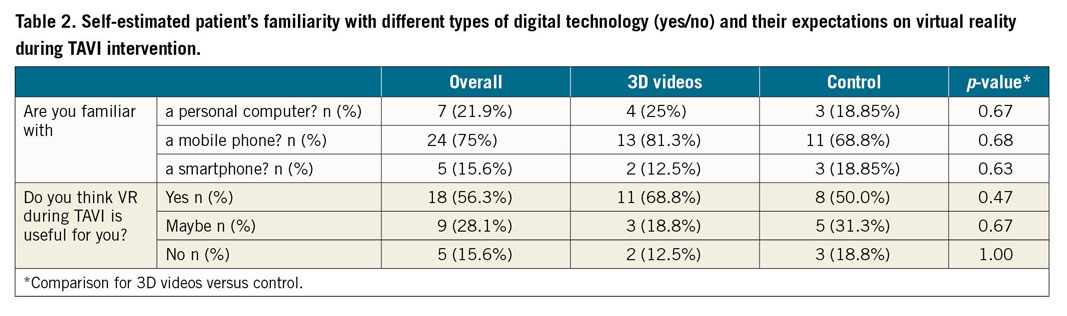
AFFINITY FOR TECHNOLOGY
None of the patients had used 3D glasses before. The majority were able to handle a mobile phone (75%), but only a few were familiar with a personal computer (21.9%) or a smartphone (15.6%). After bedside demonstration the day before the procedure, most patients believed that the peri-interventional use of 3D glasses might be definitely (56.3%) or possibly (28.1%) helpful in order to relax (Table 2).
PRE- AND PERI-INTERVENTIONAL DRUG TREATMENT
In both groups, six patients (19% per group) received pre-interventional benzodiazepine. There was no difference between the groups regarding the peri-interventional use of remifentanil (6 patients in the interventional group vs 10 patients in the control group; p=0.08). In those patients who received remifentanil, no statistically significant differences were seen in the maximum application rates (0.04±0.02 µg/kg/minute in the interventional group vs 0.06±0.05 μg/kg/minute in the control group; p=0.36).
VIRTUAL REALITY INTERVENTION
The 3D glasses were tolerated well: the median application time was 30.5 minutes (IQR 23.5-46); 81.3% of patients wore 3D glasses until the implantation was completed, 37.5% until the end of the procedure. The most common reasons cited for ending VR were annoyance and heat generation. The latter was not caused by the VR glasses, but by the thermal blanket. The day after the procedure, 93.8% of patients stated that they would like to use 3D glasses during a medical intervention again. The most popular 3D video contained forests, lakes, coasts, castle ruins and landscapes in drone flight.
PERIPROCEDURAL ANXIETY AND PAIN
Results on periprocedural anxiety are reported in Figure 3. On average, all patients reported moderate anxiety the day before the TAVI procedure (VAS 3.5, IQR 0-5.75 vs VAS 3, IQR 2-6; p=0.42). Patients in the interventional group reported significantly less anxiety during the procedure (VAS 2 [IQR 0-3.75] vs 5 [IQR 2-8]; p=0.04). The subjective pain levels during the intervention did not differ between the groups (VAS 4 [IQR 3-4.8] in the interventional group vs 4 [IQR 2-6] in the control group; p=0.61).
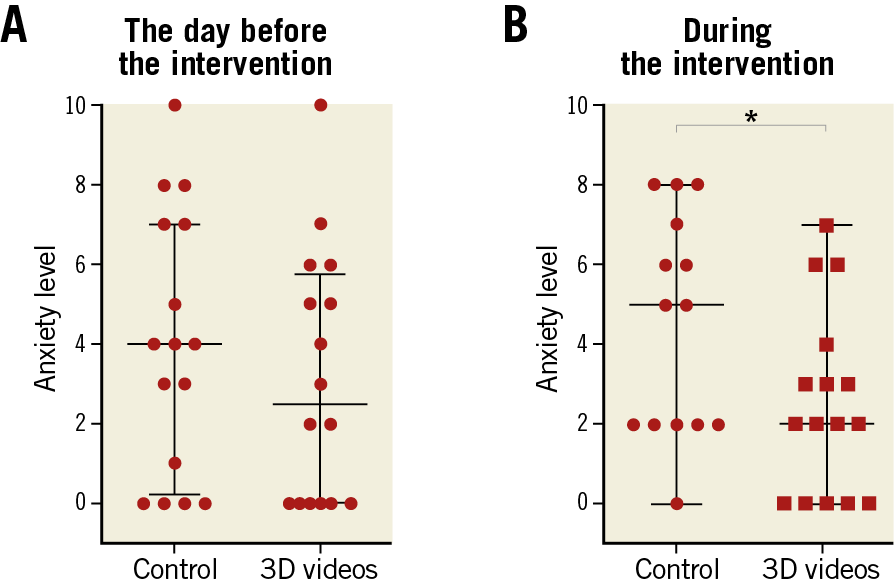
Figure 3. Subjective levels of anxiety before and during the intervention. A) Subjective level of anxiety on the day before the intervention. B) Subjective level of anxiety during the intervention. * p<0.05 for 3D videos versus control. VAS: visual analogue scale (0=no anxiety; 10=maximum anxiety)
PERIPROCEDURAL HAEMODYNAMICS
The maximum relative increase in blood pressure was similar in both groups (145% [IQR 132.2-158.8] for the control and 136.4% [IQR 122.7-163.6] for the interventional group; p=0.54). The same applies to the maximum relative decrease in blood pressure (64.5% [IQR 59.4-78.1] for the control group and 61.8% [IQR 57.1-74.4] for the interventional group; p=0.4). Neither the maximum relative increase nor the maximum relative decrease in blood pressure deviation showed a significant impact on nausea (p=0.6 for the maximum increase in blood pressure, and p=0.74 for the maximum decrease) or vomiting (p=0.87 and p=0.93, respectively).
