Abstract
Renal denervation (RDN) as a catheter-based procedure was introduced in 20091. As a reinvention of an old concept2 this approach in treating resistant hypertension has been gathering an unprecedented momentum in the world of hypertension. The incredible success in introducing this technique, followed by its quick and wide distribution, introduced new challenges and requirements for hypertension centres in offering optimal patient care. The challenges of these new parameters and requirements have to be met not only by a multidisciplinary team of doctors who can provide excellent evaluation, treatment and follow-up of these patients, but also by the hypertension centres themselves, who wish to provide this treatment option to their patients.
Introduction
Although the exact prevalence of resistant hypertension in the general population is unknown, this group of patients represents a recurring problem in specialised hypertension centres. In large hypertension trials the percentage of patients presenting with resistant hypertension is as high as 30%3. The official definition of resistant hypertension is somewhat less strict than the inclusion criteria in the large renal denervation Symplicity trials: not achieving the individual blood pressure goal (in general ≤140/90 mmHg; ≤130/80 mmHg in diabetes or renal insufficiency) despite the use of three or more antihypertensive drugs from different classes at full tolerable dosages, one of which is a diuretic4. It has to be emphasised that resistant hypertension is not an immediate indication for renal denervation. Rather renal denervation is a possible treatment option at the end of a thorough patient evaluation.
Since this treatment option has only existed since 2009, there are no studies available which confirm that renal denervation reduces morbidity and mortality. It is feasible that the reduction in systolic blood pressure due to RDN will probably reduce morbidity and mortality in concordance with large pharmaceutical interventional studies, but at present there is no proof of this assumption. In addition, even though the procedure is simple and only a small number of severe procedural side effects have been reported5-7, there are no long-term safety data especially regarding renal artery anatomy and renal function. Regarding the available data, reduction of blood pressure appears to be sustained for a period of at least 24 months7.
These uncertainties are the basis for the restrictive recommendations regarding the application of renal denervation in everyday practice. They demand a sophisticated team and centre infrastructure to ensure diligent and safe patient evaluation and treatment.
This review highlights these challenges and outlines specific requirements for an RDN centre based on national and international recommendations8,9 as well as the experience of our centre.
The RDN team
The RDN team should consist of at least two hypertension specialists, an interventional cardiologist or radiologist and a nephrologist.
The multidisciplinary approach in evaluating patients for renal denervation is emphasised by hypertension experts8,10. A multidisciplinary approach for hypertension control has proven to be successful in daily practice11. There are several reasons for implementing a multidisciplinary team for renal denervation: first, evaluation of patients for secondary causes of hypertension and end-organ damage is time-consuming and usually falls into different specialties. Even though a hypertension specialist should manage the patient, assessment usually has to be done in co-operation with cardiologists, nephrologists and endocrinologists. Secondly, as stated above, resistant hypertension is common if you consider the number of patients with hypertension12. Hence, in theory, there are a substantial number of hypertensive patients who qualify for renal denervation. Since renal denervation is an easy procedure, there are no substantial clinical obstacles in performing it. In order to have the correct indication for renal denervation without treating patients who might not qualify completely or who have not gone through a substantial evaluation, a multidisciplinary approach is advisable. Especially in the context of having little long-term safety data on this procedure with no evidence of reduction in morbidity and mortality, patients for renal denervation have to be carefully selected. A renal denervation team, which considers patients who do not fulfil the inclusion criteria of the Symplicity trials, should only proceed with renal denervation if the patient is included in either a registry or a study.
Eligibility for renal denervation should also be discussed with the RDN team in the context of response rates. The only parameter currently identified which predicts response to renal denervation is blood pressure before renal denervation. The higher the systolic blood pressure before renal denervation, the more likely the response in blood pressure drop six months after the procedure6,7,13. Hence, patients with resistant hypertension only slightly above the blood pressure goal will not respond as well as patients with severe hypertension, not close to the blood pressure goal. This aspect should be considered during patient selection for renal denervation.
The hypertension specialist
A hypertension specialist can be any doctor in internal medicine who is particularly trained to evaluate and treat hypertensive patients. Commonly, this is either a general practitioner or – in special centres – a nephrologist, cardiologist or endocrinologist. National and international societies offer special certified courses for physicians in order to acquire the knowledge and strategy to approach patients with hypertension. For example, the European Society of Hypertension offers a career path to become an ESH hypertension specialist. In addition, centres with special expertise can become ESH Hypertension Excellence Centres.
Even though this is a recommendation, it should be emphasised that evaluation and treatment of hypertension is no trivial task. Especially with resistant hypertension, an expert opinion should always be considered3.
