Abstract
Aims: Chronic total occlusions (CTO) secondary to in-stent restenosis (ISR) represent challenging lesions with low PCI success rates. The CrossBoss is an over-the-wire blunt catheter which has emerged as a useful tool in occlusive ISR. We aimed to review the utility of this device in the treatment of occlusive ISR within the United Kingdom.
Methods and results: The CrossBoss catheter was used as the primary strategy in 30 patients (31 CTOs) with a median CTO duration of 24 months, a mean CTO length of 39 mm and a previous unsuccessful PCI attempt in 48% of cases. Procedural success was 90% (27/30) and the CrossBoss catheter directly facilitated success in 81% of cases, with direct lumen-to-lumen crossing of the catheter in most cases. Identifiable predictors of failure were evident in the unsuccessful cases. When successful, crossing time was short (median eight minutes, range one to 40 minutes), as were procedural time (mean 99±29 minutes) and fluoroscopy time (mean 26.9±12.2 minutes), whilst radiation dose (median 5,738 cGycm2, range 3,430-64,122 cGycm2) and contrast dose (mean 271±79 mL) were low. There were no procedural complications.
Conclusions: In our experience, use of the CrossBoss catheter is associated with high procedural success rates, short crossing times and low complication rates in the setting of occlusive ISR.
Introduction
Occlusive in-stent restenosis (ISR) represents the most severe type of ISR1 where neointimal hyperplasia from vascular smooth muscle cell proliferation completely obliterates the stent lumen2. It is a rare entity, representing only 5-10% of CTOs treated in contemporary practice, but the majority of cases are symptomatic, usually with stable angina3, and thus merit consideration for further revascularisation. Given that patients with chronic total occlusions (CTOs) caused by ISR are usually excluded from clinical trials, little published data exists to guide coronary intervention in this setting. Nonetheless, limited reports and anecdotal experience indicate they represent difficult interventions with low procedural success rates4-6. The most common failure mode is an inability to cross the lesion with a guidewire. CTOs due to ISR are composed of a hypocellular matrix made up primarily of hard and resistant collagenous material, and differ from other CTOs in that they have a relative absence of microchannels, thus explaining the lower success rates evident with soft, tapered wires. Penetrative wires with high tip loads are therefore commonly employed in this setting but often result in substent wire passage, precluding subsequent device delivery, even if the distal true lumen has been successfully wired. Previous reports have described some success with the Frontrunner device (Cordis Corporation, Bridgewater, NJ, USA)7 and optical coherence reflectometry wires8, but neither is now commercially available.
The CrossBoss™ (Boston Scientific, Natick, MA, USA) is a 6 Fr-compatible, over-the-wire catheter (Figure 1A and Figure 1B) with a blunt, atraumatic 3 Fr (1 mm) tip that is advanced ahead of the coronary guidewire into the lesion and rapidly rotated manually using the “fast spin technique” to allow crossing of the occlusion whilst remaining within the vessel architecture (either through the true lumen or by creating a controlled subintimal track). It was designed to allow crossing of CTOs in this manner and, if in the subintimal space beyond the distal cap of the CTO, to facilitate subsequent controlled luminal re-entry with the Stingray™ balloon (Boston Scientific). The utility of the CrossBoss catheter for refractory CTOs has been established in the FAST-CTOs trial9; however, ISR cases were excluded from this trial. Further evidence exists for these devices (CrossBoss catheter and Stingray balloon) in refractory CTOs in a prospective, multicentre European trial10; however, ISR cases were under-represented in this series with only one case included. Nonetheless, this represents the first description of the use of the CrossBoss catheter to treat an ISR CTO successfully. Support for use of the CrossBoss catheter in ISR CTOs exists in a small case series by Papayannis et al, who described a success rate of 83% (five of six patients) with this strategy11. The presence of stent struts in CTOs due to ISR tends to prevent device exit to the subintima and facilitates passage of the CrossBoss catheter’s blunt tip through the occlusion to the distal true lumen. Indeed, early clinical experience with the CrossBoss suggests it is well suited to this setting and often crosses the CTO from “lumen to lumen”10,11, thus negating the need for a re-entry strategy. We aimed to review its utility in the setting of occlusive ISR in the United Kingdom.
