Abstract
Aims: This study sought to characterise the real-world performance and clinical outcomes of the PASCAL system, a leaflet approximation device for transcatheter mitral valve repair.
Methods and results: Fifty patients in NYHA Class II-IV despite optimal medical therapy (median age 78.0 years [IQR 74.5-81.0], 52% female, log EuroSCORE 21.6 [IQR 13.2-30.2]) were treated for severe mitral regurgitation (MR) and followed up for one month. Primary and secondary MR was present in 24% and 68% of patients, respectively, with a mixed aetiology observed in 8%. A 1-device strategy was employed in 26/50 patients (52%), a 2-device strategy in 23/50 (46%) patients, and a 3-device strategy in 1/50 (2%) patients. Technical and procedural success was achieved in 100% and 98% of patients, respectively. MR grade ≤1 was observed in 39/50 (78%) patients at discharge, and in 36/46 (78%) patients at one month, with transvalvular gradients remaining ≤5 mmHg in all patients. One device embolisation and one single leaflet device attachment were observed during follow-up. After one month, 73% of patients reported an improvement in NYHA class, and six-minute walk test distance increased by 73±12 m in patients without relevant tricuspid regurgitation.
Conclusions: In a real-world population, the PASCAL device effectively reduces MR and leads to functional improvements on short-term follow-up.
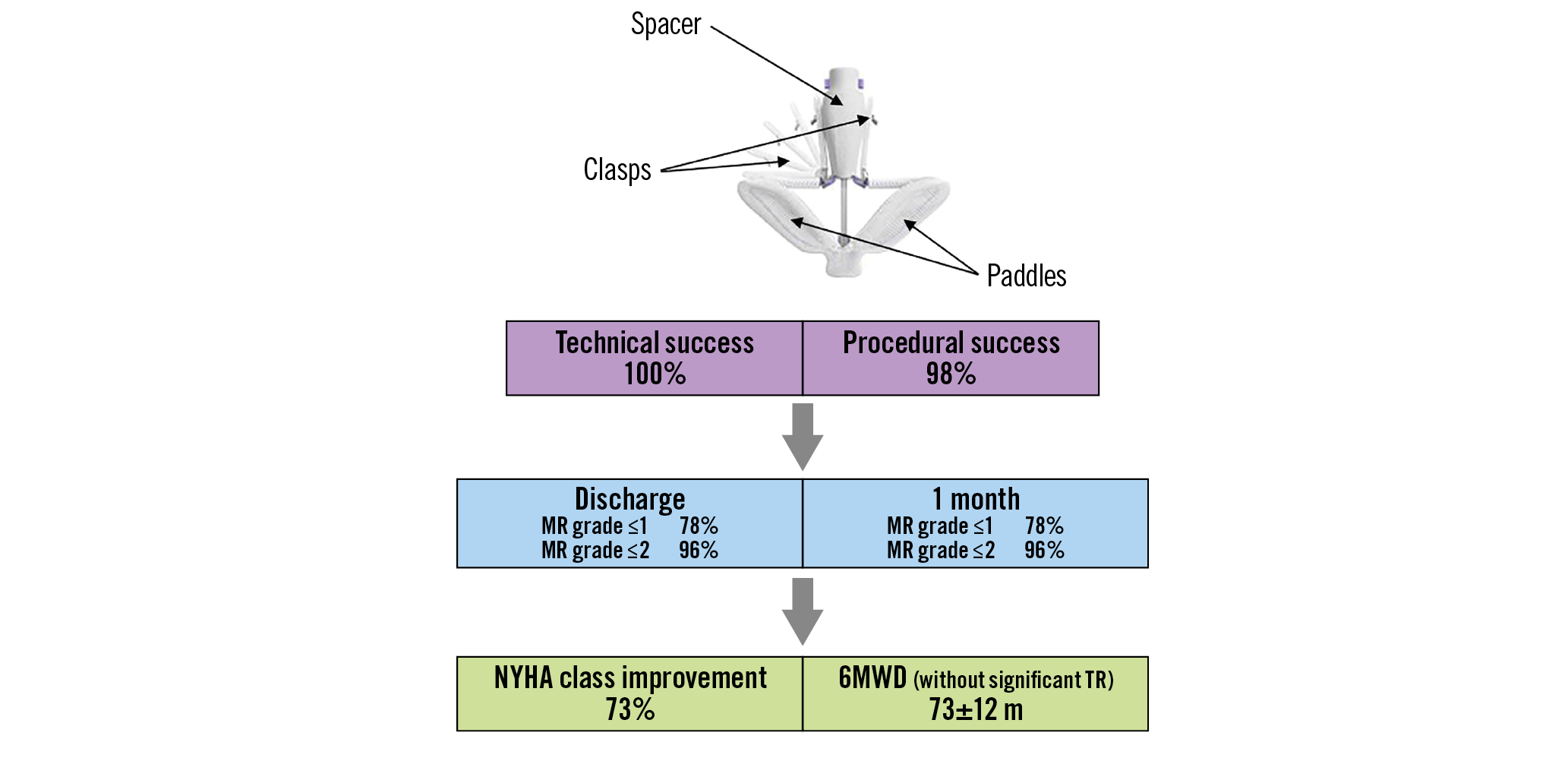
Visual summary. PASCAL system in mitral regurgitation.