The interventional cardiologist/radiologist
In general, the procedure of renal denervation is simple and safe. If the inclusion criteria of the Symplicity trials and current recommendations are the basis of patient selection, renal artery anatomy and femoral access should not pose any obstacle (Table 1). However, due to the widespread use of the procedure, the easy approach and ongoing studies, more and more patients are being treated who do not present with normal renal artery anatomy, in which the RDN team would still consider renal denervation as a treatment option. Due to the non-existent evidence in these patients, intervention outside of any study or registry is not recommended at all. The interventionalist should have the appropriate material (stents for renal arteries) in stock in order to handle unexpected problems (e.g., dissection of the renal artery).
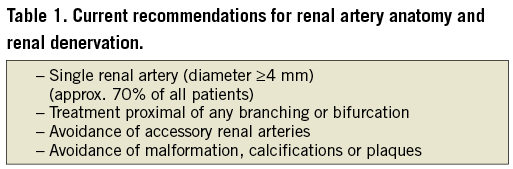
Due to the more complicated anatomy, it is feasible that these patients are at higher risk of complications, such as development of renal artery stenosis or dissection. Especially in the latter case, the physician who performs renal denervation should be well experienced in interventional techniques (PTA and stent implantation) in order to treat these complications instantly. Therefore, it is recommended that the interventional cardiologist/radiologist should perform at least 25 such procedures per year8.
The nephrologist
Since renal denervation as an interventional catheter-based procedure is a relatively young treatment option, it remains unclear whether there are any long-term consequences for kidney function or renal artery anatomy. Even though it appears feasible that this procedure might be beneficial for kidney function, especially in the case of chronic kidney disease, long-term safety of this procedure remains unclear14. Therefore, current recommendations demand a renal evaluation before and a close renal follow-up of the patient after renal denervation9. This includes evaluation of kidney function as well as assessment of renal perfusion in order to exclude development of renal artery stenosis. Even though the incidence of renal artery stenosis is low using the Symplicity uni-electrode device, it might be higher or is at least unknown for multi-electrode devices or other approaches such as ultrasound ablation6,7,13,15. Since patients with high blood pressure are always at risk of developing chronic kidney disease, evaluation by a nephrologist before and after renal denervation should always be performed15. If, in the future, more and more patients with impaired kidney function are considered for renal denervation, this contrast-agent-based procedure certainly requires close monitoring of these patients by a nephrologist11,16.
The RDN centre
As an immediate consequence of the recommendations made in the previous section, the RDN centre should consist of departments which can provide the necessary personnel for the RDN team.
Currently, the distribution of centres performing renal denervation varies dramatically among countries in Europe. In Germany, for example, the availability of the procedure as well as the structural requirements are widespread. In other countries in Europe, only a few centres offer renal denervation. One of the main reasons for these differences is reimbursement of procedural costs. Even though it is assumed that renal denervation is a cost-effective strategy for resistant hypertension, the lack of long-term data and proven cost-effectiveness currently prevents widespread reimbursement by healthcare insurances among European countries17.
Most centres with a focus on hypertensive patients will meet the requirements for renal denervation centres as listed in Table 2. As stated above, careful patient evaluation and selection are crucial to a successful procedure. This requires a proper pre-procedural evaluation with exclusion of secondary causes of hypertension as well as ruling out contraindications for renal denervation. Since all patients should be included in a study or registry, renal denervation centres should be able to provide adequate administrative support in this regard.
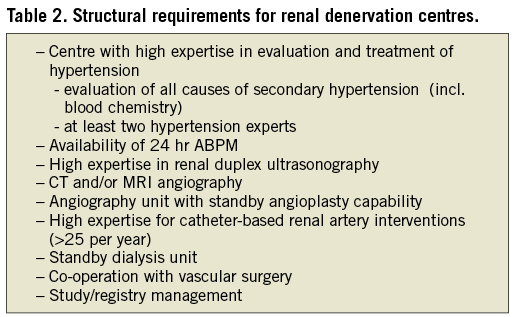
Besides requirements for proper evaluation of hypertension, most structural requirements aim at the management of possible adverse events during or after renal denervation. These events are rare; however, their consequences might be dire. Therefore, a proper evaluation of renal artery anatomy is recommended at least by duplex ultrasound, or alternatively by imaging techniques like CTA or MRA. In addition, in the event of renal artery dissection or bleeding, percutaneous transluminal angioplasty (PTA) standby is mandatory. In severe cases, vascular surgery might be necessary and should therefore be available on site or in a nearby centre. In patients with impaired kidney function, dialysis standby should be available on site or in a nearby centre.
As stated above, even though exact numbers are not available, patients who qualify for renal denervation are numerous. Due to the simple procedure and media coverage, demand is increasing and an increasing number of patients are requesting this procedure. Currently, most centres will recruit most of their patients from their own pool of patients. However, diagnosis, evaluation and treatment of hypertension are commonly a task of the general practitioner and not all patients with resistant hypertension are referred to specialists. In the near future, the number of patients referred for this procedure will certainly increase, when specialists and general practitioners are working closely together. It is unlikely that specialised centres will be able to uphold the strategy of a complete patient evaluation in their own centre as presented in the first part of this section. Reimbursement for such an evaluation is low and it is very time-consuming.