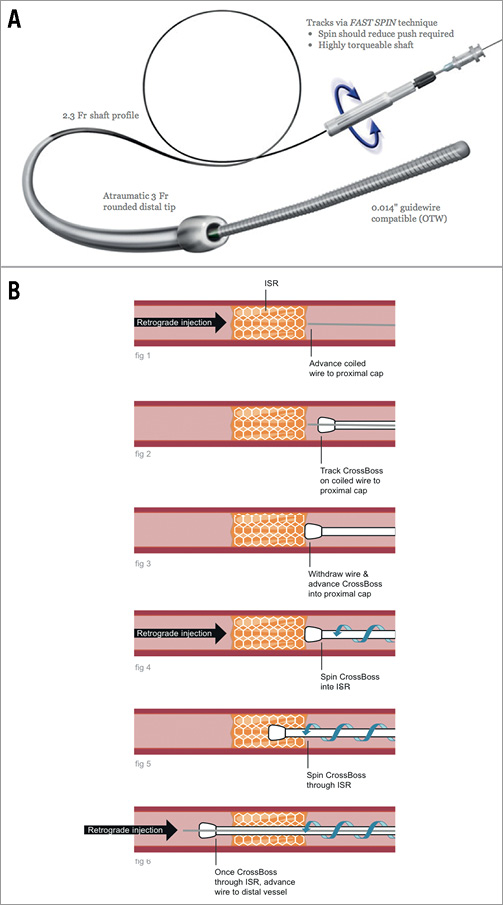
Figure 1. A) CrossBoss catheter (reproduced with permission of Boston Scientific). B) Use of the CrossBoss catheter in occlusive restenosis.
Methods
We retrospectively identified all cases with a CTO due to in-stent restenosis undergoing PCI at our respective institutions in the United Kingdom from January 2011 (when the CrossBoss catheter was first commercially available in the UK) to March 2013. A CTO was defined as the presence of TIMI 0 flow within the occluded segment and angiographic or clinical evidence (or high likelihood) of an occlusion duration of ≥3 months. CTO length and diameter were calculated by QCA. Chronic kidney disease was defined as an eGFR <60 ml/min/1.73 m2. Technical success was defined by a final TIMI 3 flow and <30% residual stenosis, whilst procedural success was defined as technical success without in-hospital major adverse events (including death, myocardial infarction, emergency coronary bypass surgery or stroke).
Continuous parameters are reported as mean±standard deviation or median±range when data were not normally distributed. Discrete parameters were reported as percentages. Comparison between subgroups was made using the Student’s t-test (unpaired). All analyses were performed using Stata 10 (StataCorp LP, College Station, TX, USA).
Results
Three hundred and forty-nine percutaneous interventions for chronic total occlusions were undertaken in the described time period in the authors’ institutions, of which 52 were identified as being due to occlusive restenosis. Thirty-one of these were managed with use of the CrossBoss catheter as the primary strategy (in 30 patients; one patient had two CTOs due to occlusive ISR). Their medical records and coronary angiograms were reviewed to define clinical and angiographic characteristics, success rates and predictors of failure.
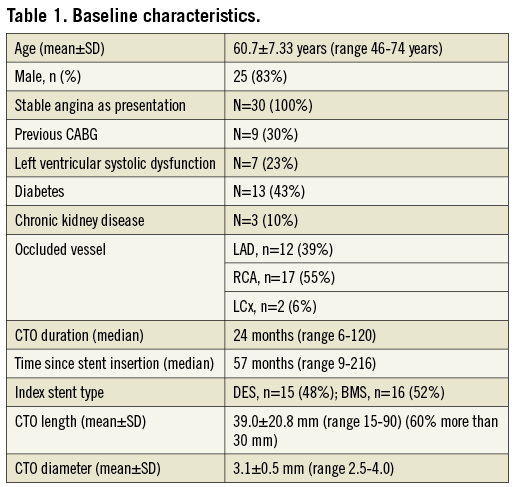
Baseline characteristics are presented in Table 1. A prior unsuccessful attempt at PCI to the CTO had been made in approximately half of the cases, with the common failure mode being due to an inability to cross with a guidewire. Guide catheters of at least 7 Fr were used (although the CrossBoss itself is 6 Fr catheter-compatible) and contralateral injections were used for visualisation in all cases.
Technical and procedural success for PCI with a strategy of initial CrossBoss catheter use was 90% (technical success 28/31, procedural success 27/30). The CrossBoss catheter directly facilitated success in 81% of cases (25/31), usually by passing from “lumen to lumen” (88% of “CrossBoss success” cases [22/25]), or otherwise by facilitating wiring of the distal vessel when the catheter had crossed at least part of the segment. The CrossBoss catheter frequently crossed the occlusion rapidly (median eight minutes, 40% of cases in under five minutes), in particular if it passed from “lumen to lumen”, but on occasion it was necessary to redirect the catheter within the occlusion using a penetrative (high tip load with a tapered tip) coronary guidewire. Anchor balloon support was required in one case of successful “lumen to lumen” crossing. Two representative successful cases are presented in Figure 2, Moving image 1 and Figure 3, Moving image 5. (Moving image 2-Moving image 4 are examples of other successful cases). Figure 4 demonstrates the “trap” balloon technique, which was used in all cases to remove the CrossBoss catheter once distal wire position (luminal or subintimal) had been achieved.
