Case 1
A 66-year-old male with prior coronary artery bypass (CABG) and chronic lung disease presented with class III dyspnoea. Echocardiography (TTE) confirmed severe aortic stenosis with a left ventricular ejection fraction (EF) of 30%. He was deemed unsuitable for conventional surgery. Warfarin (for low EF) was discontinued five days prior while 600 mg of clopidogrel and 325 mg of aspirin were loaded three hours before transcatheter valve implantation (TVI). Heparin (5000 IU) was administered during the procedure. Asize 23 mm Edwards SAPIEN™ (Edwards Lifesciences Inc., Irvine, CA) valve was implanted. Post implant echocardiography showed thrombi on the valve (Figure 1 A) hence heparin was continued. Three days later, the patient had acardiovascular arrest. Telemetry revealed sinus arrest with a slow ventricular escape. Cardiopulmonary resuscitation was unsuccessful. An autopsy showed that the valve was well seated with good cusp mobility and no pericardial effusion. Thrombi were however seen on the stent frame (Figure 1 B)
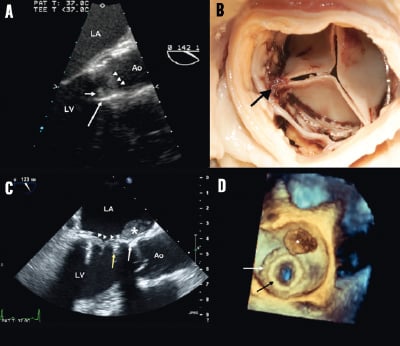
Figure 1. Panel A: Transesophageal echocardiogram of patient 1. Left ventricular outflow tract seen in the long axis demonstrating the stent (long white arrow), thrombus on the stent (short white arrow) and the thickened valve leaflets (white arrow heads). LA: left atrium; Ao: aorta; LV: left ventricle. Panel B. Post-mortem image of thrombi on the outflow stent frame of the transcatheter valve (black arrow) of patient 1. Panel C. 2D transesophageal echocardiography of patient 2. This long axis view shows a thrombus (asterix) situated between the first surgical mitral valve (white arrow) and the stent of the THV (yellow arrow). The transcatheter valve leaflets are also thickened (white arrowheads) Panel D. 3D transesophageal echocardiography showing the thrombus from the atrial side in patient 2. The original surgical mitral sewing ring (white arrow) and the transcatheter valve (black arrow) are seen.
Case 2
A 77-year-old lady with a history of CABG and mitral valve replacement for rheumatic mitral stenosis (MS) presented with pulmonary oedema. TTE confirmed severe bioprosthetic mitral regurgitation (MR) and moderate MS (mean gradient of 10mmHg). ATVI was offered due to frailty. Aspirin 81mg was continued while clopidogrel 600 mg was loaded two hours prior to the procedure. Asize 26 mm Edwards SAPIEN valve was deployed transapically. MR was abolished and transmitral gradient fell to 7mmHg. She was discharged on clopidogrel 75 mg and aspirin 81mg daily. Echocardiography for evaluation of dyspnoea a month later showed athrombus attached to the edge of the Edwards SAPIEN valve (Figures 1C and 1D). Anticoagulation was instituted and she was discharged uneventfully.
These cases show that thrombi can develop early after TVI despite dual antiplatelet therapy (DAPT). The experience gathered from surgical bioprosthetic valves show that thromboembolic risks are highest in the first three months following valve implantation1. It is however unclear if this is mirrored in TVI. Whether the current recommendation of DAPT for six months (PARTNER protocol and recommendation for Medtronic Corevalve2 is adequate for all patients remains to be clearly tested.
Conflict of interest statement
Drs. Webb and Cheung are consultants to Edwards Lifesciences. The other authors have no conflict of interest to declare.