Introduction to the session
This summary report aims to capture the content of the session at EuroPCR 2018 that reviewed the implications for clinical practice of the CULPRIT-SHOCK trial, in order to share a critical analysis of the trial and report the views expressed in the interactive discussion. This article does not constitute an independent review of the topic by the authors.
The CULPRIT-SHOCK study1 tested the hypothesis that percutaneous coronary intervention (PCI) of culprit lesion only, with the option of staged revascularisation of non-culprit lesions, would result in better clinical outcomes than immediate multivessel PCI in patients with multivessel coronary artery disease and acute myocardial infarction with cardiogenic shock.
Trial headlines indicated that this study is a landmark study and a “game changer” for clinical practice, similarly to the IABP-SHOCK2 study that has resulted in a large reduction in the use of intra-aortic balloon pump (IABP) in patients with cardiogenic shock. IABP is nevertheless still used in 25-40% of cardiogenic shock cases. Will the results of CULPRIT-SHOCK follow the same path or will they change our practice?
The case presentation
A 67-year-old man was admitted to a tertiary hospital with non-ST-segment elevation myocardial infarction (NSTEMI) complicated by cardiogenic shock during the first day of admission, prior to revascularisation.
The coronary angiogram showed a distal left main with some haziness due to a large amount of thrombus involving mainly the proximal left anterior descending artery (LAD), which was patent with Thrombolysis In Myocardial Infarction (TIMI) flow 2, and a totally occluded left circumflex atery (LCx), with no distal collateral filling.
Background: what was known before the CULPRIT-SHOCK trial?
Previous studies on cardiogenic shock have shown a gradual increase over recent years, from about 7 to 10%, of patients with STEMI and cardiogenic shock. Despite early revascularisation, mortality remains extremely high, particularly in patients older than 75 years. The original SHOCK trial3 showed that early revascularisation by PCI or coronary artery bypass grafting (CABG) reduced mortality when compared with the initial medical stabilisation arm. In this study, 36% of patients in the revascularisation arm were treated by CABG with a median delay of 2.7 hours, and 64% by PCI with a median delay of 54 minutes. Though the trial spanned the era of the introduction of stents and GP IIb/IIIa inhibitors, there was no trend to additional benefit with the newly introduced PCI strategies and the one-year-mortality was similar over time4.
Recent data from a large German registry5 showed that, in patients with cardiogenic shock, the time elapsing from the first medical contact to primary PCI was a strong predictor of an adverse outcome. Hence, special efforts to shorten contact-to-balloon time should be implemented, especially in these high-risk patients.
Two recent meta-analyses6,7 of 10 observational studies concluded that, in patients with acute myocardial infarction and multivessel coronary artery disease complicated by cardiogenic shock, culprit-only PCI was associated with short-term, but not long-term benefit.
However, in spite of almost two decades of research since the SHOCK trial, no other strategies have been shown to improve outcomes convincingly, including trials of new pharmacological approaches or mechanical circulatory support2.
Trial analysis: summary of the trialists’ critical review
The study design (Figure 1) and results of the CULPRIT-SHOCK trial (Figure 2A, Figure 2B) are included.
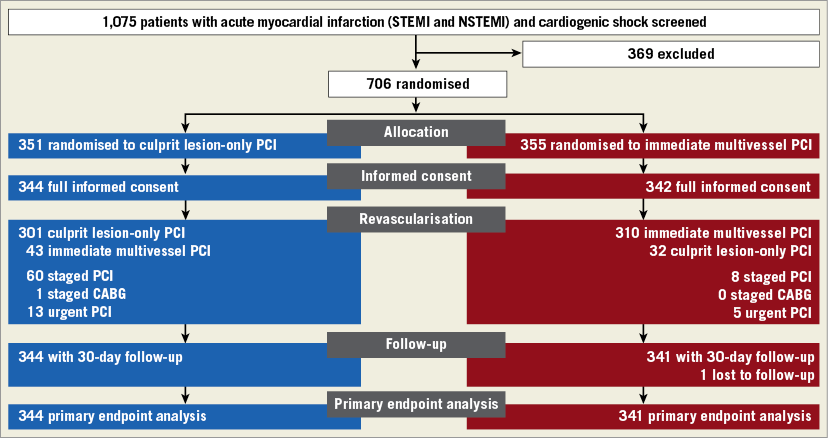
Figure 1. Study flow chart.
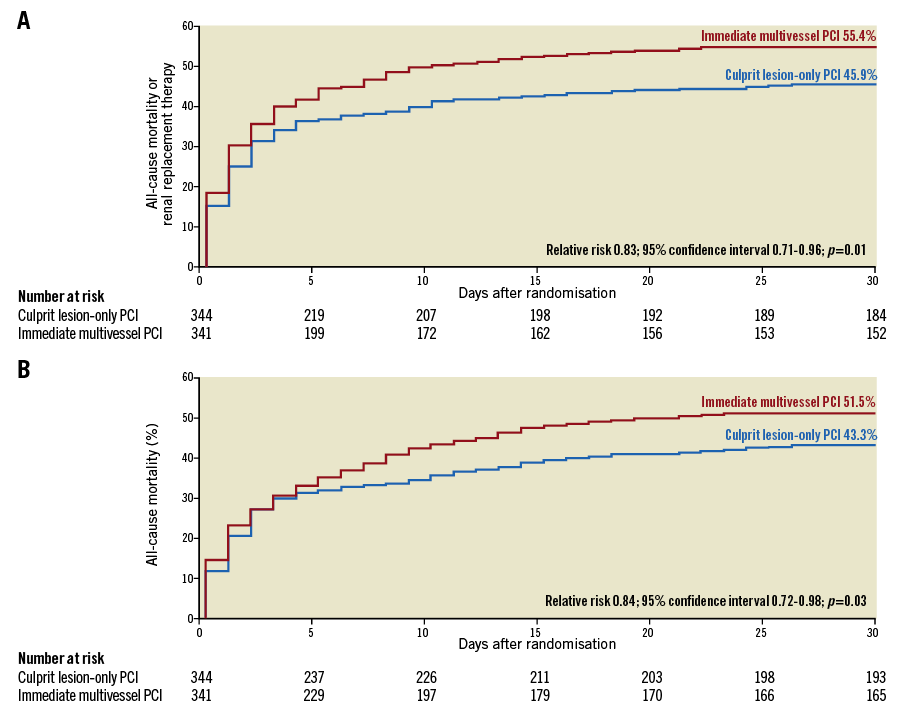
Figure 2. Results of the CULPRIT-SHOCK trial. A) Primary composite endpoint at 30 days. B) Mortality at 30 days.
