Abstract
Aims: To define frequency and predictors of aborted myocardial infarctions (MI) after primary angioplasty.
Methods and results: We analysed 196 consecutive patients with the clinical diagnosis of ST-elevation acute coronary syndrome (ST-ACS) admitted for primary angioplasty to one interventional facility between October 2005 and September 2006. Aborted MI was defined as a creatine increase of less than two times the upper limit of normal, combined with typical evolutionary electrocardiographic changes. Masquerading MI was diagnosed if evolutionary changes were missing or could be attributed to other causes. Thirty-four patients (17,3%) had an aborted and nine (4,6%) a masquerading MI. The main predictor of abortion was Thrombolysis In Myocardial Infarction (TIMI) flow 2 or 3 prior to procedure. The in-hospital mortality of aborted MI was 0%, the one year mortality 2.9%. Sixteen patients without prior or inter-current myocardial infarction had a preserved ejection fraction on cardiac MR at 12 months; in six patients even without any detection of late enhancement.
Conclusions: There is a substantial proportion of aborted myocardial infarction after primary angioplasty, corresponding to a small or even non detectable scar formation in terms of late enhancement on cardiac MR. Preprocedural TIMI flow 2 or 3 is the main predictor of aborted MI.
Introduction
The outcome of patients with ST-segment elevation acute coronary syndrome (ST-ACS) depends on the time between symptom onset and successful reperfusion1,2. Prompt spontaneous or induced reperfusion is able to avoid myocardial necrosis to a large extent, a phenomenon described as an aborted infarction. The original definition of no or only small creatine kinase increase combined with typical evolutionary electrocardiographic changes was first applied to pre- and intra-hospital thrombolysis populations3,4. The observed incidences were between 13.3% and 18.2% with the highest frequency (25%) occurring in patients treated within one hour after symptom onset, reaching a plateau of approximately 10% between two and five hours of symptom duration3,4.
There is little data on the incidence and predictors of aborted myocardial infarction (MI) after primary percutaneous coronary interventions (PPCI)5. We hypothesised that a significant number of aborted MI should also be found after PPCI and, that PPCI would avoid a certain percentage of unjustified fibrinolytic therapy (masquerading MI). Based on this, in consecutive patients admitted for acute angiography with the clinical diagnosis of acute ST-ACS, our primary objective was to determine the proportion and predictors of aborted and masquerading MIs, respectively. Our secondary objective was to determine how the existing CK-based enzymatic definition of aborted MIs translates into late enhancement during cardiac MR in the post-infarction period.
Methods
Study population
Between October 2005 and September 2006 all 196 consecutive patients with the clinical diagnosis of ST-ACS (according to standard criteria) and symptom duration of less than 12 hours who were scheduled for mechanical reperfusion (PPCI) at the Schwarzwald-Baar-Klinikum (SBK) were included into this prospective registry.
The SBK is a tertiary referral centre for a population of about 350,000. There is an established regional referral network for ST-ACS patients involving the ambulance services and five non cath lab hospitals apart from the SBK. Of all patients admitted to any of the network hospitals 87% received a primary PCI and 1% a rescue PCI at the SBK, 3% received only fibrinolysis and 9% were treated conservatively (unpublished data) . About two thirds of patients were triaged in the ambulance. Selective pre-hospital abciximab facilitation was available at the discretion of the emergency physician.
Definition of aborted and masquerading myocardial infarction
In all patients with the clinical diagnosis of ST-ACS, plasma samples for creatine kinase (CK), the CK-MB fraction and troponin I were collected before and after completion of the invasive procedure, and subsequently for CK and CK-MB every six to eight hours until they declined into the normal range, or to at least half of the maximum value. Troponin I was only redone after six to eight hours if baseline CK-MB was not elevated. After the baseline preprocedural ECG a second ECG was taken on the ICU within half an hour after completion of the invasive procedure. Further ECG’s were taken on an individualised basis. Early ST segment resolution was evaluated by the same observer on all first postprocedural ECG according to the Schroeder method6,7.
The definitions of aborted MI and masquerading MI were chosen in line with the analysis of the ASSENT 3 population by Taher et al4. Aborted MI was defined as maximum creatine kinase increase <2 times upper limit of normal combined with typical evolutionary ECG changes. Although the contemporary universal definition of myocardial infarction is based on CK-MB- or troponin measurements there is no such definition of aborted MI published yet. Masquerading MI was diagnosed if evolutionary ECG changes were missing or could be attributed to other causes. The latter condition was included because patients with Tako-tsubo syndrome are sometimes hard to distinguish from aborted MI by non-invasive means.