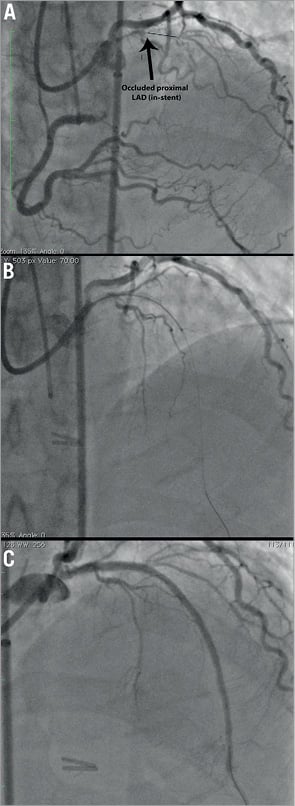
Figure 2. Example of successful case with “lumen to lumen” passage of CrossBoss catheter (Moving image 1). A 64-year-old male presented with 12 months of recurrent angina. He had undergone previous PCI to the LAD nine years prior and subsequent CABG x 1 (LIMA-LAD) for severe ISR eight years prior (subsequent graft failure). He now presented for elective PCI to the chronically occluded LAD due to in-stent restenosis (angiographically documented to be present for eight years). The occluded stent length and CTO length were 28 mm whilst the stent diameter was 2.5 mm. A) RAO cranial view with occluded proximal LAD (in-stent). Line marks length of occlusion. B) Successful CrossBoss catheter passage. Via a 7 Fr EBU 3.5 guide, a standard coronary 0.014 inch wire was used to direct the over-the-wire CrossBoss catheter to the proximal cap. With the wire withdrawn, the catheter was advanced into the occlusion using the “fast spin technique”. Subsequent direct passage of CrossBoss catheter to distal lumen (confirmed with contralateral injections) allowed easy passage of soft, polymer-coated wire through catheter to distal vessel. The CrossBoss catheter was then removed with the aid of a “trap” balloon (Figure 4) and the procedure completed in a normal manner. C) Final result after insertion of three drug-eluting stents.
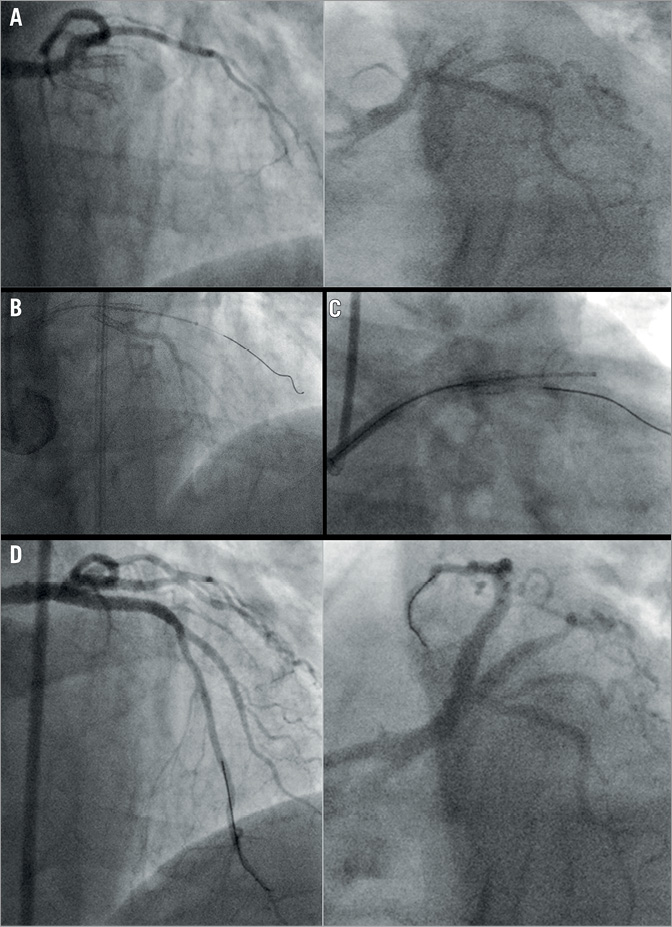
Figure 3. Example of successful percutaneous revascularisation of in-stent occlusions affecting the proximal LAD and ramus vessels in the same setting (Moving image 5). A) Pre-procedure angiogram (RAO cranial view on left, LAO caudal view on right) demonstrating proximal LAD and ramus in-stent occlusions. B) CrossBoss passage “lumen to lumen” into the ramus branch with subsequent wire passage to distal vessel through the CrossBoss catheter. C) CrossBoss passage “lumen to lumen” to LAD (with wire seen in ramus branch). D) Good final angiographic result (RAO cranial view on left, LAO caudal view on right).
