Recent developments in the emerging field of transcatheter therapies for tricuspid regurgitation (TR) stimulated the field of tricuspid valve (TV) treatments1. Nickenig et al reported the outcomes of 64 high-risk patients with functional TR and right ventricular failure, treated with MitraClip® (Abbott Vascular, Santa Clara, CA, USA)2. Functional improvement (NYHA class) and TR reduction of at least one grade were safely achieved in all patients.
While transthoracic echocardiography (TTE) is used for preoperative diagnosis, intraprocedural guidance is mostly dependent on transoesophageal echocardiography (TEE), which provides high-quality images but requires general anaesthesia. Little is known about using only intracardiac echocardiography (ICE) guidance for TV procedures, although this has been adopted since the very beginning in combination with TTE and TEE3.
A 64-year-old female patient with severe TR was admitted in NYHA Class III, after episodes of decompensated heart failure. She underwent prior mechanical aortic and mitral valve replacement for rheumatic disease and oesophagectomy due to perforation. Baseline echo revealed severe TR (vena contracta [VC] 9 mm, effective regurgitant orifice area [EROA] 0.65 cm2) and right ventricular (RV) dysfunction (tissue Doppler imaging [TDI] S velocity 8 cm/sec) with good left ventricular ejection fraction (LVEF).
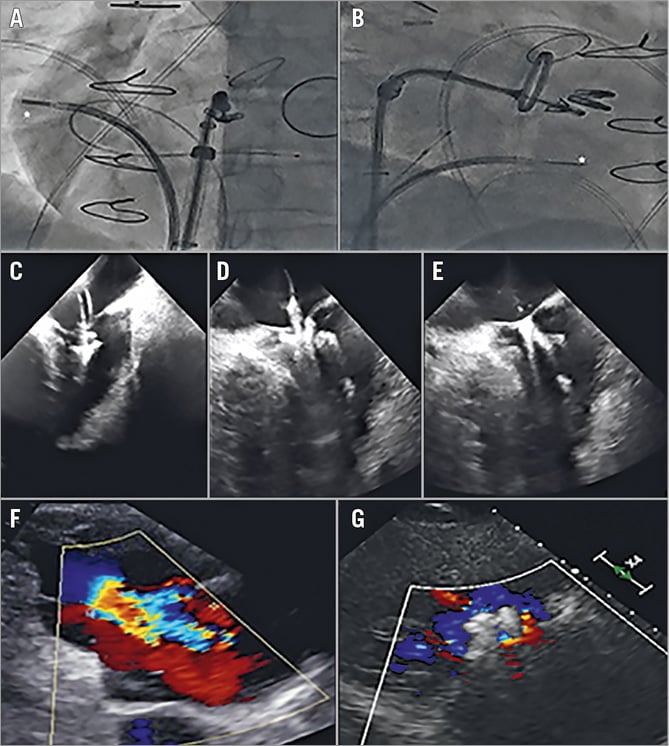
After multidisciplinary Heart Team agreement, the patient was scheduled for transcatheter TV clipping. The TV was approached from the right femoral vein with a MitraClip. A 10 Fr ViewFlex™ Xtra ICE probe (St. Jude Medical, St. Paul, MN, USA), which permits two planes of bidirectional steering in the anterior-posterior and left-right direction, was inserted through the left femoral vein. Manoeuvring the clip in the atrium was facilitated by the presence of the aortic prosthesis (otherwise a pigtail catheter could be positioned in the aorta). While fluoroscopy was used to reach the targeted commissure and to assess whether the ICE probe was orthogonal to the leaflets and to the clip arms (Panel A, Panel B), ICE views ensured clear visualisation of leaflet grasping (Panel C-Panel E). After the first clip, three more clips were positioned sequentially, obliterating the line between the anterior and the septal leaflet. At discharge, moderate residual TR was documented (Panel F, Panel G).
Up to now, the use of TEE has been crucial to guide the TV procedure, although joint agreement on adequate intraoperative nomenclatures should be standardised4. We demonstrated that the TV clipping procedure could be safely guided by ICE under local anaesthesia, with avoidance of orotracheal intubation and of anaesthetic agents for amnesia, analgesia, muscle paralysis and sedation. This would represent the evolution of transcatheter procedures towards more minimal invasiveness, offering benefits to patients. On the other hand, the limited field of view and the need for specific operator skills remain limitations. Further studies comparing the outcomes of ICE guidance vs. guidance by TEE and pure fluoroscopy need to be performed.
Conflict of interest statement
The authors have no conflicts of interest to declare.