All patients were stratified according to the TIMI risk score8. A risk score >4 was used to identify a high risk population. Variables included in this score were age, Killip class >1, anterior infarction, time to treatment, history of hypertension and/or diabetes and/or pre-infarction angina, systolic blood pressure, weight and heart rate.
Patient inclusion and exclusion criteria
All consecutive patients with the clinical diagnosis of ST-ACS were included in this study. Patients however presenting with typical chest pain and unknown left bundle branch block (LBB) or persistent ST segment elevation of remote infarction without an invasive confirmation of intracoronary thrombus were not included in this observation, because the applied definition of aborted MI requires typical evolutionary ECG-changes, often difficult to diagnose in the presence of LBB or persistent ST segment elevation of remote infarction.
Analysis of TIMI flow and in-hospital left ventricular ejection fraction
All angiograms were assessed for pre- and postprocedural TIMI flow by the same observer who was not aware of the results of the laboratory test or the use of facilitation. Left ventricular ejection fraction was determined either echocardiographically or angiographically. Patients were classified to have either normal (>55%), mildly impaired (45–54%), moderately impaired (30-44%) or severely impaired left ventricular systolic function (<30%) after the intervention. In case of several consecutive echocardiograms the latest was considered for this analysis.
Cardiac magnetic resonance
All measurements were done on a 1.5 Tesla Excite HD magnetic resonance tomograph (General Electrics) using Magnevist as the contrast medium. Left ventricular ejection fraction, wall movement and delayed enhancement were determined according to standard protocols (wall movement: gradient echo SSFP, TE 1.5 ms, TR 3.5 ms, FOV 40×40 cm, matrix 224×224 px, thickness 8 mm; delayed enhancement: gradient echo, TE 3.1 ms, TR 6.6 ms, TI 200-260 ms, FOV 40×40 cm, matrix 256×192 px, thickness 8 mm).
Data collection and follow-up
All clinical and procedural data were collected in a commercial database according to hospital standards. The hospital quality assurance standard includes a follow-up of all patients after PCI. The responsible Ethics Committee was informed about the extension of clinical data collection for this observational study with follow-up after 30, 180 and 360 days. A formal ethical vote was not demanded. Patients were informed about and asked for the additional follow-up items in writing.
Statistical methods
The statistical analysis was performed using SPSS Version 15.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were summarised as medians with interquartile ranges or mean ±standard deviation for continuous variables as appropriate, and the Mann-Whitney U test was used. For categorical variables, data were summarised in percentages and the Fisher exact test was used.
In a subsequent step of the analysis a binary logistics regression model with additive factors was applied to define predictors of aborted myocardial infarction. The results were calculated using the SPSS procedure “Logistic Regression” with a “Forward” inclusion technique. Included were variables that significantly increased the Maximum Likelihood Statistic (p<0.05), the exclusion criterion was that the variable was not significant at the 10% level. The algorithm terminated after four iterations, no variables were excluded during the stepwise process. The following variables were considered potentially significant in the model: age; gender; cardiovascular risk factors including diabetes; serum creatine; blood glucose; c-reactive protein: medical therapy at admission: acetylicsalicylic acid, clopidogrel, fractionated and unfractionated heparin, anticoagulants, beta-blockers, Ca antagonists, nitrates, lipid lowering drugs, ace-inhibitors, antiarrhythmic drugs; application of abciximab and abciximab facilitation; extent of coronary artery disease; culprit vessel; success of PPCI; pre- and post-interventional TIMI flow; symptom-to-balloon-time and first medical contact-to-balloon-time; use of stents and use of drug eluting stents during PPCI.
Results
Between October 1st, 2005, and September 30th, 2006, 196 patients were scheduled for mechanical reperfusion with the clinical diagnosis of acute ST-ACS (<12h). Of the total cohort, 34 patients (17,3%) fulfilled the criteria of aborted MI, 20 of them (58,8%) had been transferred for more than 20 km. Nine patients (4.6%) were diagnosed as masquerading MI and 153 (78,1%) patients experienced a complete MI. Out of the masquerading MI group six patients had Tako-tsubo syndrome, two patients pericarditis and one patient suffered from subarachnoidal haemorrhage admitted after cardiopulmonary resuscitation with anterior ST-segment elevation9. After a median of 12 months, we could perform a cardiac MR in 16 out of 26 aborted MI patients who did not have a history of MI before or after the index event (Figure 1).