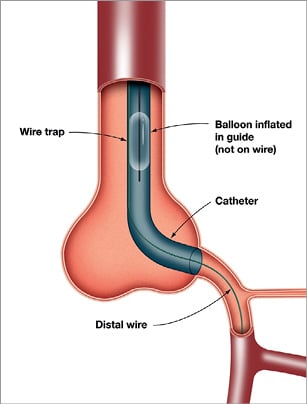
Figure 4. “Trap” balloon used to withdraw CrossBoss catheter safely once wire in distal lumen (or subintimal space prior to a re-entry manoeuvre).
For the overall group, procedural characteristics included (mean±standard deviation unless otherwise specified): procedure time 113.4±44.8 minutes (range 51-250), fluoroscopy time 29.6±15.1 minutes (range 7-67), dose area product (DAP) median 9,111 cGycm2 (range 3,430-64,122) and contrast dose 298±122 (range 180-750 ml).
Technical success was not achieved in three cases and the CrossBoss catheter did not directly facilitate success in six cases (termed “CrossBoss failure”). In the 25 cases where success was directly attributable to the CrossBoss, crossing time was short (median eight minutes, range one to 40 minutes), as were procedural time (mean 99±29 minutes, range 51-166 minutes) and fluoroscopy time (mean 26.9±12.2 minutes, range 7-50 minutes), whilst radiation dose (median 5,738 cGycm2, range 3,430-64,122 cGycm2) and contrast dose (mean 271±79 mL, range 180-440 ml) were low.
No differences in baseline characteristics existed between successful and “CrossBoss failure” cases. Of the six “CrossBoss failure” cases, four involved the right coronary artery, one involved the left anterior descending artery and one involved the circumflex artery. In these failure cases, mean procedural time was significantly longer (181±47 minutes, p<0.001), as was mean fluoroscopy time (48.4±12.8 minutes, p=0.003), whilst mean contrast use (424±210 ml, p=0.008) was greater.
There were no procedural complications.
“CROSSBOSS” FAILURE CASES
The CrossBoss catheter did not facilitate success in six cases, with a previous unsuccessful PCI attempt having been made in four.
Failure case 1 had undergone successful RCA PCI six years prior with the insertion of three drug-eluting stents (non-overlapping stents in the proximal, mid and distal vessels). Angiography confirmed occlusion of the RCA at the proximal aspect of the mid vessel stent due to ISR (Figure 5A and Figure 5B). Tortuosity between the proximal and mid vessels led to the CrossBoss catheter being directed into a side branch within the unstented segment just proximal to the occlusion, thus precluding successful passage of the CrossBoss catheter (Figure 5C). Percutaneous revascularisation was successful via a retrograde approach in the same setting (Figure 5D, Moving image 6).
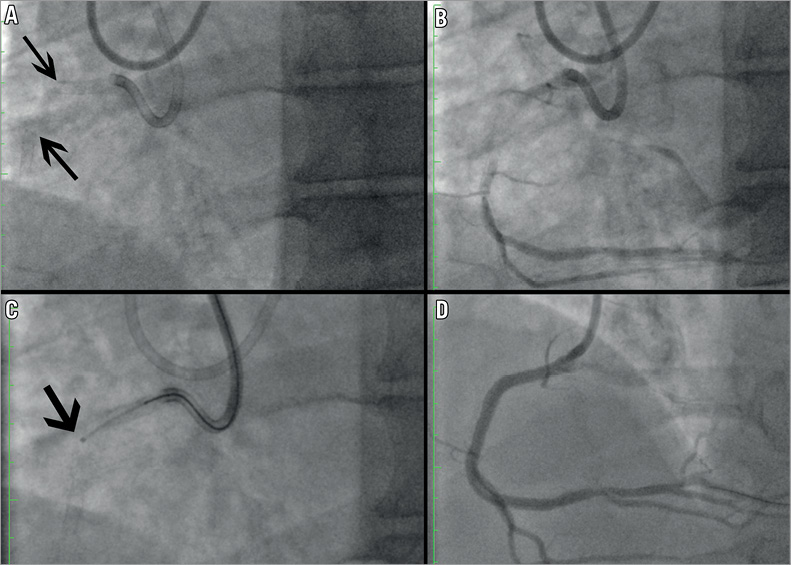
Figure 5. Failure case 1 (Moving image 6). A) Cine without contrast to illustrate stent positions. Occlusion at proximal aspect of second stent in mid RCA with hidden tortuosity between two stents (arrows point to distal aspect of proximal stent and proximal aspect of second stent). B) Angiogram demonstrating short occlusion in second stent. C) Unsuccessful passage of CrossBoss catheter into second stent (biasing owing to tortuosity – arrow points to CrossBoss tip distal to first stent). D) Final result after retrograde PCI.
