The procedural results of transcatheter aortic valve implantation (TAVI) have continuously improved, paralleling an improvement in available technologies, procedural planning and technical execution. However, some anatomical barriers still remain incompletely resolved, since a proportion of TAVI candidates have advanced atherosclerotic disease associated with complex pathological changes of the arterial tree, leading to difficulties in delivering and implanting a transcatheter heart valve (THV).
Increased angulation or unfolding of the aortic root and ascending aorta, often referred to as a “horizontal aorta”, is one of these anatomical challenges, particularly for the transfemoral approach for TAVI. Defined on either angiography or preprocedural computed tomography (CT), a horizontally oriented aortic root may hamper valve crossing, impair THV delivery, prevent optimal positioning and coaxial alignment of the THV within the aortic annulus, and decrease the overall control on important procedural steps. Consequently, previous reports have documented an association between increasing aortic root angulation and procedural failure using first-generation THV devices1,2,3. In addition, the risk of procedural failure in a horizontal aorta seemed to be confined to the use of self-expanding valves as opposed to balloon-expandable ones2. In cases of horizontal aorta, coaxial alignment may not be perfectly achieved with a long stent frame with a non-steerable delivery catheter as opposed to a short device with a steerable delivery system (such as the SAPIEN 3 valve; Edwards Lifesciences, Irvine, CA, USA). Hence, in patients with a marked horizontal aorta, the SAPIEN 3 device is often preferred by implanting physicians.
In this issue of EuroIntervention, Di Stefano et al revisit the field of aortic root angulation, and provide an analysis on the impact of a horizontal aorta on procedural and early outcomes after transfemoral TAVI using next-generation devices4.
The study is a retrospective analysis of 547 patients undergoing TAVI with a variety of THV devices at a single institution, including balloon-expandable valves in 100 patients (18%), self-expanding valves in 244 (44%), and differential deployment prostheses in 203 (37%). The latter two valve types were pooled in what the authors define as a “non-balloon-expandable” group. A horizontal aorta was defined as an angulation of ≥48° between the horizontal line and the centreline of the ascending aorta on preprocedural CT, and was observed in a surprisingly large number of patients (n=230, 42%).
In the study population, the presence of a horizontal aorta was associated with older age, a higher body mass index, and a higher prevalence of hypertension, atrial fibrillation and cerebrovascular disease. Radiation dose and fluoroscopy time during TAVI were higher in patients with a horizontal aorta, reflecting the related procedural challenges. However, device success according to the Valve Academic Research Consortium (VARC)-2 definition, severity of post-procedural aortic regurgitation, as well as in-hospital and 30-day mortality, were not significantly different among patients with a horizontal aorta and those with a “normal” one. Furthermore, aortic angulation did not affect procedural success and early outcomes for both balloon-expandable and non-balloon-expandable types of next-generation devices. Thus, the study by Di Stefano et al may indicate that a horizontal aorta is no longer a limitation to device success in the contemporary TAVI era using current-generation THVs, and that the anatomy is equally treatable with balloon-expandable and self-expanding devices.
The potential mechanisms underlying the comparable success observed with the newer-generation non-balloon-expandable THVs in this study as well as in daily clinical practice are multifactorial. As discussed by the authors, the improved design of both stent frames and delivery catheters of newer-generation self-expanding devices has allowed more controlled and predictable implantations. The option of recapturing and repositioning – when available – additionally allows precise positioning and adds to procedural safety. Nevertheless, an important aspect that cannot be ignored is the continuous improvement in procedural skills, allowing experienced operators to adjust implantation steps and overcome anatomical hurdles. Particularly in the setting of a horizontal aorta, the choice, position and management of the left ventricular wire is an integral part of a successful procedure. With non-steerable catheters, wire management remains essential for advancing, steering and aligning the THV in the desired position, especially in extremely challenging anatomies (Figure 1).