Therefore, the authors of this article would recommend a co-operative approach to this problem (Figure 1).
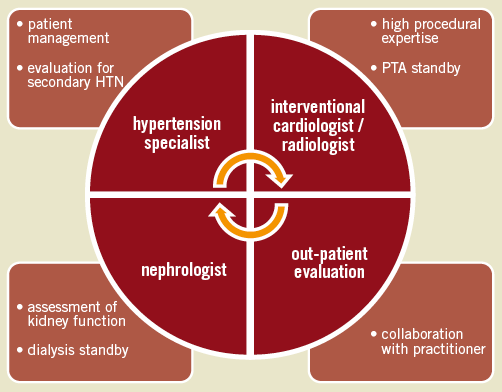
Figure 1. Multidisciplinary approach to RDN.
The RDN centre should establish a close relationship with practitioners in the area. We very much emphasise establishing a minimum evaluation plan for patients who are referred for renal denervation as stated in Table 3. This will dramatically reduce the burden for the specific RDN centre while maintaining a streamlined patient evaluation.
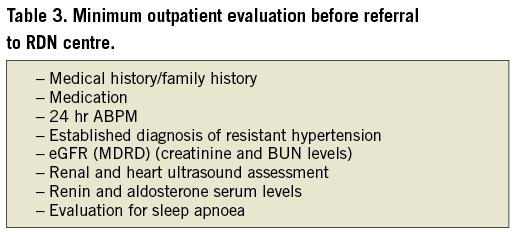
Even though outpatient assessment might differ from in-house standards, pre-selection of patients who approach specialised centres will help to improve optimal patient selection for renal denervation. In addition, inclusion of the practitioner will help to improve the co-operative relationship to the RDN team and will help to spread the knowledge about this procedure.
Patient care strategy
Proper patient care is important for adherence and patient satisfaction. Even though we highly recommend a multidisciplinary approach to RDN in any patient, a single clinic or doctor should be responsible for managing the patient. Regarding the procedural evaluation of patients, we have put together a possible “route to renal denervation” (Figure 2) as well as a detailed assessment plan for patient evaluation (Figure 3).
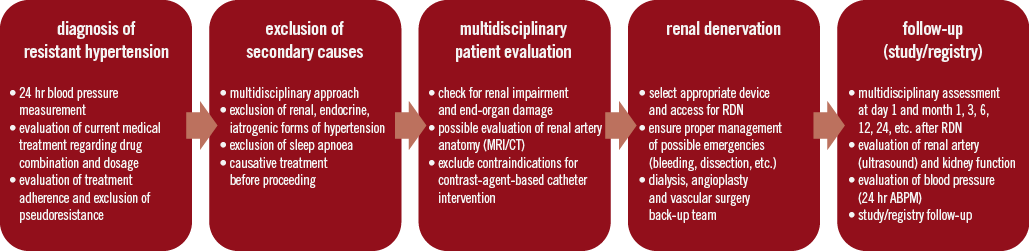
Figure 2. Patient route to renal denervation.
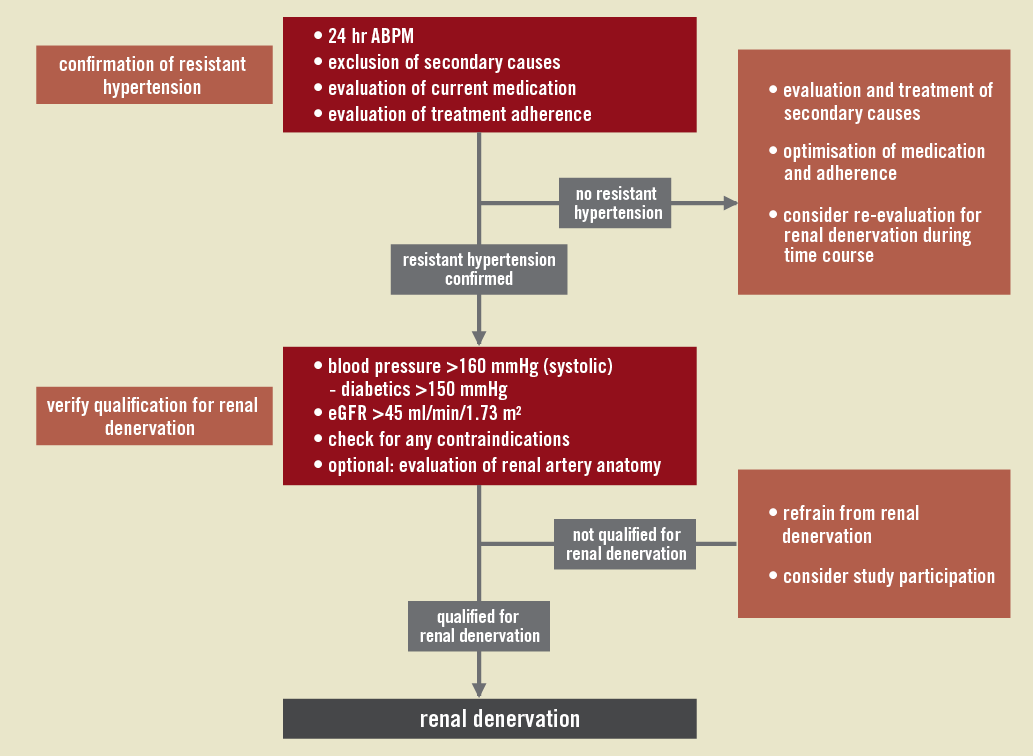
Figure 3. Detailed patient assessment for renal denervation based on current recommendations8,9.
