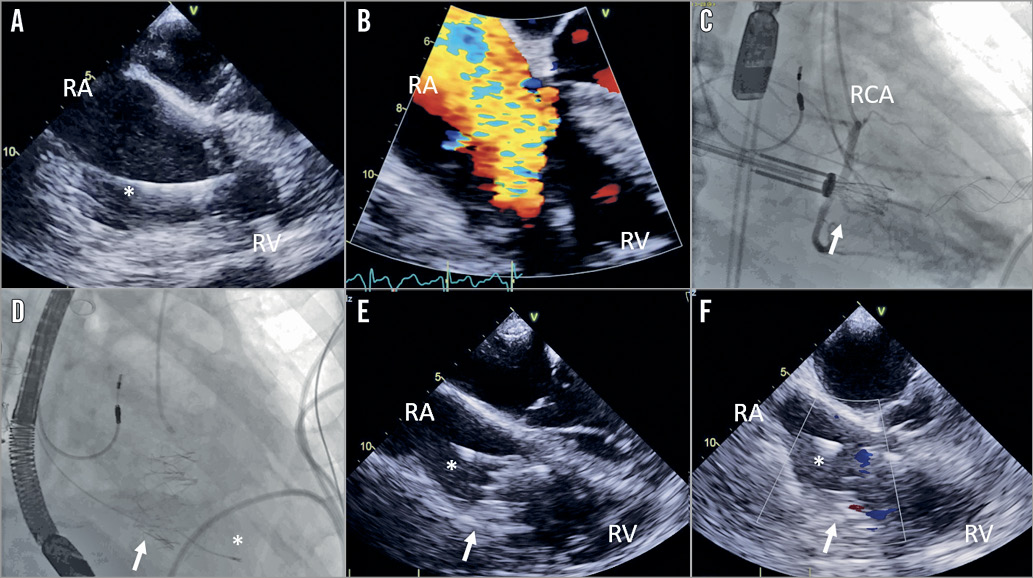
Figure 1. Procedural steps for Gate implantation. A) Transoesophageal (TEE) view demonstrating pacemaker lead and (B) severe tricuspid regurgitation (TR). C) Fluoroscopic positioning and (D) deployment of the Gate valve. E) Post-implantation TEE view demonstrating Gate valve, lead and (F) abolishment of TR. *PPM lead; ➞: Gate valve; RA: right atrium; RCA: right coronary artery; RV: right ventricle
An 82-year-old man presented with severe tricuspid regurgitation (TR) and right heart failure. Despite optimal medical therapy, he remained in NYHA Class III with significant fatigue and oedema. Past history included atrial fibrillation and remote permanent pacemaker (PPM). Transoesophageal echocardiography (TEE) demonstrated a dilated right ventricle (RV) with moderate dysfunction, severe TR with leaflet tethering and a large (15 mm) coaptation gap, and impingement of the posterior tricuspid leaflet by the PPM lead, precluding transcatheter edge-to-edge repair (Figure 1A, Figure 1B, Moving image 1-Moving image 6). Left ventricular function was normal, with no left-sided valve disease or pulmonary hypertension. After Heart Team review, the patient was accepted for transcatheter tricuspid valve replacement.
The Gate™ Tricuspid Valved Stent (NaviGate Cardiac Structures Inc., Lake Forest, CA, USA) is a self-expanding valved stent with equine pericardial leaflets designed to engage the tricuspid annulus with minimal extension into the atrium or ventricle. Atrial winglets and ventricular graspers anchor the bioprosthesis to the tricuspid annulus and leaflets1. A Gate 44 mm valve was implanted via the right atrial approach with mini-thoracotomy under TEE and fluoroscopic guidance (Figure 1C, Figure 1D, Moving image 7, Moving image 8), jailing the PPM lead. TEE demonstrated excellent valve function with only trace paravalvular regurgitation and a mean gradient of 1 mmHg (Figure 1E, Figure 1F, Moving image 9, Moving image 10). PPM interrogation demonstrated stable lead thresholds, with no change in position. At follow-up, the patient was clinically improved with resolution of fatigue and oedema. Repeat echocardiography demonstrated sustained TR reduction, with decreased RV size and normal function.
Transcatheter tricuspid repair is being used with increasing frequency and success in the treatment of severe TR2, including lead-associated TR3. However, in patients with advanced RV remodelling and severe leaflet tethering, large coaptation gaps or PPM lead impingement, transcatheter tricuspid valve replacement may provide a more definitive solution. Further studies will define the efficacy and safety of transcatheter tricuspid valve replacement in patients with severe TR and heart failure.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. TEE apical view of tricuspid valve with lead impinging on posterior leaflet.
Moving image 10. TEE transgastric view with colour Doppler showing trace TR.
Moving image 2. TEE apical view with colour Doppler showing severe TR.
Moving image 3. TEE transgastric view with colour Doppler showing severe TR.
Moving image 4. TEE transgastric view with lead impinging on posterior leaflet.
Moving image 5. 3D TEE view of tricuspid valve and lead position.
Moving image 6. 3D TEE view of lead impinging on posterior leaflet.
Moving image 7. Fluoroscopic positioning of Gate valve.
Moving image 8. Fluoroscopy of deployed Gate valve.
Moving image 9. TEE apical view with colour Doppler showing trace TR.