Historical overview of preclinical science
Preclinical animal models provide a powerful tool for assessing vascular biology in cardiovascular medicine. In the search for reliable models that mirror the essential vascular effects of local drug delivery concepts, several animal species were evaluated during the past decades. One of the earliest successful models in interventional cardiology – the swine model of coronary artery stenting – has best stood the test of time1. In the era of drug eluting stents (DES), the rabbit iliac artery stenting model became established as a second appropriate model for the study of vascular responses to stent implantation2,3. More recent preclinical studies have again focused on using smaller animal models (rat and mouse) for evaluating stent implants as they provide the opportunity to assess basic molecular mechanisms of stent healing4,5. These models require smaller devices with adapted stent designs, and therefore their translational applicability for the assessment of human device safety is limited. Nevertheless, they may serve as important complementary tools due to the great advantage of utilising genetically engineered strains and the specific insights provided into pathophysiologic mechanisms.
The essential need for preclinical studies in interventional cardiology
The treatment of cardiovascular disease has dramatically changed during the past decades, owing in large part to the development of numerous innovative therapeutic modalities. Nowhere has this been more evident than in interventional cardiology.
With the introduction of percutaneous coronary intervention and stent implantation, a seemingly endless number of devices have been introduced to the European market. While subsets of these devices have been carefully examined before introduction, others remain largely unstudied and potentially harmful to our patients. Alerted by this fact, the clinical, scientific, regulatory and commercial communities are seeking reliable criteria for the evaluation of novel cardiovascular devices. In order to define a secure road map to clinical practice, preclinical research is a prerequisite and a well-appreciated tool in interventional cardiology. Despite this appreciation, there is substantial discordance with respect to the uniformity of preclinical studies in cardiovascular medicine, and as a consequence, preclinical models frequently lack the reliability to appropriately predict the outcome of novel treatment modalities in clinical trials.6
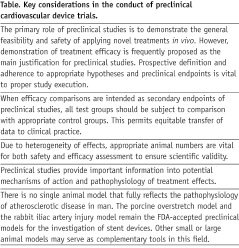
Several key points of preclinical studies should be considered to avoid misleading outcomes and these are displayed in the Table 1.
To improve human health, scientific endeavours and technologies must ultimately be translated to clinical practice. Such translational processes are usually viewed as a two-way street, from “bench-to-bedside” and back. In this regard, translational research is greatly facilitated by a forum that provides researchers and clinicians with necessary information relevant in this field. Innovative integrative journals like EuroIntervention provide a unique medium for researchers, clinicians, regulatory and commercial institutions to present data relevant for the successful implementation of novel diagnostics and therapeutics. In light of the growing need for reliable and sustained innovation in interventional cardiology, EuroIntervention may provide an important collaborative platform in the future, not only for European activities.
Preclinical research in the current issue
In this issue of EuroIntervention, three different preclinical studies are published that share certain similarities, but also differ in terms of the animal model used, preclinical methodology and their impact on clinical practice. While all of these studies provide a significant amount of information to the reader, they also neatly highlight some important issues in relation to the conduct of preclinical research studies.
The study of van Beusekom et al explores the important issue of endothelial regeneration after DES implantation7. Two critical issues are the choice of the model and the time point of assessment. In this respect, the choice of the normolipaemic porcine model is in keeping with current guidelines for preclinical studies3. Nevertheless, we should remember that this pig model displays certain idiosyncrasies when utilised for the assessment of vascular healing after DES – namely pigs display a frequent marked granulomatous response particularly to sirolimus-eluting stent (Cypher) implantation which leads to a more pronounced neointimal formation than that seen in other animals or in humans8,9. This is nicely illustrated in the dataset of van Beusekom et al. Furthermore, as endothelialisation in pig models is rapid, the choice of an early time point of assessment (five days) is pertinent. The authors’ data shows a numerically lower percent endothelialisation with all DES compared with the bare metal control, not statistically significant in the sample size studied. In terms of endothelial function, the suggestion that the paclitaxel-eluting stent (PES; Taxus) has a more pronounced adverse effect is interesting and should be interpreted in light of larger clinical trials10,11. Our interpretation of this very relevant study would differ only slightly from that of the authors, namely, that DES show evidence of impairment in both structural and functional endothelial regeneration, with delay in healing most marked with the PES. This does not detract from the important tenet that structural integrity is no sign of restoration of functional integrity.
Segev et al present interesting data concerning RUS3108, a novel compound which induces perlecan expression12. Perlecan is a large heparin sulphate proteoglycan shown to have inhibitory effects on smooth muscle cell migration and proliferation. In this study, an RUS3108-eluting stent showed promising inhibition of neointimal hyperplasia at 28 days in a normolipaemic rabbit iliac model. While these results are undoubtedly encouraging, we should remember that efficacy endpoints in preclinical stent studies are typically of secondary importance. Indeed, this study highlights the primary function of preclinical trials: the polymer used for RUS3108 loading and elution (PEVA) induced marked arterial wall inflammatory changes. In addition, most cross-sections from RUS3108-eluting stents showed evidence of superimposed intraluminal thrombus. This mandates that alternative approaches to control of RUS3108 release need to be evaluated and tested before this promising technology is ready for translation to clinical studies.
The report of Pendyala et al summarises findings with a novel polymer-free cerivastatin-eluting stent (CES) in a healthy rabbit iliac model13. The favourable efficacy outcomes reported with this device at 28 days are certainly promising. In contrast to the study of Segev et al, safety outcomes (inflammation scores and fibrin deposition) also seemed encouraging – at least in comparison with the Taxus PES. Herein lies the principal failing of this study, i.e., the lack of an appropriate control device (bare metal stent), a scientific imperative where the primary focus is safety and biocompatibility. Accordingly, while the stand-alone data with the CES look good, the reported comparison really only tells us that the novel CES is less toxic to the arterial wall than a stent containing a cytotoxic drug (paclitaxel) and a pro-inflammatory polymer (Translute, SIBBS) – a combination known to be associated with significant vascular toxicity9.
Conclusion
In conclusion, the investigators of all three studies must be commended for undertaking animal studies of innovative cardiovascular devices and functional endothelial integrity. With the aforementioned caveats, the data is a welcome addition to experimental cardiovascular literature. Preclinical studies hold a gate-keeper function with respect to the entrance of novel diagnostic and therapeutic modalities into clinical routine. This underscores the importance of proper animal model investigations in cardiovascular medicine.

