A 71-year-old male patient underwent PCI for an occluded everolimus-eluting stent implanted 17 months earlier (Figure top panel A). Following balloon angioplasty, directional atherectomy was performed to aid in-stent placement. After five cuts the atherectomy catheter could only be withdrawn with considerable resistance, retrieving a deformed stent containing neointima (Figure bottom panel). Angiography confirmed the absence of the stent and a patent LAD without contrast extravasation, but with hazy borders (Figure top panel B). Endovascular imaging showed a dissected LAD with intraluminal flaps (Figure middle panels A-D) that were successfully stented (Figure top panel C). The patient showed no symptoms or biomarker release during and after the procedure. Histology of stent and atherectomy tissue showed an inhomogeneous distribution of heavily vascularised myxoid and fibrous tissue containing both old (hemosiderin) and recent (erythrocyte ghosts) neointimal bleeding. Six month follow-up angiography showed a nice result (Figure top panel D).
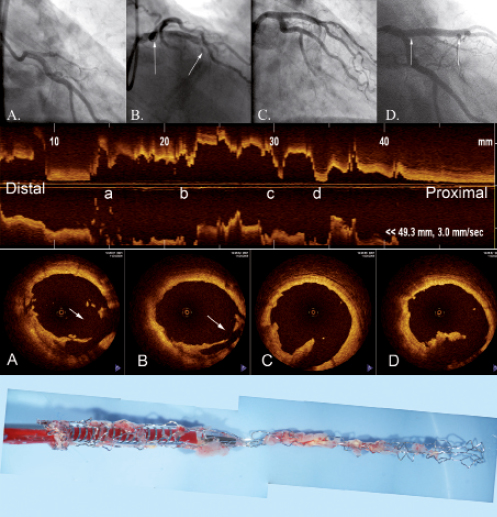
Figure 1. Top panel: angiogram of procedure; middle panel: OCT imaging; bottom panel: deformed stent containing neointima.
Conclusion
Atherectomy can be useful to reduce in-stent neointima burden prior to stenting for in-stent restenosis.1 Stent removal by atherectomy is a rare complication.2 The present case illustrates substantial intimal damage but without transmural vascular disruption.
Conflict of interest statement
The authors have no conflict of interest to declare.