Introduction
Mitral regurgitation (MR) is the most frequent heart valve disease in the general population. Recent data suggest that only a minority of affected patients undergoes surgical treatment despite facing poor outcomes1. The most important patient characteristics associated with a decision not to operate included an increased operative risk due to age or comorbidities and impaired left ventricular function2. Randomised controlled trials have suggested transcatheter mitral valve repair (TMVr) with use of the MitraClip® system (Abbott Vascular, Santa Clara, CA, USA) as a safe and durable, but less effective alternative for mitral valve surgery in predominantly primary MR (PMR)3, and as a treatment option to improve prognosis in at least a subset of patients with heart failure and secondary MR (SMR) remaining symptomatic despite the use of maximal doses of guideline-directed medical therapy4.
Nevertheless, TMVr in more complex valve pathologies beyond anatomic criteria tested in clinical trials has resulted in a considerable number of patients who need to undergo reintervention5, or are left with moderate or residual MR conferring worse prognosis6. Recently, the PASCAL Transcatheter Valve Repair System (Edwards Lifesciences, Irvine, CA, USA) has been added to the armamentarium of TMVr therapies and is expected to expand the treatable patient population by offering unique features7,8. Data on the real-world performance of the PASCAL system outside of clinical studies and details on procedural aspects are limited.
Methods
PATIENTS
This analysis with prospectively collected data was conducted in 50 consecutive patients treated with the PASCAL device for moderate-to-severe or severe MR of primary, secondary or mixed aetiology at the Heart Center Leipzig at the University of Leipzig, Germany, between February and November 2019. During the study period, 74 additional patients were treated by TMVr with the MitraClip at our institution. A detailed list of inclusion and exclusion criteria is provided in Supplementary Appendix 1. Concomitant severe tricuspid regurgitation (TR), markedly elevated pulmonary artery pressures, and advanced chronic kidney or pulmonary disease did not serve as exclusion criteria. In addition to transthoracic echocardiography (TTE) and transoesophageal echocardiography (TOE), preprocedural assessment included evaluation of N-terminal prohormone of brain natriuretic peptide (NT-proBNP) levels (Cobas®, Elecsys® NT-proBNP II; Roche, Basel, Switzerland) and a six-minute walk test. All patients gave written informed consent and data analysis was approved by the local ethics committee.
TMVr WITH USE OF THE PASCAL SYSTEM
The technique of TMVr with use of the PASCAL system was carried out as described in detail previously7,8. All procedures were performed under general anaesthesia with interventional guidance by TOE and fluoroscopy. Following access of the right femoral vein and transseptal puncture, the 22 Fr guide sheath of the PASCAL system was positioned in the left atrium. Thereafter, the implant system consisting of a steerable and implant catheter was advanced through the guide sheath, positioned in the target leaflet zone above the mitral valve and appropriately aligned with the mitral annular plane using TOE guidance. Before crossing the mitral valve, paddles of the PASCAL device were opened and a clasp check, i.e., sequential lowering and raising of each clasp to ensure proper functioning, was performed. Leaflets were grasped either simultaneously or independently with sufficient leaflet insertion evaluated by TOE. Implantation of an additional device was considered in case of residual MR and acceptable transvalvular gradients. The definitions of technical and procedural success are provided in Supplementary Appendix 2.
ECHOCARDIOGRAPHIC ASSESSMENT
Echocardiograms were analysed from stored images by an experienced operator in the local echocardiography lab who was unaware of procedural details except for the number of implanted devices. Quantification of MR followed recent recommendations published by the American Society of Echocardiography and included five MR grades: none or trace (0), mild (1+), mild to moderate (2+), moderate to severe (3+), and severe regurgitation (4+)9. Because of limitations of the proximal isovelocity surface area (PISA) method, the current study incorporated the MR regurgitant fraction derived from left ventricular end-diastolic volume, left ventricular end-systolic volume and forward stroke volume (calculated from the left ventricular outflow tract diameter and velocity time integral), as well as improvements in pulmonary vein flow in the integrative approach for MR evaluation after TMVr10.
FOLLOW-UP EXAMINATIONS
Patients were seen for follow-up one month after the procedure. At this follow-up visit, symptoms were recorded, and a physical examination was performed. In addition, patients underwent TTE and TOE, NT-proBNP measurement, and a six-minute walk test.
STATISTICAL ANALYSIS
Normality of data was assessed using Shapiro-Wilk tests. Data for continuous variables are presented as mean±standard deviation, if normally distributed, or as median and interquartile range (IQR) if not normally distributed. Categorical variables are presented as frequencies and percentages. Continuous variables were compared with non-parametric Mann-Whitney U tests. Within-group comparisons were realised with Wilcoxon signed-rank tests. All statistical analyses were performed with SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
BASELINE CHARACTERISTICS
Baseline clinical characteristics of patients included in the present analysis are detailed in Table 1. The median age of the patient sample was 78.0 years (interquartile range [IQR] 74.5-81.0) with 52% of patients being female. Patients were at increased risk for surgery (log EuroSCORE 21.6% [IQR 13.2-30.2]) and highly symptomatic, with 80% of subjects presenting in NYHA functional Class III or IV. Heart failure with reduced ejection fraction (left ventricular ejection fraction [LVEF] <40%) was present in 20/50 (40%) patients. Median NT-proBNP was 2,331 (IQR 944-6,073) pg/ml and renal function in the entire cohort was moderately impaired (mean estimated glomerular filtration rate 51.2±19.7 ml/min/1.73 m² body surface area). Patients were on advanced medical heart failure therapy prior to TMVr (Table 1).
