When dissecting the progress of stent development over the past twenty years, one cannot but admire the rate at which stent technology has improved from first-generation bare metal stents (BMS) to current-generation drug-eluting stents (DES)1. The most recent advances, such as stents that promote healing, bioabsorbable scaffolds and stent-free technologies, are definitely exciting from the translational science point of view, with some yet to prove themselves in clinical trials2,3.
The panacea of any stent technology development would be to achieve three aims: 1) minimal in-stent restenosis, 2) zero in-stent thrombosis (whilst requiring as little antiplatelet therapy for as short a duration as possible), and 3) maintenance of normal vessel biology and physiology, whilst inhibiting pathological processes such as excessive neointimal hyperplasia4,5. Despite recent advances, there is only a narrow margin for improvement when using technology based on current paradigms. Thus, “tweaks” in current stent technology are only likely to achieve marginal gains in clinical terms. These benefits would be difficult, if not impossible to detect in clinical trials that are powered beyond “non-inferiority”6.
Therefore, original thinking is required when considering new devices for the treatment of atherosclerosis in general and culprit vessels in acute coronary syndromes in particular. With the complexity of disease increasing and the average age, as well as the comorbidities of patients, becoming higher, the focus on reducing the need for dual antiplatelet therapy is important7. One option would be to explore the biological aspects of endothelial repair mechanisms in stented arteries and try to address the problem using targets to promote endothelial healing rather than targeting platelet inhibition8.
Another option would be to revisit original preconceived ideas, such as the inferiority of classic BMS vs. DES. Thus, one could try to break through the barrier of development in a way that would utilise the advantage of BMS with quicker endothelialisation, whilst tackling the problem of late loss by treating mitigating factors that lead to increased in-stent restenosis, such as inflammation9.
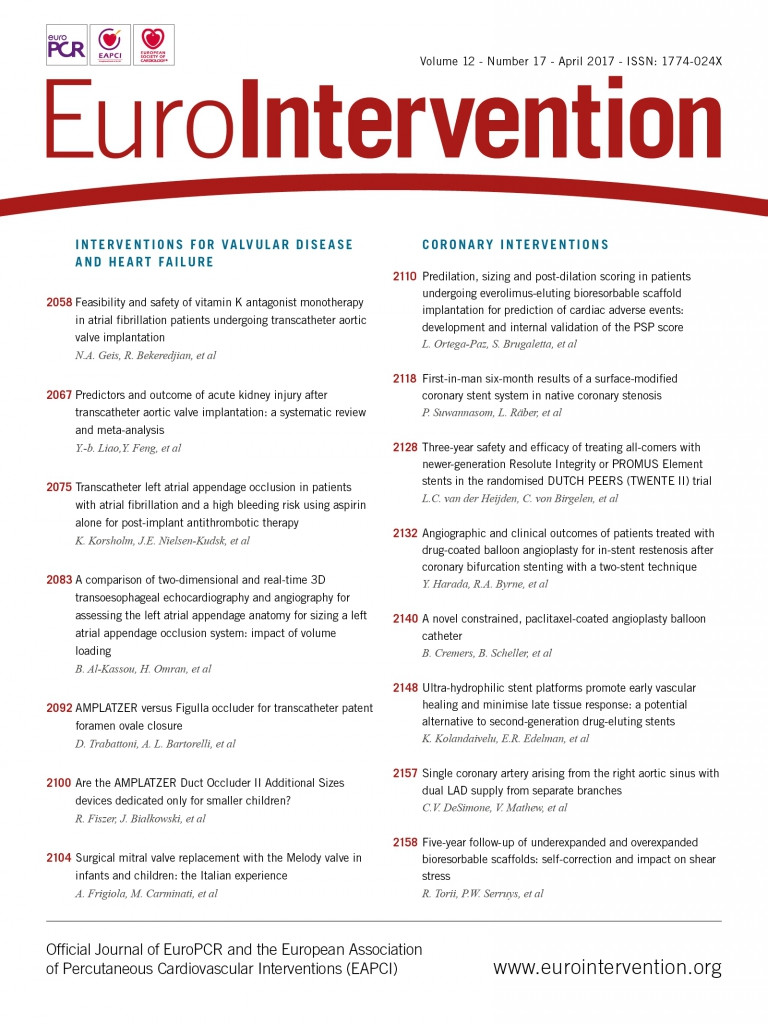
In this issue of EuroIntervention, we present two papers as a transitional pair, namely “Ultra-hydrophilic stent platforms promote early vascular healing and minimise late tissue response: a potential alternative to second-generation drug-eluting stents” from Kolandaivelu et al10, and “First-in-man 6-month results of the Qvanteq surface-modified coronary stent system in native coronary stenosis” by Suwannasom et al11. These two papers will take you through the exciting translational journey the Qvanteq stent underwent from animal studies to first-in-man (FIM).
The stent is designed to explore surface wettability as a favourable modifier of thrombotic and inflammatory pathways, based on encouraging in vitro data suggesting that increased hydrophilicity reduces adhesion and promotes healing. So, we read how a novel ultra-hydrophilic bare metal stent is taken through its paces from the pig and rabbit models to a well-designed FIM study.
The first paper demonstrates that the novel ultra-hydrophilic surface-treated stent with no drug to elute showed promise in the pig (intimal hyperplasia and late thrombosis) and rabbit (early healing and early thrombosis) models. The stent demonstrated superior healing and better neointimal properties than equivalent untreated BMS and DES throughout the study. Importantly, it also demonstrated equivalent endothelialisation to the BMS and less thrombotic risk than DES. Therefore this seemed promising for further study in an FIM experiment.
The FIM study presented here by Suwannasom et al had 31 patients enrolled with follow-up at six months. The design of the study was novel and innovative. The imaging endpoints were based on both quantitative coronary angiography as well as optical coherence tomography (OCT), measured both at baseline and at six months, providing a plethora of stent performance data. The authors also present a device-oriented composite endpoint that provides a solid clinical benchmark for assessing novel stent technologies. Furthermore, the authors relate the FIM study to the animal study by including a strut embedment analysis using specialised software. This quantitative embedment analysis is used as a surrogate marker to evaluate the degree of injury after stent implantation in the atherosclerotic lesion. Therefore, another novelty this study introduces is in using OCT to quantify the degree of injury in vivo and correlating it to neointimal response.
However, the results of the FIM were unexpected and did not correspond to what was found in the animal study. The new stent did not prevent neointimal hyperplasia, with the results indicating that there would be no real substantial reduction in late lumen loss over what is to be expected from current BMS technologies.
In conclusion, a promising preclinical trial did not translate into a superior clinical result in a FIM study. The reasons for this discrepancy when taking the device into atherosclerotic lesions in man from a juvenile porcine or a rabbit model could be multifactorial. One important message to take home is the need for better animal models that reflect the biological environment of an atherosclerotic coronary artery, with all that this entails in terms of a chronic inflammatory milieu. It may be that future technology should be tested on more mature porcine models, and even models that have established atherosclerosis such as the hypercholesterolaemic mini-pig model, in order to approximate the findings to what may be seen in human disease12.
We are very pleased to be able to showcase this example of translational interventional cardiology research in EuroIntervention. We hope that this strategy of combining high-quality research papers into translational duos or even trios will provide encouragement for the research community encompassing scientists, engineers and physicians to be bold and imaginative, and to work closely together in the exciting journeys that take technologies from bench to patient.
Conflict of interest statement
The author has no conflicts of interest to declare.