Failure case 2 had occlusive ISR within two overlapping distal RCA bare metal stents inserted eight years previously. The occluded segment was 50 mm in length (occlusion involved entire length of stents with maximal diameter 2.5 mm at index PCI) (Figure 6A). The CrossBoss catheter negotiated approximately two thirds of the occluded segment before stalling and could not reach the distal aspect of the stented segment despite multiple attempts at redirecting the device with coronary guidewires and use of an anchor balloon (Figure 6B). Wire passage distal to the stent through the CrossBoss catheter was probably subintimal with subsequent unsuccessful distal-wire-based re-entry. Repeat angiography eight weeks later demonstrated an antegrade channel, which was easily wired, and successful PCI was performed. It is likely that the initial failure of the device to negotiate the occluded stents was due to tortuosity both in the proximal vessel and within the occluded segment (Moving image 7).
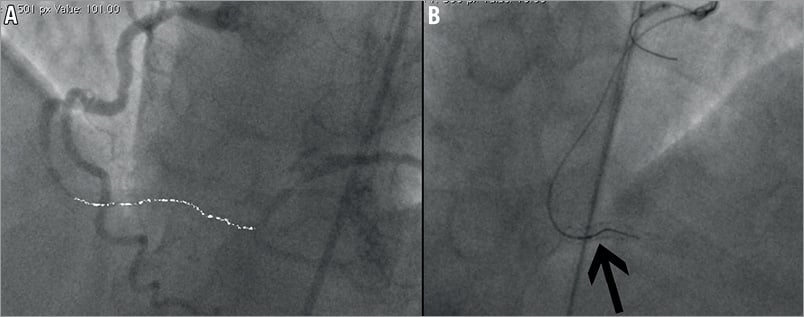
Figure 6. Failure case 2 (Moving image 7). A) Long segment distal RCA occlusion with proximal tortuosity (dashed line highlights length of in-stent chronic occlusion). B) CrossBoss passage into stent (arrow) with guide support from an anchor balloon, but inability to deliver further and subsequent subintimal passage of wire.
Failure case 3 was a long segment in-stent occlusion (~50 mm) in a circumflex artery (Figure 7A). The stents extended into a large second marginal vessel and jailed a moderate sized first marginal branch (OM1). The CrossBoss catheter tracked to the level of the OM1 with some difficulty (Figure 7B), which probably pertained to proximal circumflex tortuosity and poor guide catheter support. To facilitate further passage of the device, balloon angioplasty in the proximal segment was performed (2.0 mm balloon tracked over a wire which had passed into OM1). Balloon inflation across the stent struts into OM1 unfortunately meant the CrossBoss catheter subsequently tracked repeatedly into this branch, and attempted redirections with a stiff wire were unsuccessful. Passage of a stiff wire to the distal OM2 was achieved; however, it tracked subintimally distal to the stents (Figure 7C). The case was abandoned with a neutral outcome (Figure 7D, Moving image 8).