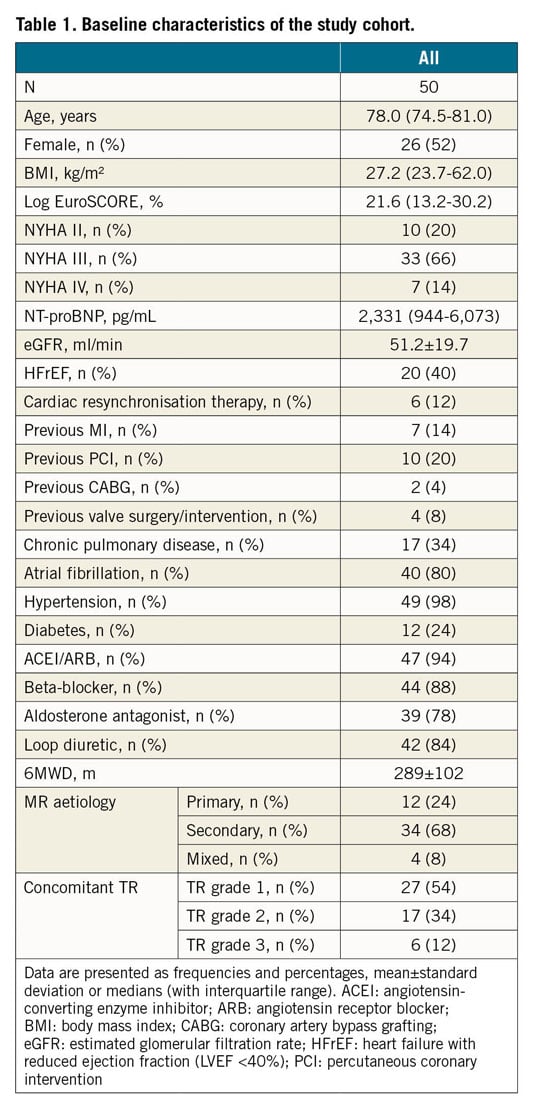
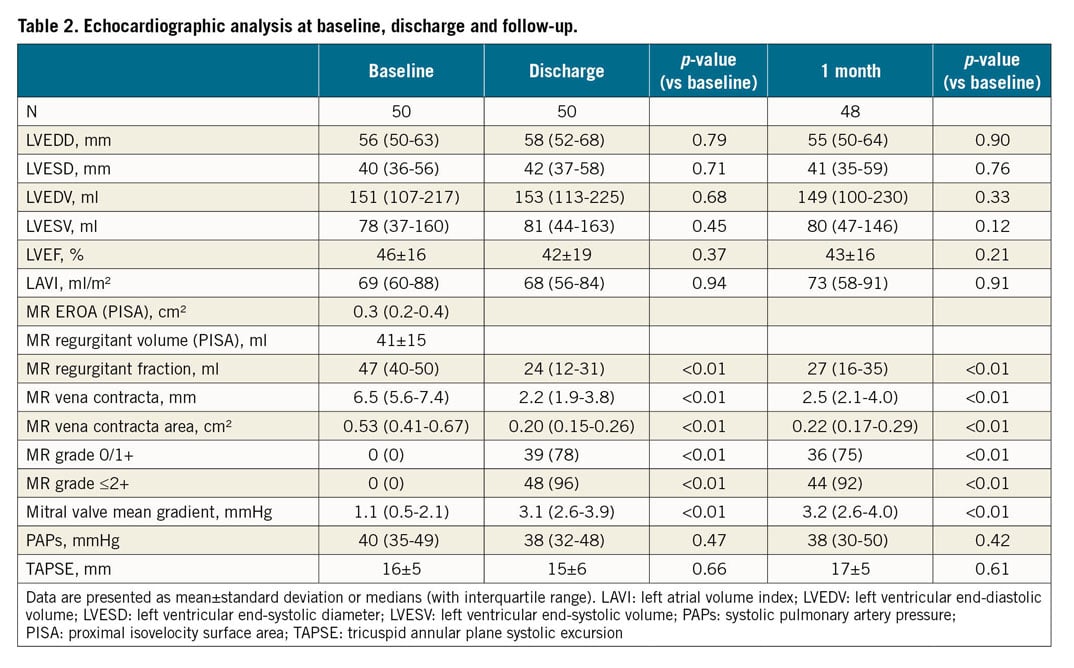
RESULTS OF PREPROCEDURAL ECHOCARDIOGRAPHY
Results of echocardiography are displayed in Table 2. Mean preprocedural LVEF was 46±16%. Patients had dilated left heart chambers with a median left ventricular end-diastolic diameter (LVEDD) of 56 (50-63) mm and a median left atrial volume index (LAVI) of 69 (60-88) ml/m². The most severely dilated left ventricle displayed an LVEDD of 82 mm. PMR and SMR were present in 24% and 68% of patients, respectively, with a mixed aetiology observed in 8% of patients. Three patients had a significant non-central jet close to the posteromedial commissure; a large flail gap >10 mm was evident in three other patients. Preprocedural MR grading on echocardiography revealed a median vena contracta of 6.5 (5.6-7.4) mm, a median vena contracta area of 0.53 (0.41-0.67) cm² and a median regurgitant fraction according to volumetric analysis of 47 (40-50) ml. Based on PISA, the median effective regurgitant orifice area (EROA) and mean regurgitant volume were 0.3 (0.2-0.4) cm² and 41±15 ml, respectively.