In this multicentre trial, 706 patients who had multivessel disease, acute myocardial infarction, and cardiogenic shock were randomly assigned to one of two initial revascularisation strategies: either PCI of the culprit lesion only, with the option of staged revascularisation of non-culprit lesions, or immediate multivessel PCI.
At 30 days, the composite primary endpoint of death or renal replacement therapy had occurred in 158 of the 344 patients (45.9%) in the culprit lesion-only PCI group, and in 189 of the 341 patients (55.4%) in the multivessel PCI group (relative risk, 0.83, 95% confidence interval [CI]: 0.71 to 0.96; p=0.01). The reduced composite endpoint in the culprit lesion-only PCI group was mainly driven by a lower mortality at 30 days. The relative risk of death in the culprit lesion-only PCI group as compared with the multivessel PCI group was 0.84 (95% CI: 0.72 to 0.98; p=0.03), and the relative risk of renal replacement therapy was 0.71 (95% CI: 0.49 to 1.03; p=0.07). The time to haemodynamic stabilisation, the need for catecholamine therapy and the duration of such therapy, the levels of troponin T and creatinine kinase, and the rates of bleeding and stroke did not differ significantly between the two groups.
In contrast with previous trials involving highly selected patients with stable infarction, this trial did not specify the presence of a chronic total occlusion as an exclusion criterion. Therefore, in the multivessel PCI group, immediate recanalisation of a chronic total occlusion was recommended. However, it was also advised to limit the total dose of contrast to 300 ml. Complete revascularisation was achieved in 81% of the patients in the multivessel PCI group.
It was concluded that this study has definitively challenged the most recent ESC guidelines, suggesting that PCI of the non-culprit vessel should be considered in STEMI patients with cardiogenic shock (class IIa, level of evidence C)8. Moreover, mechanical circulatory support was used in only ~28% of the patients and IABP was used in 27% in the multivessel PCI group. It is still a matter of debate whether a higher use of mechanical circulatory support could determine better outcomes in these patients.
The case resolution and the practitioner’s view
Treatment of the case presentation patient was revealed: PCI with manual thrombectomy in the LAD, followed by left main-LAD and LCx T-stenting with a good angiographic result. An IABP was introduced after the PCI. The patient died after three days in the intensive care unit. Despite increasing catecholamine infusion and IABP, the systolic blood pressure was 80 mmHg and the LV systolic function remained severely depressed (EF: 10% by transthoracic echocardiography [TTE]). The patient passed away from cardiac arrest after ineffective resuscitation attempts.
It was mentioned again that IABP is not helpful in cardiogenic shock, as shown in the IABP-II trial; however, not all the interventional centres have access to the different mechanical circulatory support alternatives. Manual thrombectomy was used in this case, although routine thrombectomy is discouraged in the 2017 ESC Guidelines (class III recommendation) after the results of the TASTE9 and TOTAL studies10. Of note, even in patients with very high thrombotic risk or high thrombus burden from the TASTE subgroup analyses, no benefits of manual thrombectomy were observed.
Further discussion focused on the possible treatment strategies for the case patient. Multivessel PCI seemed to be the most reasonable revascularisation strategy in this case. The audience and the panel were split among the possibilities of using mechanical circulatory assistance by IABP, ECMO or Impella® (Abiomed, Danvers, MA, USA). At the moment there is little supporting evidence, and future randomised studies would be required to evaluate the potential benefit of early application of the different available mechanical circulatory support systems. The best timing also remains to be defined - whether just before or just after PCI.
Conclusions
The results of this trial support the clinical practice where PCI in culprit lesion-only with possible staged revascularisation is the most commonly selected option. The recent available randomised trials11,12 that have shown a benefit of multivessel PCI in STEMI patients have excluded patients with cardiogenic shock. CULPRIT-SHOCK was a randomised trial including challenging real-life patients with a “real-life” primary endpoint that has been shown to be significantly improved by PCI of the culprit lesion only. The results of this study have been integrated into the recently published update of the ESC guidelines13 with the following summary key points.
In patients with cardiogenic shock complicating STEMI and NSTEMI:
−Primary PCI should routinely be restricted to the infarct-related artery (IRA).
−Immediate multivessel PCI may be justified if the IRA is difficult to identify or incorrectly defined initially or when multiple culprit lesions are identified.
−Immediate multivessel PCI may be justified in selected cases in which there is a flow-limiting non-IRA with very severe stenosis irrigating a large myocardial area.
−Staged non-IRA PCI might be an option, carefully balancing the benefits and risks.
Conflict of interest statement
G. Sarno has received institutional research support from Boston Scientific. A. Chieffo has received speaker’s fees from Abiomed. C. Spaulding has received speaker’s fees from Abiomed and is a consultant for Medtronic. S. James has received institutional research support and lecture fees from Boston Scientific, Abbott Vascular, Biotronik and Terumo. The other authors have no conflicts of interest to declare.