Abstract
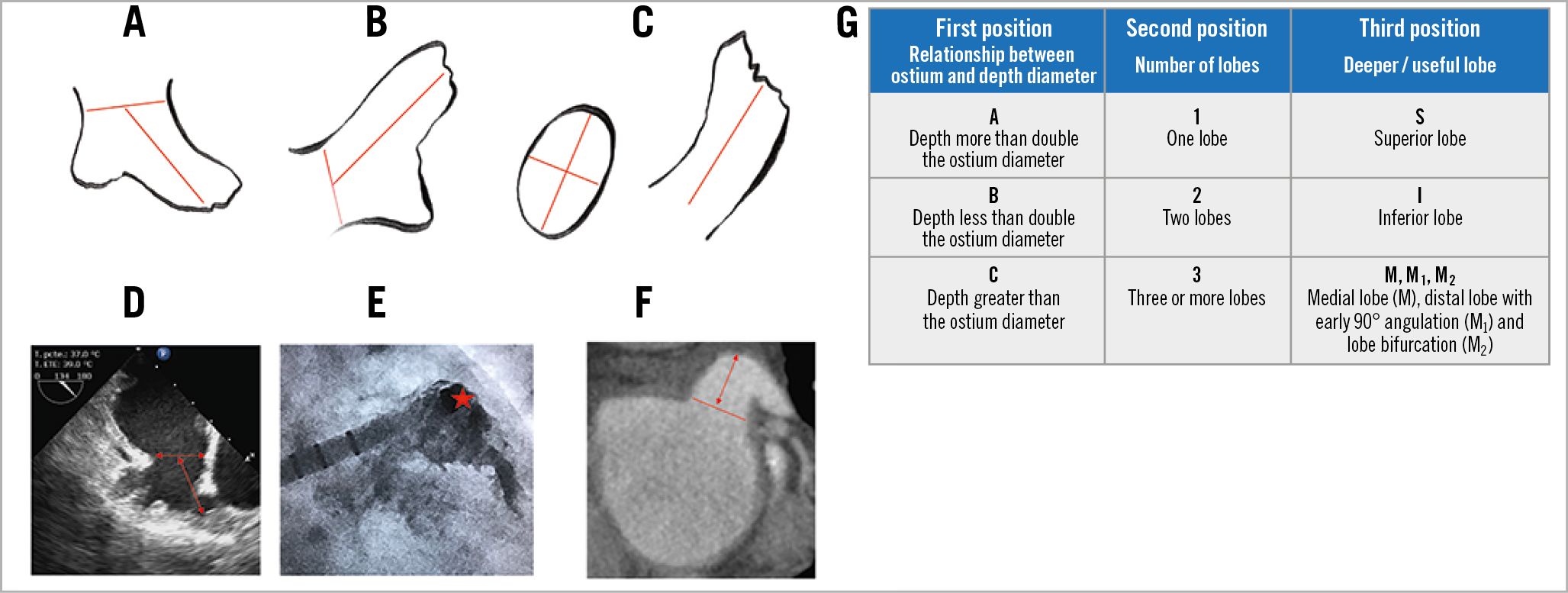
Figure 1. Step-by-step classification using LAA images from TEE, angioCT and angiography. A) TEE 135º view showing measurement of the landing zone and depth diameter. RAO 20º caudal 20º angiography (B) and angioCT axial and coronal views (C) in which the landing zone diameter can be obtained using either shorter and larger diameter media or the perimeter-derived diameter (PDD). D) B 2 S LAA sample in which the depth diameter is greater but less than double that of the landing zone diameter and so corresponds to B, has two lobes and so corresponds to 2, and the deeper useful lobe is superior. E) Catheter placed in the superior lobe perpendicular to the landing zone in the same B 2 S LAA. F) An angioCT B 1 M1 LAA sample with a distal inferior lobe with an early 90º angulation. G) The three variables and step-by-step positions forming the classification.
Left atrial appendage (LAA) is one of the major sources of thrombus formation in atrial fibrillation1. It presents a wide range of anatomical morphologies23.
The current morphological classification is subjective, comparing LAA with shapes such as Broccoli, Windsock, Chicken wing, Cactus and others. Even if some shapes have an impact in terms of prediction of procedure success4, an objective classification that allows planning the procedure better is needed. Additionally, an objective classification will avoid observer-dependent mistakes. Furthermore, some challenging shapes defined as rare are not included in the current classification.
The aim is to include all possible morphologies in a step-by-step classification with images obtained by transoesophageal echocardiography (TEE), angioCT and angiography using the landing zone diameter, depth, number of lobes and the dominant/useful lobe (Figure 1A-Figure 1C). We propose an intuitive classification which will have an impact on the procedure planning (Figure 1G). First, allocating a letter depending on the relationship between the landing zone and the useful depth diameter: “A” when the depth is more than twice that of the landing zone, “B” when the depth is less than double, and “C” when the landing zone is greater than the depth. Nitinol cage devices need at least the same depth as the landing zone diameter; therefore, A and B types will be more suitable (Figure 1D, Figure 1E). C types will be more suitable for plug devices. Second, a number will be allocated depending on the number of lobes, and third another letter will be allocated depending on which is the deeper/useful lobe for placing the catheter and implanting the device (deeper is not always the most useful lobe): “S” for superior lobe, “I” for inferior, and “M” when the deeper/more useful lobe is medial with three possibilities – absence of other lobes “M”, “M1” when the distal lobe starts with an early (less than 20 mm from the landing zone) 90º angle (Figure 1F), and “M2” when the LAA has two lobes with early bifurcation (less than 15 mm from the ostium) in which none of the lobes is useful. In an LAA with a deeper/useful superior lobe, an inferior/posterior transseptal puncture will be helpful in order to reach it and for manoeuvring the catheter inside the LAA (Figure 1E); when a useful/deeper lobe is inferior (“I”), a medial transseptal puncture will be more useful.
This new classification makes the description of LAA simpler, a factor which is strategically significant when facing the choice of closure technique, choosing a strategy and assessing its results. It will also be useful for criteria unification in further trials.
Conflict of interest statement
L. Cressa receives fees/honoraria from Boston Scientific and Abbott Vascular, and is a consultant for Boston Scientific. The other authors have no conflicts of interest to declare.