PROCEDURAL DETAILS
A total of 75 PASCAL devices were implanted: a 1-device-strategy was employed in 26/50 patients (52%), a 2-device-strategy in 23/50 (46%) patients and a 3-device-strategy in 1/50 (2%) patients. Independent leaflet grasping was performed in 27/50 (54%) patients. In 24/27 patients, independent grasping was applied to improve insertion of the posterior mitral valve leaflet, and in 3/27 patients independent grasping was performed to improve approximation of both leaflets.
Technical success was achieved in 50/50 (100%) patients and final TOE in the operating room demonstrated MR reduction by at least one grade in all patients. Procedural success was achieved in 49/50 (98%) patients, with one patient displaying MR reduction from grade 4+ to grade 3+ on final TOE assessment in the operating room. No acute single leaflet device attachment (SLDA) was observed.
Median duration of the procedure (i.e., time from skin incision to femoral vein access closure) was 64 (51-80) minutes and median fluoroscopy time was 19.8 (14.0-29.8) minutes in the entire patient cohort. Procedure times decreased significantly after the first 15 interventions had been carried out (Figure 1). No difference was observed for the degree of MR reduction when the initial 15 cases were compared to the later cases. In 1/50 (2%) patients, a major bleeding episode occurred during femoral access, which was managed by prolonged compression. No other serious adverse events were observed.
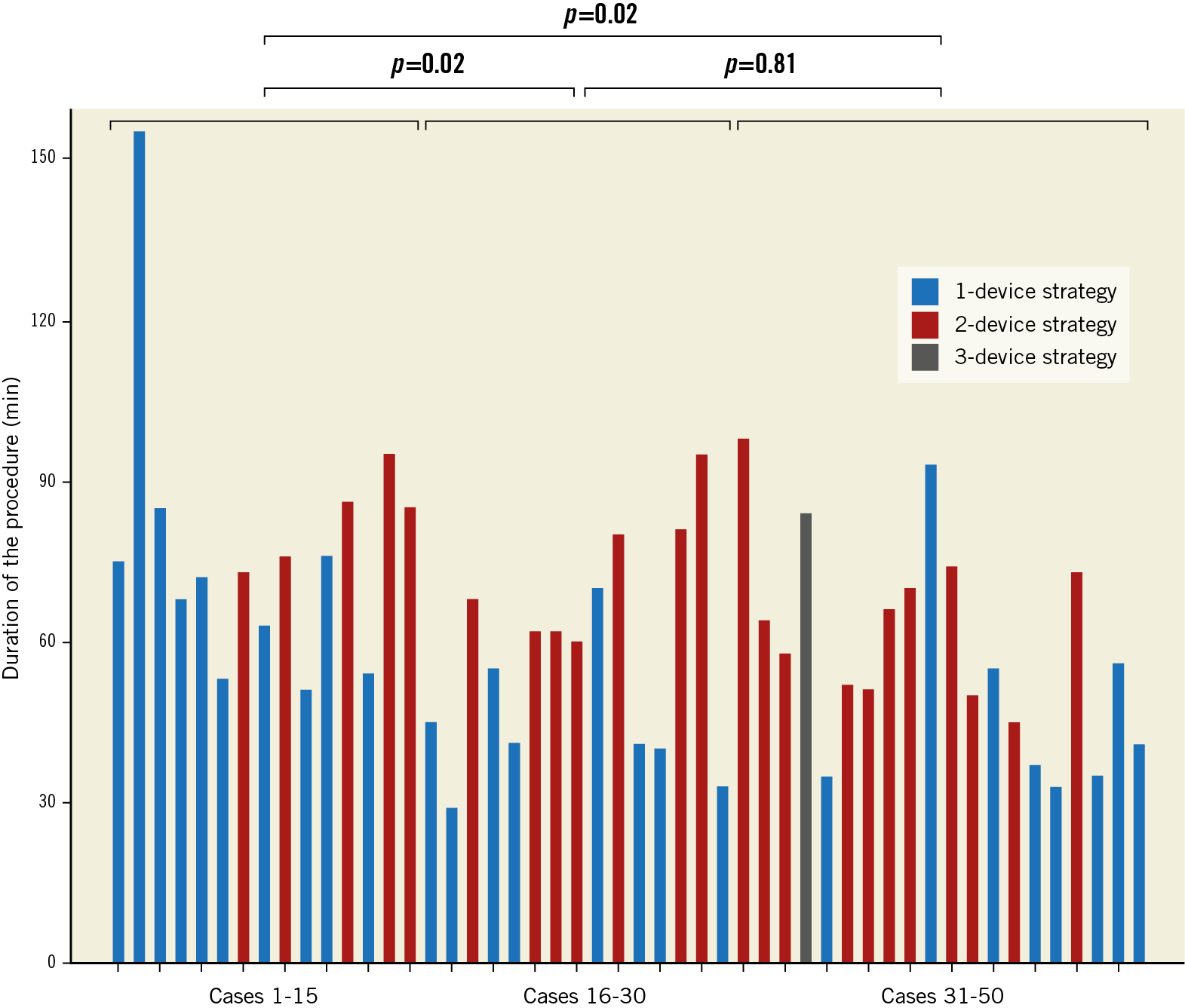
Figure 1. Procedure times of PASCAL procedures 1-50.