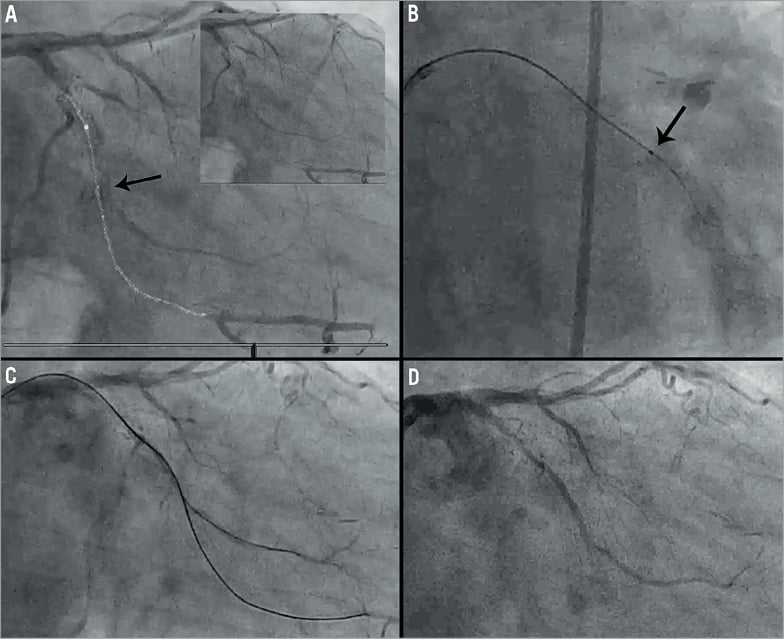
Figure 7. Failure case 3 (Moving image 8). A) Annotated pre-intervention angiogram, with white line highlighting course of vessel and black arrow indicating small OM1 jailed by stents (inset=angiogram without annotation). B) Black arrow indicates tip of CrossBoss catheter within occlusion at level of OM1. C) Wire passage into OM1 and subintimal wire in OM2. D) Final result with flow to small OM1 but persistent occlusion of OM2.
Failure case 4 was an ostial occlusion of an LAD stent where flush occlusion with angulation and lack of support precluded engagement of the CrossBoss catheter in the lesion (Figure 8). This case was completed successfully via a retrograde approach.
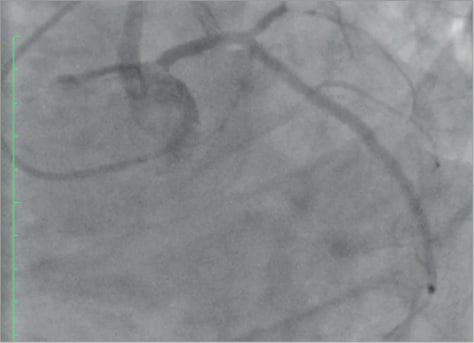
Figure 8. Failure case 4. Ostial LAD occlusion.
Failure case 5 involved occlusive ISR within two layers of stents, where one stent was previously inadvertently deployed through the side of another stent into the subintimal space in a complicated procedure, which resulted in a crush deformity of the distal aspect of the first stent (Figure 9). The vessel filled from contralateral collaterals to the “true” lumen, which was outside the double layer of previously inserted stents. The CrossBoss was unable to penetrate the proximal cap of this occlusion.
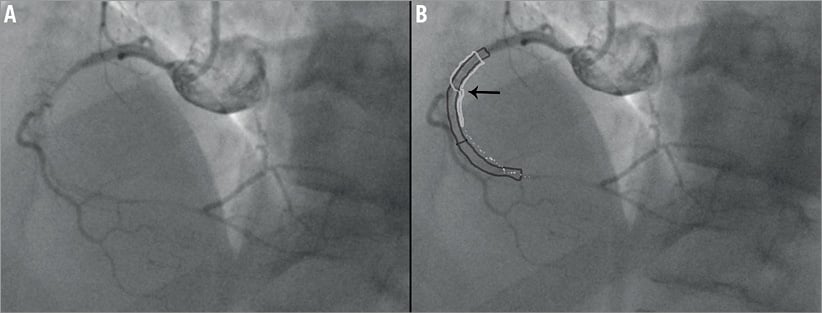
Figure 9. Failure case 5. A) Initial angiogram demonstrating long RCA in-stent occlusion. B) Annotated angiogram demonstrating arrangement of previously inserted stents. Initial stent is light grey with subsequent stents (dark grey) inserted inadvertently through side of this stent (arrow indicates where CrossBoss catheter stalled).
Failure case 6 was an occlusion within a long 40 mm segment of stents inserted into the distal RCA seven years prior. The CrossBoss catheter appeared to cross the entire stent length within 10 minutes; however, subsequent wire passage through the device was met with resistance, presumed related to subintimal tracking distal to the stent. The case was successfully completed in a retrograde fashion and IVUS imaging prior to balloon inflation and stent insertion demonstrated grossly underdeployed stents that extended further distally than initially appreciated. These stent struts were very difficult to identify on cine angiographic imaging alone. It is likely the mechanism of failure of the CrossBoss in this instance was not actually the device itself but an underappreciation of the stent length and a consequent early wire attempt to the distal vessel that likely tracked behind underdeployed stent struts.