VR ACCEPTANCE OF THE INTERVENTIONISTS
Not only was the acceptance of this new technology by the patients important, but also the approval by the interventionists. Initially, the reaction of the interventionists ranged between full support and slight refusal. Those who hesitated to apply this new approach thought that their periprocedural interaction with the patient might be limited. However, during the course of the study, acceptance increased since interaction was not limited.
SAFETY
The rates of nausea and vomiting events recorded were 12.5% and 6.3%, respectively, without any difference between the groups. No technical complications regarding the device were observed.
Discussion
This proof-of-concept study demonstrates the safety and feasibility of VR-assisted conscious sedation during TAVI. The main findings are: 1) this novel technological approach is safe for use in TAVI; 2) there was a significant reduction of periprocedural anxiety by using VR; 3) the subjective responses of participants were very positive for using VR again for similar procedures; 4) even frail older patients accepted this innovative approach.
These results are very important as the proportion of older patients is constantly growing13. Accordingly, the incidence of severe aortic stenosis increases and presents a significant burden to the healthcare system14. TAVI is an established therapy for patients with severe, symptomatic native aortic valve stenosis at high operative risk1. The procedure is both safe and feasible even in nonagenarians15. However, periprocedural anxiety remains a constant concern5. VR has already been used successfully in various clinical settings: it attenuated anxiety and reduced pain in brain mapping with direct electrical stimulation during awake craniotomy9 or intravenous injections16. VR was feasible for children undergoing intravenous puncture10, during immunisation11 or dental intervention16. However, a trial that was performed during cystoscopy demonstrated no benefit regarding anxiety and pain for the patients17. Until now, VR has never been used for this purpose during TAVI.
For the current study, we expected a high degree of reluctance to wear 3D glasses, as the patients had little or no previous experience with newer electronic devices such as smartphones or computers. Not a single patient had ever put on VR glasses before this investigation, but surprisingly all approached patients were very open to this technology. Almost all patients in the intervention group stated that they would like to use such 3D glasses again for comparable operations.
A very common complication when using 3D glasses is “cybersickness”, which is characterised mainly by nausea and vomiting12. Since our patients were strictly in a supine position during TAVI but the 3D videos were played straight ahead, we expected an increased incidence of nausea and vomiting a priori in this experimental set-up. However, this did not occur more frequently than in the control group. The observed cases were closely related in time to transient hypotension during rapid pacing, so that the causal relationship to the 3D glasses is unclear.
In summary, VR during TAVI might result in a significant reduction of stress and periprocedural anxiety. This is of great importance because these factors contribute to the development of postoperative delirium (POD). POD affects 23% of patients after TAVI18 and negatively influences the length of stay19, the risk for hospital readmission and mortality20,21. Further studies should explore whether VR results in a significant reduction of periprocedural pain and anxiety and whether these reductions lead to a lower incidence of POD.
Limitations
Neither pain nor anxiety could be assessed objectively. A correlation with the vital parameters is hardly objectively possible due to procedural fluctuations in blood pressure, heart, and respiratory rate. The present study uses the term “VR” because the 3D glasses are all VR-capable, but in this interventional setting no 3D movement of the extremities could be allowed for safety reasons.
Conclusions
This proof-of-concept study demonstrates the feasibility and safety of virtual reality-assisted conscious sedation during transfemoral TAVI. This novel technological approach was very well accepted by patients and may reduce periprocedural anxiety.
|
Impact on daily practice 3D-VR is feasible and safe during TAVI. This new technology is well accepted even in frail old patients and contributes to an attenuated level of anxiety during the procedure. |
Acknowledgements
Special thanks to Tatiana Kartashova (Institute for Experimental Psychology, Heinrich Heine University Düsseldorf, Germany) and Jenni Scharlau for technical assistance.
Funding
This work was supported by the German Research Foundation (Collaborative Research Centre 259 “Aortic Diseases”) and an academic research grant from the “Forschungskommission” of the Medical Faculty of the Heinrich-Heine-University Düsseldorf [No. 2018-32].
Conflict of interest statement
V. Veulemans reports receiving grants, personal fees, non-financial support and other from Edwards Lifesciences and Medtronic, outside the submitted work. A. Polzin has received travel fees from Medtronic and Edwards. C. Jung reports grants and personal fees from Bayer Healthcare, and Vifor Pharma, personal fees from Bristol Myers Squibb, Boston Scientific, Boehringer Ingelheim, Novartis, and Orion Pharma, and grants from Medicure Pharma, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.