CLINICAL AND ECHOCARDIOGRAPHIC FOLLOW-UP
At discharge, MR was reduced to grade ≤2+ in 48/50 (96%) patients and to grade 0/1+ in 39/50 (78%) patients (Figure 2, Table 2). During a mean follow-up of 33±6 days, one 78-year-old patient with dilated cardiomyopathy died from progressive heart failure despite successful MR reduction with a discharge MR grade of 1. No heart failure hospitalisations or adverse events occurred in the remaining patients. One patient refused the outpatient follow-up visit at one month but was alive and reported an improvement in NYHA functional class by one grade when contacted by telephone. In one patient with a severe flail posterior leaflet, implantation of two PASCAL devices using independent grasping resulted in acute MR reduction to grade 1+. Follow-up echocardiography in this patient after one month revealed recurrent severe MR due to embolisation of one PASCAL device to the aortic bifurcation without limitations in iliac flow. Another patient with PMR due to a severe posterior leaflet prolapse who underwent implantation of two PASCAL devices with an acute MR reduction to grade 1+ had a delayed SLDA of one PASCAL device with recurrent MR 3+ on follow-up echocardiography.
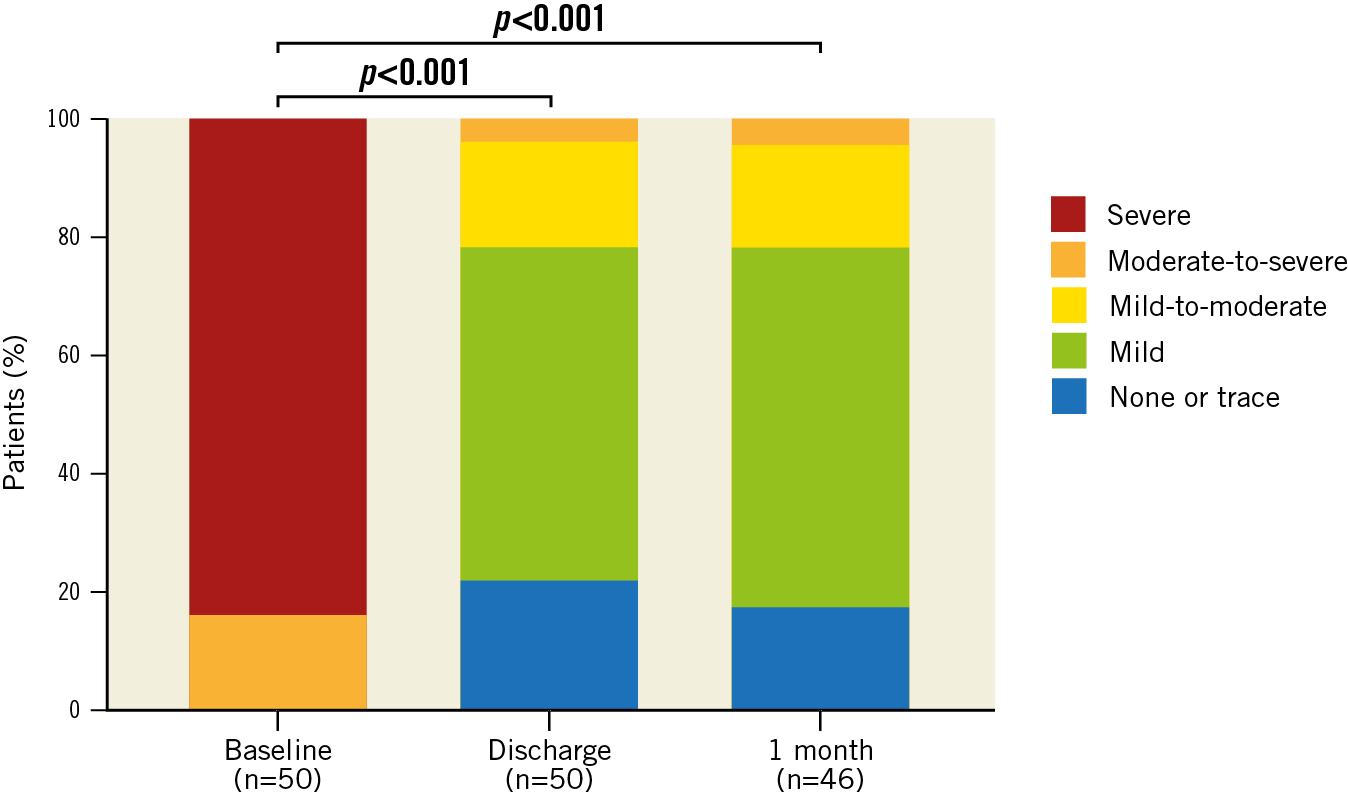
Figure 2. MR grade distribution on echocardiography at baseline, at discharge and after one month following TMVr using the PASCAL system.