Tortuosity (defined as a bend more than 45 degrees) within the stented segment probably contributed to failure in three cases, and was absent in most of the successful cases. Tortuosity proximal to the occlusion did not appear predictive of failure. CTO duration, vessel diameter (mean 3.1±0.5 mm, range 2.5-3.5 mm) and CTO length (mean 39±20 mm, range 15-80 mm) did not appear to predict CrossBoss failure. An additional previously reported predictor of failure9 in this setting is the presence of a side branch at the proximal cap and, although this can increase case complexity (in one of these cases, engagement of the CrossBoss catheter into the proximal cap was challenging and necessitated multiple redirections of the catheter with a wire), it was not a mode of failure in our series and indeed was present in two successful cases.
Discussion
PCI in CTO due to ISR has largely been reported to have a lower success rate than non-ISR CTO4-6. These low success rates exist despite previously placed stents serving as a “road map” of the course of the occluded artery as well as providing some protection against vessel perforation. Failure usually relates to inability to cross the lesion with a guidewire, with the hard proximal cap making lesion engagement and penetration difficult. Alternatively, failure can relate to substent wire passage, particularly with stiff, penetrative wire use, which prevents subsequent passage of balloons and stents. Reported predictors of failure of PCI in ISR CTO include longer duration of occlusion, smaller initial stent diameter and the presence of a large side branch at the proximal cap4,11. Previously reported techniques to optimise success rates in occlusive ISR cases include use of optical coherence reflectometry wires8, use of the Venture catheter (St. Jude Medical, St. Paul, MN, USA) with or without the Stingray wire4,11, and blunt microdissection with the Frontrunner device (Cordis), which is no longer commercially available7.
Blunt microdissection, often in a subintimal plane, is the principle underlying the CrossBoss catheter’s utility in CTOs. In non-ISR CTO lesions, it capitalises on the differential tissue properties between intraluminal plaque and the adventitia, allowing preferential disruption of the fibrocalcific plaque, thus preventing catheter exit through the outer arterial wall and facilitating rapid passage within the subintimal tract. A luminal re-entry strategy is therefore usually required in this setting. Conversely, the passage of the CrossBoss catheter in CTO lesions due to ISR is usually intraluminal with subintimal passage prevented by stent struts, thus precluding the need for a re-entry strategy as long as the distal cap of the CTO is either within or at the very end of the stent struts. Advantages of the CrossBoss catheter in this setting over its predecessors such as the Frontrunner device include its narrow diameter, which can afford delivery to the distal vessel, and its over-the-wire design which allows easy passage of a guidewire to the distal lumen once the CTO is negotiated (no need to withdraw the device and attempt to wire the track created through the occlusion as with other blunt microdissection devices). In addition, passage through the occluded segment is usually rapid, as evidenced by the short crossing and procedural times in our series.
Failure of the CrossBoss catheter was observed in six cases and contributing factors were evident in each, in particular the ostial location of a lesion and severe tortuosity within the occlusion. If tortuosity precludes further advancement of the CrossBoss catheter, often the track created by its passage can be explored subsequently with a polymer-coated wire whose lubricity facilitates advancement. An underlying mechanical issue relating to the initial stent deployment (such as gross underdeployment, stent fracture or stent deformation which may have contributed to the restenotic process) can also preclude successful CrossBoss catheter passage. Stent abnormalities such as these are likely over-represented in occlusive ISR. Thus, where possible, it is worth closely reviewing the angiograms of the initial case in detail to identify such issues (for example, those encountered in failure case 5). Furthermore, actions during the current procedure that cause alteration to stent geometry (such as balloon angioplasty to the stented segment out into the side branch as in failure case 4) can lead to failure through interruption of the “cage” which normally serves to contain the CrossBoss catheter. In no case did the CrossBoss catheter exit the side of a stent in our series (other than in the aforementioned failure). Certain stents are less radiopaque than others, which can hinder visualisation, particularly in overweight patients. Underestimation of stent length can lead to failure in a manner to that described in failure case 6, where resistance to wire passage through the CrossBoss lumen was met as the device was still within the occluded segment, but was misinterpreted as being due to subintimal passage distal to the occlusion. We have also recognised that severe calcification limits the utility of the CrossBoss catheter; however, this is less often an issue in occlusive ISR, except in the presence of significant calcification in the vessel proximal to the occluded segment.
Conclusion
In our experience, use of the CrossBoss is associated with high procedural success rates, short crossing times and low complication rates in the setting of occlusive ISR. While the CrossBoss catheter is designed for subintimal tracking, in CTOs due to ISR it can rapidly negotiate occluded segments as it deflects off-stent struts. This device is particularly suited to lesions with a tapered proximal cap without severe tortuosity. Certain adverse features, such as ostial occlusions, significant tortuosity, stent deformation and severe calcification may predict CrossBoss failure.
| Impact on daily practice CTOs due to ISR represent challenging lesions with low success rates using wire-based strategies alone. The CrossBoss catheter is very effective in this setting and frequently affords rapid crossing of the occluded segment, permitting direct wiring of the distal vessel without the need for a re-entry manoeuvre. It is especially effective in lesions with a tapered cap and without significant tortuosity or underlying stent abnormalities. |
Acknowledgements
The authors gratefully acknowledge imaging support provided by Adrian Brown.