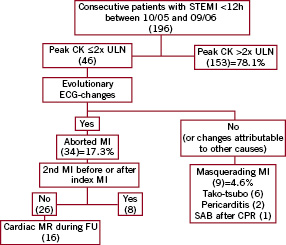
Figure 1. Identification of aborted and masquerading myocardial infarction (MI) from 196 consecutive patients admitted for primary angioplasty. CK: creatine kinase; CPR: cardiopulmonary resuscitation; ECG: electrocardiogram; FU: follow-up; MR: magnetic resonance; SAB: subarachnoidal haemorrhage; STEMI: ST-elevation myocardial infarction
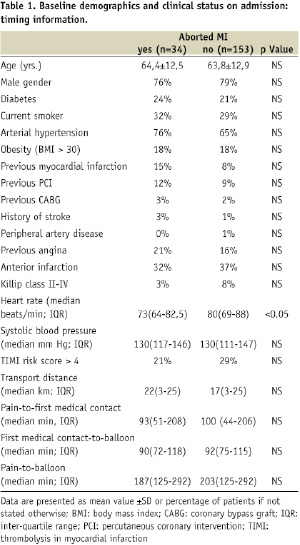
Keeping in mind the limited statistical power of the given sample sizes, there were no significant differences in demographics, cardiovascular risk factors and clinical status on admission between patients with aborted or complete myocardial infarction with exception of a lower median heart rate on admission in the aborted MI group. Correspondingly the number of patients with more than Killip class 1 was higher in the non-aborted group (Table 1).
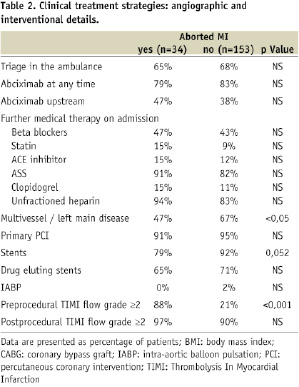
With respect to angiographic presentation features there was a highly significant difference between the two groups concerning pre-interventional TIMI flow. Moreover, we found significantly less multivessel or left main disease in the aborted MI group (Table 2).
There was no significant difference in the clinical management of the two groups. The frequency of aborted MI however was numerically higher if angioplasty was performed within the first two hours of symptoms compared to revascularisation after more than two hours (Figure 2).
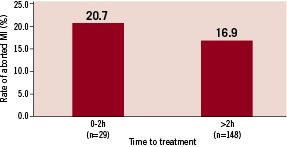
Figure 2. Rate of aborted myocardial infarction according to time from symptom onset to treatment. HR: hour; MI: myocardial infarction; NS: no significant difference between both groups
Moreover, we found a higher percentage of abciximab facilitation and a lower percentage of patients with necessity for angioplasty + stent or intra-aortic balloon pump (IABP) support in the aborted MI group.
After application of a multivariate logistic regression model pre-interventional TIMI 2 or 3 flow remained the only independent positive predictor of abortion of myocardial infarction. Negative predictors were multivessel or left main disease, the use of stents or a longer first medical contact-to-balloon time (Table 3).
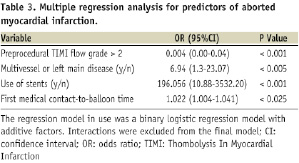
The sample sizes however were not powered to reliably exclude other factors.
While the definition of aborted MI is historically based on the lack of a significant CK-increase we could identify only six patients in the aborted group that did not even have a significant troponin increase. Of these patients, four had cardiac ventriculography after coronary angiography that showed acute regional wall movement abnormalities. Five out of six (5/6) received a primary PCI, only one of six (1/6) had no significant stenosis or thrombus.
Abortion of myocardial infarction translated into significantly higher rates of complete early ST-segment resolution and preserved LV-function during the hospital stay as well as a numerically lower in-hospital and one year mortality (Table 4).
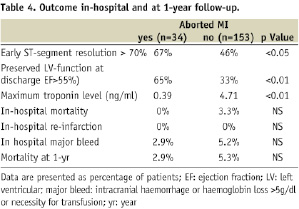
After a median of 12 months, 16 patients of the aborted MI cohort, without a second infarction prior to or after the index event, had a cardiac MR. In all of those patients we found a preserved global left ventricular function, 11 patients had no wall movement abnormalities and in six patients detectable late enhancement was not seen.
Discussion
The main finding of the present study is that an aborted myocardial infarction (CK-based enzymatic definition) can be found with a similar frequency after primary PCI as described for pre-hospital thrombolysis2,3, even in transfer patients. Preprocedural TIMI flow 2 or 3 is its main predictor. An enzymatically aborted MI corresponds to small or even non-detectable scar formation in terms of late enhancement on cardiac MR, and results in a low one year mortality.