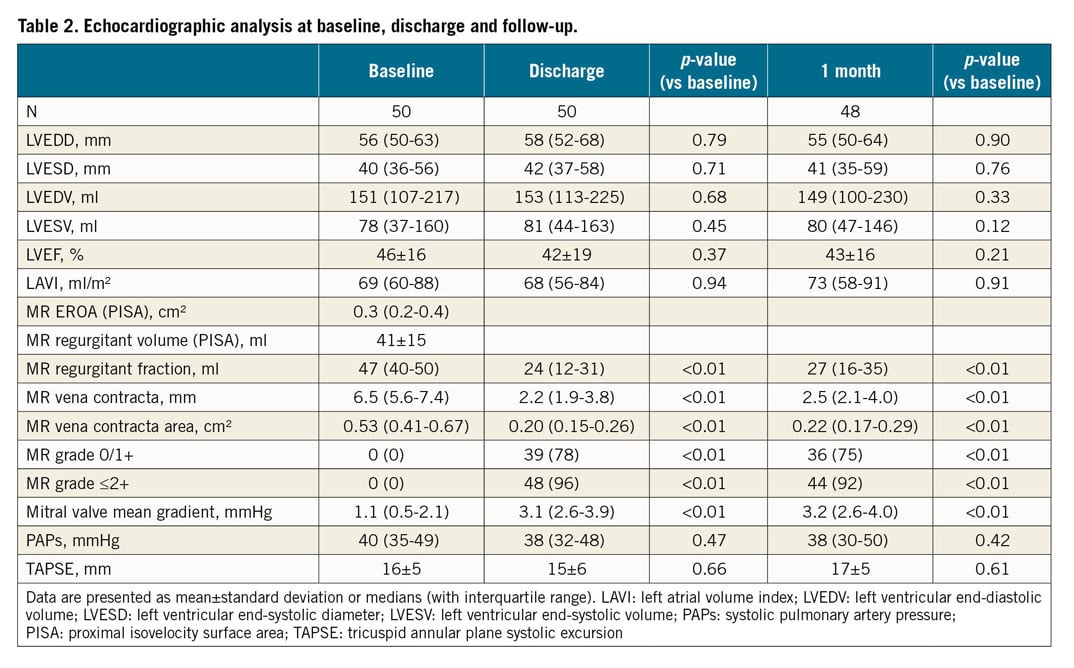
On echocardiography at one-month follow-up in patients with the device in position, an MR reduction to grade ≤2+ was maintained in 44/46 (96%) patients, and 36/46 (78%) patients displayed MR reduction to grade 0/1+ (Figure 2). Results of echocardiographic MR evaluation are displayed in Table 2. The median transvalvular gradient across the mitral valve increased from 1.1 (0.5-2.1) mmHg to 3.2 (2.6-4.0) mmHg but remained ≤5 mmHg in all patients undergoing echocardiography after one month.
EFFECT ON NYHA FUNCTIONAL CLASS, NT-proBNP LEVELS AND 6MWD
After one month of follow-up, 35/48 (73%) patients reported an improvement in NYHA functional class and 37/48 (77%) patients were in NYHA functional Class I or II (Figure 3). The mean six-minute walk distance (6MWD) increased from 291±92 metres to 329±133 metres (p=0.015) (Figure 4A). No significant change in NT-proBNP levels was observed (Figure 4B).
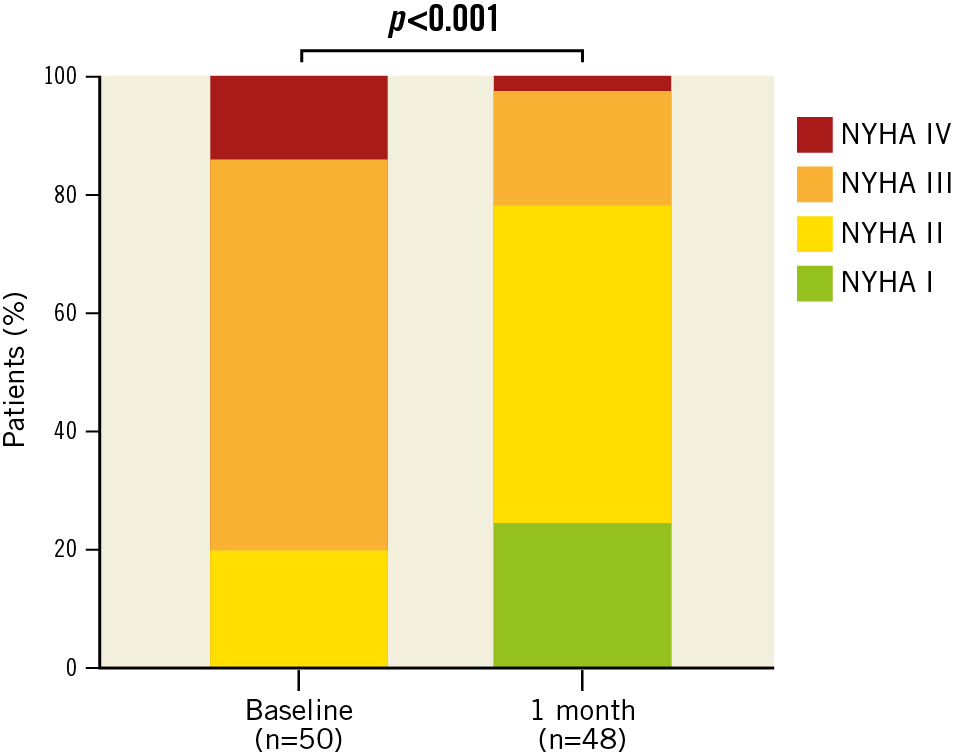
Figure 3. NYHA functional class distribution at baseline and after one month of follow-up in patients undergoing TMVr with the PASCAL system.