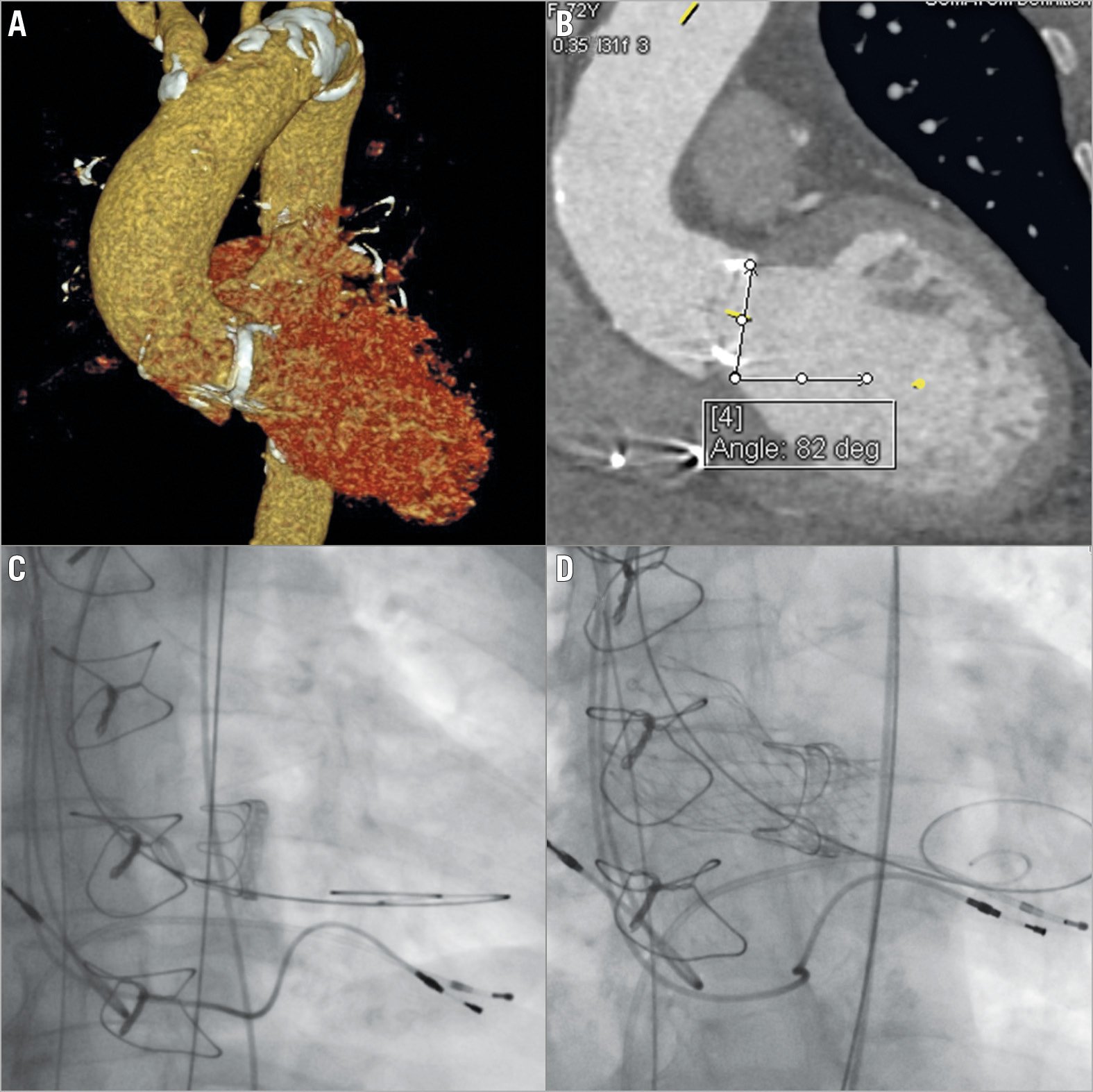
Figure 1. Transcatheter aortic valve implantation using a second-generation self-expanding transcatheter heart valve (Evolut™ R; Medtronic, Minneapolis, MN, USA) for a 72-year-old female with an extremely angulated aortic root and a degenerated surgical bioprosthesis. A) Preprocedural evaluation of reconstructed images using three-dimentional computed tomography. B) Angle measurement revealing an extreme aortic angulation of 82 degrees. C) The guidewire in the left ventricle is adequately filling the apex and is kept “hugging” the outer curve of the ascending aorta following its horizontal orientation to allow co-axial alignment of the long self-expanding device. D) Implanted self-expanding transcatheter heart valve.
Can we now remove the horizontal aorta from the list of challenging TAVI anatomies? The answer is a clear “no”. Despite improvement in technologies and outcomes, advanced operator skills are required in this subset of patients to prevent serious complications. Catastrophic complications such as aortic dissection, annular or aortic rupture were numerically higher in the group with a horizontal aorta in the study by Di Stefano et al, which highlights the importance of careful procedural planning and execution in this subset of patients. Furthermore, the definition of a horizontal aorta used in this report may have been too liberal, which is supported by the fact that almost half of the patients had a horizontal aorta according to the used cut-off. The impact of severe forms of horizontal aorta with extreme angulations (>70 degrees) on clinical outcomes still remains unclear and needs to be investigated, and the influence of other markers of procedural complexity (such as the presence of a bicuspid valve or a surgical bioprosthesis, both excluded from the current study) needs to be evaluated (Figure 1). In addition, the orientation of the THV device in a horizontal anatomy with possible canting and malalignment and its impact on valve function, durability and possibility of redo procedures remain unknown.
Di Stefano et al should be congratulated for adding important information on the relationship between aortic root angulation and transfemoral TAVI with current-generation devices, but – more importantly – for allowing us to rethink our approach and definition of such a complex relationship.
Conflict of interest statement
The authors have no conflicts of interest to declare.