Conflict of interest statement
C. Hanratty, S. Walsh, J. Strange, J. Hill and J. Spratt have consultancy agreements with Boston Scientific. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Representative successful case 1: angiogram in RAO cranial view demonstrating occluded LAD due to in-stent restenosis; CrossBoss catheter crossed occluded stent from “lumen to lumen” within minutes and 0.014 inch coronary guidewire has been passed through CrossBoss catheter to distal vessel; final result after insertion of three drug-eluting stents.
Moving image 2. Representative successful case 2: long segment RCA occlusion with rapid CrossBoss passage from “lumen to lumen” with successful distal wiring and a good final angiographic result.
Moving image 3. Representative successful case 3: proximal RCA in-stent occlusion with “lumen to lumen” passage of CrossBoss (initial redirection required with guidewire).
Moving image 4. Representative successful case 4: initial angiogram loops reveal long segment of stents in RCA with occlusion at level of RV branch; CrossBoss catheter tracked to the distal stent and afforded rapid wiring of the distal vessel with a good angiographic result.
Moving image 5. Representative successful case 5: successful CrossBoss use for two CTOs due to ISR (LAD and ramus) in one setting; direct “lumen to lumen” passage of CrossBoss catheter in both vessels with a good final result.
Moving image 6. Failure case 1: angiogram demonstrating short occlusion in second of three separate RCA stents. Unsuccessful passage of CrossBoss catheter into second stent (biasing owing to tortuosity).
Moving image 7. Failure case 2: long segment distal RCA occlusion with proximal tortuosity; CrossBoss passage to distal third of stent (with anchor balloon support) but inability to deliver further and subsequent subintimal passage of wire; procedure abandoned with neutral outcome; follow-up angiography at eight weeks reveals a track to the distal vessel with TIMI 2-3 flow; distal vessel was easily wired with a jacketed wire with a good final angiographic result.
Moving image 8. Failure case 3: long segment LCx occlusion with stents extending into large OM2; CrossBoss catheter to level of OM1; subsequent wire passage to OM1 and balloon of proximal track; unable to pass CrossBoss past OM1 but wire tracked distally and repeatedly in a subintimal plane; procedure abandoned with a neutral outcome.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Representative successful case 1: angiogram in RAO cranial view demonstrating occluded LAD due to in-stent restenosis; CrossBoss catheter crossed occluded stent from lumen to lumen within minutes and 0.014 inch coronary guidewire has been passed through CrossBoss catheter to distal vessel; final result after insertion of three drug-eluting stents.
Moving image 2. Representative successful case 2: long segment RCA occlusion with rapid CrossBoss passage from lumen to lumen with successful distal wiring and a good final angiographic result.
Moving image 3. Representative successful case 3: proximal RCA in-stent occlusion with lumen to lumen passage of CrossBoss (initial redirection required with guidewire).
Moving image 4. Representative successful case 4: initial angiogram loops reveal long segment of stents in RCA with occlusion at level of RV branch; CrossBoss catheter tracked to the distal stent and afforded rapid wiring of the distal vessel with a good angiographic result.
Moving image 5. Representative successful case 5: successful CrossBoss use for two CTOs due to ISR (LAD and ramus) in one setting; direct lumen to lumen passage of CrossBoss catheter in both vessels with a good final result.
Moving image 6. Failure case 1: angiogram demonstrating short occlusion in second of three separate RCA stents. Unsuccessful passage of CrossBoss catheter into second stent (biasing owing to tortuosity).
Moving image 7. Failure case 2: long segment distal RCA occlusion with proximal tortuosity; CrossBoss passage to distal third of stent (with anchor balloon support) but inability to deliver further and subsequent subintimal passage of wire; procedure abandoned with neutral outcome; follow-up angiography at eight weeks reveals a track to the distal vessel with TIMI 2-3 flow; distal vessel was easily wired with a jacketed wire with a good final angiographic result.
Moving image 8. Failure case 3: long segment LCx occlusion with stents extending into large OM2; CrossBoss catheter to level of OM1; subsequent wire passage to OM1 and balloon of proximal track; unable to pass CrossBoss past OM1 but wire tracked distally and repeatedly in a subintimal plane; procedure abandoned with a neutral outcome.