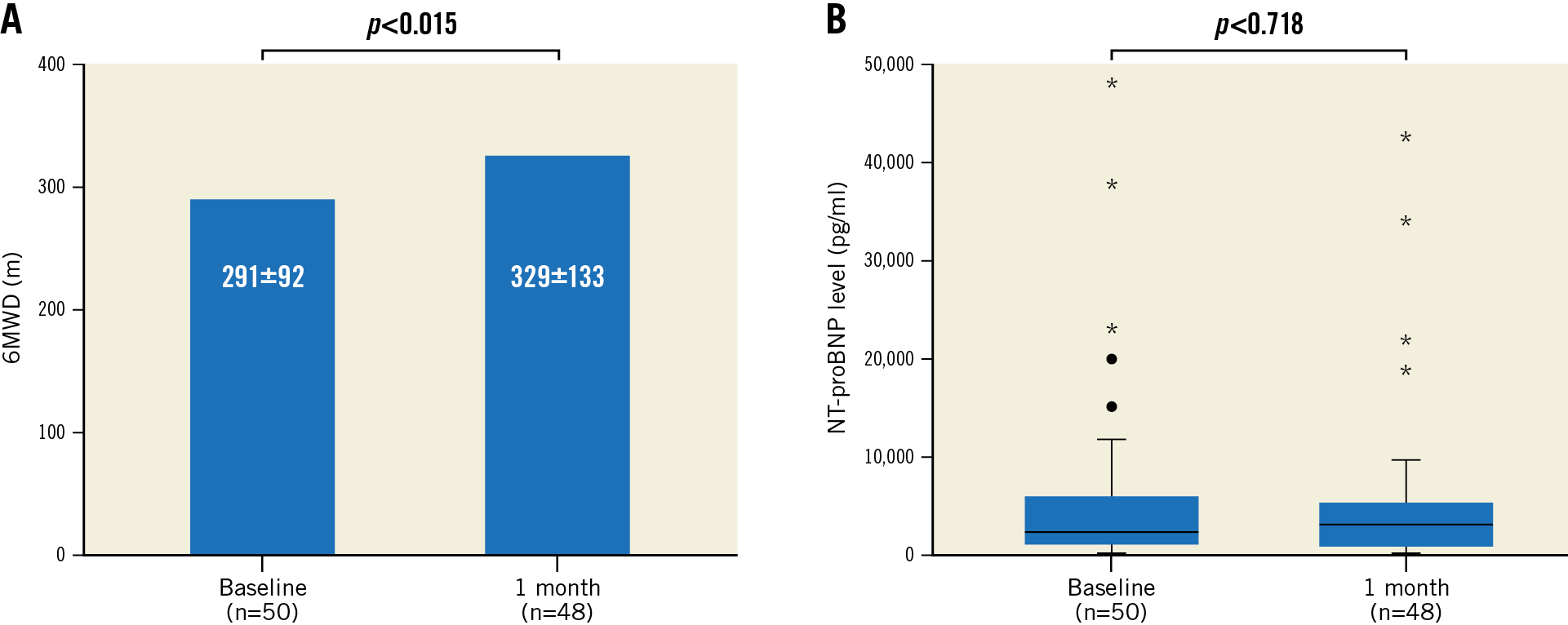
Figure 4. 6MWD (A) and NT-proBNP levels (B) at baseline and after one month of follow-up in patients undergoing TMVr with the PASCAL system.
When patients were grouped according to concomitant TR grade (mild TR: 27/50 [54%] patients, moderate to severe TR: 23/50 [46%] patients), only patients with mild concomitant TR had a significant increase in 6MWD, but not those patients with moderate or severe concomitant TR (320±83 vs 393±95 metres, p=0.002, and 276±93 vs 297±126 metres, p=0.36, respectively). No differences in NYHA functional class improvement or changes in NT-proBNP levels were apparent between patients with mild and moderate or severe TR.
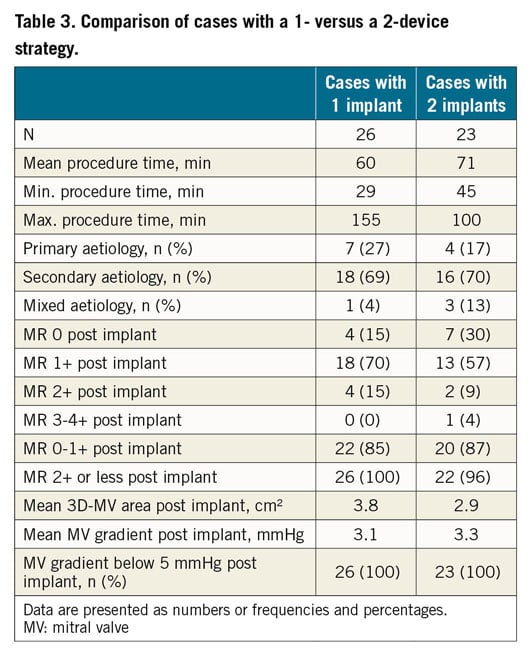
COMPARISON OF 1- AND 2-DEVICE STRATEGY
An overview of procedural details of cases treated by a 1- or 2-device strategy is provided in Table 3. Average procedure times for patients treated by a 1-device strategy and 2-device strategy were 60 and 71 minutes, respectively. Both strategies were applied equally in primary, secondary and mixed aetiologies (Table 3). The degree of MR reduction was comparable between cases treated by a 1- or 2-device strategy at the end of the procedure. Except for one patient treated by a 2-device strategy, MR was reduced to grade 2+ or less in all patients. An MR 0/1+ was apparent in 22/26 (85%) patients treated by a 1-device strategy and in 20/23 (87%) patients treated by a 2-device strategy. On 3D planimetry, average post-procedural mitral valve area was lower in patients treated by a 2-device strategy. Mean transvalvular gradients across the mitral valve were comparable between patients treated by a 1- and 2-device strategy (Table 3).
