The late 20th century has witnessed a dramatic improvement in the management and outcome of patients with cyanotic congenital heart disease, shifting previously fatal conditions into near-normal lifespans with low – albeit highly variable – symptom burden. Constituting the largest entity among this diverse group of congenital heart anomalies, tetralogy of Fallot (TOF) has attained a central focus in the development of surgical techniques to separate pulmonary and systemic circulation while maintaining adequate pulmonary blood flow.
Following the introduction of the palliative systemic-to-pulmonary artery shunt by Blalock and Taussig in 1945 and successful complete surgical repair by Lillehei in 1955, surgery for TOF is now performed during infancy with a mortality rate of less than 2%. Surgical repair involves closure of the ventricular septal defect and relief of the right ventricular outflow tract (RVOT) obstruction, which frequently not only requires resection of infundibular tissue and valvotomy, but also RVOT augmentation with a transannular patch. Although this surgical approach has been highly successful in obtaining physiologic stability in early childhood, a transannular patch leads to free pulmonary regurgitation (PR) and chronic right ventricle (RV) volume overload. Even though free PR was previously considered a benign condition, there is increasing evidence that it is the dominant cause of late mortality and morbidity. The standard treatment of free PR is surgical insertion of a bioprosthetic pulmonary valve, but the optimal timing of intervention is posing a substantial challenge.
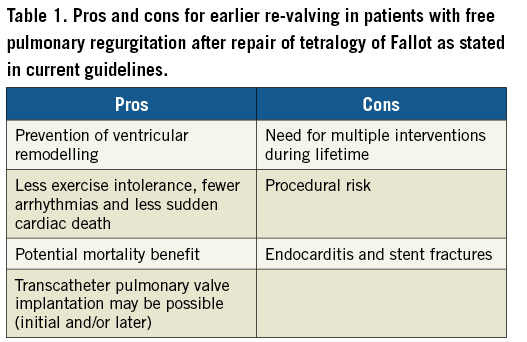
Current guidelines on pulmonary valve replacement (PVR) in patients with repaired TOF and free PR are based on symptoms including clinical arrhythmia, as well as size and function of the RV. The effect of PVR has been debated, but the majority of retrospective studies indicate a benefit in both functional class and arrhythmia burden. However, it is evident that timing of PVR according to the current guidelines means that, in a large proportion of the patients, neither the RV size and function, nor the exercise capacity normalise after re-valving1-3. The suspicion is that too late an intervention will cause fibrosis and irreversible dilatation of the RV. On the other hand, early surgical re-valving implies procedural risk, risk of infectious endocarditis, and the need for more reinterventions for failed bioprostheses (Table 1).
Since surgical PVR carries its own risk that may outweigh the positive effects of protecting the RV from the long-term volume load, it is important to consider alternative approaches. A milestone on this journey was the introduction of balloon-expandable transcatheter pulmonary valve implantation (TPVI) in 2000 by Philipp Bonhoeffer, which aimed to prolong the longevity of degenerated conduits between the right ventricle and the pulmonary arteries4. Today TPVI is a standard treatment in most institutions with an interventional service for congenital heart diseases and, importantly, it has been proven a feasible technique even in native RVOT including patients with free PR after TOF repair using a transannular patch5. Thus, TPVI in native RVOT may not only save the patient with free PR after TOF repair from another open chest procedure, but may also potentially change the threshold for intervention for free PR due to its less invasive nature.
In the current issue of EuroIntervention, new techniques and bioprostheses for TPVI in a broader population of patients are presented. Hascoët and co-authors present a modified technique for insertion of the balloon-expandable SAPIEN transcatheter heart valve (THV) using a long sheath to limit the risk of tricuspid valve injury when advancing the delivery system from the femoral vein to the RVOT6.
Furthermore, a multicentre study presents the experience with TPVI using the latest-generation balloon-expandable SAPIEN 3 THV (Edwards Lifesciences, Irvine, CA, USA) in 82 patients, where the majority had TOF including native RVOT, with good short-term haemodynamic and functional outcomes7.
As mentioned above, much attention is paid to TPVI in native RVOT in order to avoid redo surgery, as well as the potential for earlier re-valving in TOF with free PR due to a lower procedural risk. However, several obstacles for TPVI in native RVOT have been identified including heterogenous anatomy, no or sparse calcification, and the large size of these outflow tracts. One suggestion is to shift from balloon-expandable to self-expanding THV technologies, which may offer better outcomes in the native RVOT. This issue of EuroIntervention presents two studies on TPVI using the self-expanding Venus P-valve® (Venus Medtech, Shanghai, China) in TOF patients repaired using a transannular patch. Zhou and co-authors report on the largest patient cohort treated with self-expanding TPVI so far. The one-year results of Venus P-valve THV in native RVOT in 55 patients at six Chinese centres show promising outcomes despite some learning curve issues8.
Similar findings were reported by Morgan and co-authors in 38 patients treated with the Venus P-valve, although the high rate of frame fractures (27% of the patients) is worrisome9.
However, these two studies are encouraging for expanding TPVI to native RVOT with free PR after TOF repair.
Development of new THV devices and procedural refinements may lead to a paradigm shift in the treatment of patients with free PR after TOF repair. Although earlier surgical re-valving potentially increases the number of interventions during a lifetime, these reinterventions can subsequently often be performed catheter-based. Furthermore, TPVI may even be a less invasive alternative to the initial surgical re-valving in these patients. The consequence may be a shorter duration of volume overload on the RV and a reduction of long-term morbidity and mortality for patients with TOF repaired using a transannular patch.
Conflict of interest statement
L. Søndergaard has received consultant fees and institutional research grants from Edwards Lifesciences and Medtronic. The other authors have no conflicts of interest to declare.