One of the more difficult aspects of patient evaluation with regard to resistant hypertension is checking for proper treatment adherence. Improper treatment adherence can be one of the reasons for uncontrolled hypertension18. The poor adherence to antihypertensive drugs could lead to the diagnosis of resistant hypertension. If this condition is expected, we recommend admission of a patient with controlled application of antihypertensive medication during their stay in order to exclude “pseudo-resistant” hypertension. It is debatable as to whether patients with low treatment adherence should be considered for renal denervation.
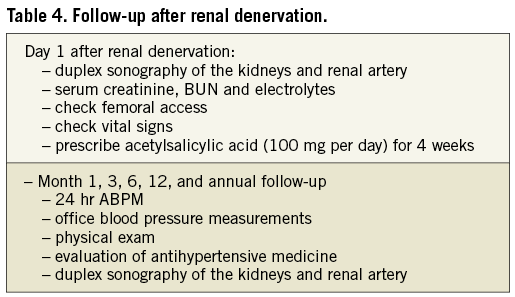
For the RDN procedure, a very short stay in the clinic might be sufficient. However, for some patients, admission one day before the procedure might be worth considering, especially if these patients need special preparation (e.g., i.v. fluids in cases of CKD). Release from hospital one day after renal denervation should provide a proper safety margin in order to detect adverse events regarding kidney function and renal artery anatomy (checking via blood chemistry and duplex sonography).
In order to improve the data on renal denervation with regard to safety as well as morbidity and mortality, it is recommended to include all patients in studies or registries for a scientific follow-up. A possible follow-up schedule is presented in Table 4. Not only does this ensure long-term safety for the patient but it is also a possible tool for quality control within the RDN centre. We therefore recommend that the RDN centre performs all scheduled follow-up appointments in their own RDN patients. Possible adverse events should always be dealt with in a multidisciplinary approach if feasible.
Future outlook
Introduction of renal denervation had a huge impact on the modern approach to resistant hypertension. However, this “young” technique has yet to prove that it reduces morbidity and mortality in treated subjects, as well as being safe in the long run.
As of now, the procedure appears to be safe with a substantial decrease in blood pressure for at least 24 months (and longer).
The technical application of this procedure is easy and time-efficient. Current data imply that severe adverse events are infrequent. Nevertheless, this does not imply that the evaluation of patients for renal denervation is an easy task, or that the procedural approach is easy to realise. It requires the joint expertise of different medical fields in order to have the best possible assessment of each patient. Due to the limited data, safety precautions and recommendations concerning the RDN team and the RDN centre are stringent.
New systems with multi-electrodes will make renal denervation an even easier and more straightforward task. RDN teams and RDN centres should be careful not to give in to the temptation to perform this procedure in every patient who “barely” meets the criteria. Since in most European countries reimbursement for this procedure is not well regulated, widespread use is currently self-limited. Due to increasing evidence on the effectiveness and safety of renal denervation, this is expected to change over time. RDN teams and RDN centres should be well aware of the fact that the future of the procedure will be measured by its success in lowering blood pressure. Currently, the only parameter known to predict response to renal denervation is the level of blood pressure before the procedure. If RDN teams “water down” criteria for renal denervation, there might be a boomerang effect after some time.
There are several feasible indications associated with an overactive sympathetic nervous system, where renal denervation might be beneficial. These are conditions such as arrhythmia, chronic kidney disease, sleep apnoea or even diabetes. However, all available data are only observational14,19-21.
Even if the approach to renal denervation might become more accessible in the future with an increase in indications even outside resistant hypertension, this point has not yet been reached. This greatly supports the current need for a sophisticated RDN team and RDN centres.
Conflict of interest statement
The authors have no conflicts of interest to declare.