Discussion
This study, the largest single-centre real-world analysis of TMVr using the PASCAL system, suggests that PMR and SMR can be effectively treated with the device, resulting in clinical and functional improvement after one month of follow-up. Implantation of the PASCAL system demonstrated a high procedural success rate and more than three quarters of patients experienced an acute MR reduction to grade 0/1+, with transvalvular gradients remaining <5 mmHg in all patients. These findings remained stable at follow-up after one month. Two devices were implanted in nearly half of the patients and such a 2-device strategy did not result in relevant increases in transvalvular gradients at discharge or follow-up. Finally, a device-specific learning curve was noticed with a reduction in average procedure times after the first 15 cases had been treated.
Compared to the MitraClip device, the PASCAL system consists of three instead of two catheters to provide a longer working length and increased range of motion. The device itself consists of a central spacer designed to fill the regurgitant orifice area, and the spacer is connected to two paddles and two clasps (Visual summary). When compared to the arms and grippers of the MitraClip, the paddles and clasps are wider in order to maximise leaflet coaptation and to allow load distribution across the surface areas of the inserted leaflets against the spacer11. The convex curvature of the tips of the paddles aims to reduce stress on the valve leaflets. Both clasps can be operated individually to permit independent leaflet capture or fine-tuning of leaflet positioning, if needed.
In line with recent data from a first-in-man compassionate use experience and an early feasibility trial7,8, the present real-world analysis confirms that, irrespective of MR aetiology, an acute reduction of MR can be achieved in nearly all patients undergoing TMVr using the PASCAL device. Procedural success was reported in 22/23 (96%) patients in the compassionate use experience7 and in 56/61 (92%) patients in the CLASP study8. One device embolisation to the aortic bifurcation without flow limitation in the iliac arteries and one delayed SLDA were observed in the present analysis. In both cases, the PASCAL system was used to treat a challenging anatomy with a marked prolapse of the posterior leaflet. Retrospective analysis of procedural and discharge echocardiograms displayed proper grasping of both leaflets. Nevertheless, we cannot exclude that leaflets slipped out of the PASCAL device due to insufficient leaflet insertion, considering the excessive leaflet mobility associated with the huge prolapse in both cases. This underlines the importance of ensuring a maximal grasp length, particularly in complex primary valve pathologies.
We observed a significant decline in procedure times following the first fifteen cases at our centre without a difference in the degree of MR reduction. Overall, procedure times were markedly shorter when compared to centre-specific learning curve analyses for the MitraClip device12. This may be due, at least in part, to the fact that operators in the present analysis were all familiar with TMVr using the MitraClip and were therefore used to basic techniques such as transseptal puncture or acquisition and interpretation of echocardiographic imaging of the mitral valve anatomy.
About half of the patients underwent implantation of more than one PASCAL device in the present analysis, which is comparable to the CLASP study but higher than in the compassionate use experience7,8. A post-procedural increase in transvalvular gradients remains a major concern in TMVr and such an increase may deteriorate long-term outcome13,14. Notably, implantation of more than one PASCAL device did not result in an increase in transvalvular mean gradients >5 mmHg in the present analysis. Future studies are required to investigate whether specific features of this relatively large device preserve leaflet dynamics and how these features impact on valve haemodynamics. Additionally, despite its larger dimensions, the PASCAL device was successfully implanted close to the posteromedial commissure in three patients without affecting the subvalvular apparatus. Although such observations along with specific anatomic criteria making procedural success with the PASCAL system more or less likely have to be tested in larger series, these preliminary data suggest that even non-central jets can be effectively treated with the device.
After one month, 96% of patients with a properly functioning device in position had an MR grade ≤2+, comparable to results of the CLASP study8. Nearly three quarters of patients experienced an improvement in NYHA functional class in the present analysis. Surprisingly, NT-proBNP levels did not change after one month of follow-up, and 6MWD increased on average by 38 metres, which is right at the threshold defined as a clinically significant improvement15. Potential explanations are the limited number of patients treated or the coexistence of other untreated cardiac pathologies in these patients, such as concomitant TR which rarely resolves after TMVr16. Indeed, half of the patients suffered moderate or severe TR with no significant improvement in 6MWD, suggesting that functional improvements mediated by TMVr are probably underestimated in this patient sample.
Limitations
As with previous publications on the PASCAL device, this analysis is limited by the small number of patients and follow-up is confined to one month. Another study reported acute results on 18 patients undergoing TMVr with the PASCAL repair system at three different hospitals17.
Conclusions
TMVr using the PASCAL system showed feasibility and safety in this single-centre real-world analysis, which is the largest so far carried out. The device effectively reduced MR of primary and secondary aetiology and led to improvements in NYHA functional class and 6MWD after one month of follow-up. Considering the complex and heterogeneous alterations of mitral valve anatomy in MR, future studies are needed to address the question as to which TMVr device is best suited to reduce MR in a given anatomical situation.
|
Impact on daily practice Transcatheter treatment of mitral regurgitation (MR) in patients at high surgical risk remains challenging given the complex and heterogeneous alterations of mitral valve anatomy in primary and secondary MR. The PASCAL system is a novel leaflet repair system for transcatheter mitral valve repair, which is differentiated from the MitraClip in several technical aspects. This study reports the largest single-centre real-world analysis of the PASCAL repair system, showing that it safely and effectively reduces primary and secondary MR and leads to functional improvement after one month of follow-up. |
Acknowledgements
The authors thank Margit Büttner and Martin Petzold for excellent technical support in the study organisation.
Conflict of interest statement
P. Lurz is a consultant to Edwards Lifesciences and has received institutional grants from Edwards Lifesciences. M. Borger receives speakers’ honoraria and consulting fees from Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.