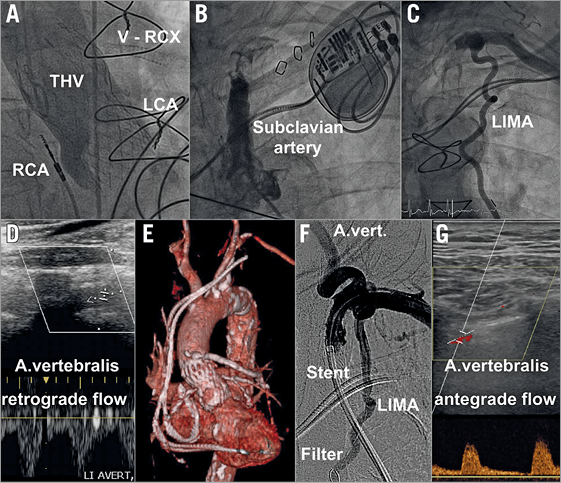
A 78-year-old patient with a history of coronary artery bypass grafting, percutaneous coronary intervention and transcatheter aortic valve implantation (Panel A, THV) was admitted with crescendo angina, dizziness, left arm fatigue and elevated troponin. An angiogram (Panel A) showed chronically occluded right (RCA) and left (LCA) coronary arteries and a chronic in-stent occlusion of the vein graft (V-RCX) to the marginal branch. The left internal mammary graft (LIMA) to the left anterior descending artery could not be intubated because of a new, subtotal stenosis in the left subclavian artery (Panel B). Via a retrograde left brachial approach, the LIMA was found patent with a take-off directly beyond the subclavian occlusion (Panel C). Duplex ultrasound revealed flow reversal in the left vertebral artery (Panel D). Three-dimensional computed tomography reconstructions (Panel E) showed an adequate distance between the subclavian obstruction and the left vertebral artery as well as the LIMA. As a guidewire did not pass the subclavian obstruction antegradely, the stenosis was wired retrogradely from a left brachial approach (Moving image 1) and the wire was snared via the left groin. With a filter wire securing the LIMA (Panel F), the subclavian stenosis was dilated from an antegrade approach and a self-expanding stent was implanted, sparing the take-off of the left vertebral artery and the LIMA (Panel F, Moving image 1). Post-procedural duplex ultrasound documented new antegrade flow in the left vertebral artery (Panel G). Symptoms of coronary and cerebrovascular malperfusion resolved and the patient was discharged home two days later.
The coincidence of cerebral and coronary symptoms in a patient after coronary artery bypass grafting should raise the suspicion of a subclavian steal syndrome, which can be successfully managed by percutaneous revascularisation of the subclavian artery.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. The aortic root angiogram shows a correct position of the transcatheter heart valve, but both native coronary arteries occluded. The saphenous graft to the circumflex artery is occluded as well. There is a functional occlusion of the left subclavian artery but good flow in the left internal mammary artery (LIMA). After retrograde wire passage through the subclavian occlusion, the lesion is dilated and a self-expanding stent is deployed. The LIMA was secured by a filter wire during the procedure.
Supplementary data
To read the full content of this article, please download the PDF.
The aortic root angiogram shows a correct position of the transcatheter heart valve, but both native coronary arteries occluded. The saphenous graft to the circumflex artery is occluded as well. There is a functional occlusion of the left subclavian artery but good flow in the left internal mammary artery (LIMA). After retrograde wire passage through the subclavian occlusion, the lesion is dilated and a self-expanding stent is deployed. The LIMA was secured by a filter wire during the procedure.