Preprocedural TIMI flow and aborted MI
For primary PCI, the positive prognostic significance of preprocedural restoration of normal flow in the infarct related artery has been described previously10,11. High-risk patients especially seem to profit12. Consistent with the findings of Brodie et al, we found a significant relationship between preprocedural TIMI flow and enzymatic infarct size as well as pre-discharge ejection fraction11. Our observation of preprocedural TIMI flow grade 2 or 3 being a highly significant predictor of aborted MI is in accordance with this, as well as the observed low mortality after abortion of MI. These findings may reflect that the duration of coronary occlusion is a main determinant of myocardial infarction size as demonstrated in animal models13-15 and, furthermore, that a delay in reperfusion may result in a higher incidence of distal embolisation or no reflow with less postprocedural TIMI flow grade 316,17. The fact that we observe a substantial number of aborted myocardial infarctions in ST-ACS patients even hours after the onset of symptoms, although 40 to 50% of myocardium at risk are dead by 90 minutes of coronary occlusion in the animal models13-15, suggests a mechanism of spontaneous - perhaps intermittent - reperfusion in some infarct related arteries, which might induce some degree of preconditioning, before final clot resolution or removal stabilises the situation, or final clot occlusion occurs. If abortion of myocardial infarction is possible, even hours after the onset of on-going symptoms, and given the higher success rate of primary PCI to restore good post interventional TIMI flow18, this observation might partially explain why the relationship between time to treatment and myocardial salvage in respect to mortality is weaker in the PPCI as compared to the thrombolysis setting19-21. The fact that we could identify a short first medical contact-to-balloon time, but not a short pain-to-balloon time as a predictor of aborted MI might reflect, among others, logistic factors such as described before22,23.
Facilitation with upstream abciximab
If preprocedural TIMI flow has a crucial importance for infarction size and outcome of ST-ACS patients, any kind of upstream pharmacological therapy increasing the early patency rate of an infarction related artery might be potentially beneficial, especially in patients with short symptom duration. However, in our small study we could not detect a significant effect of abciximab facilitation on the rate of aborted MI.
Masquerading MI
Despite exclusion of patients with left bundle branch block and ST elevation of remote infarction from the analysis, we found nearly 5% of masquerading MI in the study population. With the use of lytic therapy, this would translate into the same amount of unjustified thrombolysis. The majority of these masquerading MI patients had Tako-tsubo syndrome24. Their spontaneous ECG evolution, in combination with a moderate troponin increase, often mimics perfectly an aborted MI if no invasive diagnostic is performed.
Study limitations
The main limitation of our study is the rather small size of the aborted MI cohort affecting the results of the multiple regression analysis with respect to weaker influence factors. While we could show the effects of some factors, the sample sizes are not enough powered to exclude definitively the importance of other factors. Furthermore, there was no continuous 12 lead ST-elevation monitoring of transfer patients, which might have identified the spontaneous frequency of ST elevation resolution and re-elevation before intervention.
Clinical implications and conclusions
Although primary angioplasty has proven to be superior to thrombolysis in most circumstances2,25, some questions remain under debate. Abortion of myocardial infarction in ST-ACS patients with short duration of symptoms is an especially strong argument for pre-hospital thrombolysis in early patients. Our study shows that there is a comparable proportion of aborted MI after primary PCI. Furthermore, the number of masquerading MI potentially leading to unjustified thrombolysis is not negligible. However, as we found that pre-interventional TIMI flow grade 2 or 3 is the main predictor of abortion in ST-ACS, this favourable course seems to be related rather to spontaneous reperfusion and perhaps a preconditioning phenomenon, than to revascularisation itself. If this holds true, it would be worthwhile to study in greater depth the variables that predict spontaneous reperfusion. Considering this, the facilitation concept seems appealing, especially in early patients. Nevertheless, we could not identify abciximab facilitation as a significant factor for abortion. This might be due to the small numbers and presentation delays. On the other hand, it fits with the results of the FINESSE study, which could not prove a significant effect of facilitation on clinical endpoints26; neither did the ACUITY trial in non ST-elevation acute coronary syndromes27. Both studies did not, however, specifically address those patients with very short symptom duration in which facilitation might be more beneficial20.
From our findings we conclude that targeting for abortion of myocardial infarction is no argument for or against a specific revascularisation method.
Acknowledgements
We gratefully acknowledge Mr. Alfred Müller (Analytic Services GmbH, Munich, Germany) for the statistical analysis of the data. We would also like to thank Mrs. Karolin Schneider for the database management.

