Abstract
Aims: The aim of this study was to evaluate the feasibility, safety and outcomes of TAVI performed via the suprasternal brachiocephalic approach in selected patients at high or prohibitive surgical risk who are not eligible for transfemoral or subclavian TAVI.
Methods and results: From March 2014 to March 2016, 26 high-risk patients without transfemoral or subclavian access options were considered for TAVI via a suprasternal brachiocephalic approach. The feasibility of the suprasternal brachiocephalic approach was determined according to computed tomography findings. In 23 (88.4%) patients the procedure was performed as intended, whereas in three (11.5%) patients the approach was converted to a right carotid access. Both self-expanding (n=20, 76.9%) and balloon-expandable prostheses (n=6, 23.1%) were used. At 30 days, no patient had died; there was one major stroke (3.8%) and there were three major vascular access site-related complications (11.5%). After a median follow-up of 317 days (57-705), two patients had died, both from cardiovascular causes, and 19 out of 24 survivors (79.2%) were in New York Heart Association functional Class I or II.
Conclusions: This single-centre case series suggests that TAVI using the suprasternal brachiocephalic approach is feasible in selected patients and may represent an additional alternative route in patients who are not eligible for other approaches.
Abbreviations
AS: aortic stenosis
BC: brachiocephalic
MSCT: multislice computed tomography
SC: subclavian
TA: transapical
TAo: transaortic
TAVI: transcatheter aortic valve implantation
TC: transcarotid
TF: transfemoral
TTE: transthoracic echocardiography
Introduction
Transcatheter aortic valve implantation (TAVI) has emerged as the reference treatment for patients with severe aortic stenosis (AS) who are inoperable or at high risk for surgery1. Moreover, the recent PARTNER II trial showed results similar to surgical aortic valve replacement in intermediate-risk patients2. The transfemoral (TF) approach is the preferred access route but is not suitable for all patients. In patients with unfavourable femoral access, alternative routes have been described.
The transapical (TA) route was initially the most frequently used alternative route. However, the invasiveness and impaired outcomes of TA-TAVI have led to a progressive reduction in the use of this approach3,4. Second-generation TAVI systems which have become available in the past few years may also have contributed to this result. The subclavian (SC) approach is less invasive but may not be suitable in a proportion of patients due to the small calibre and tortuosity of the left subclavian artery5-7. More recently, the transaortic (TAo) and transcarotid (TC) accesses have been developed8-11. However, the TAo approach still requires a sternotomy or thoracotomy and data on the safety of the TC access remain limited12,13.
The brachiocephalic (BC) artery has two major potential advantages, its large diameter and a short, direct access to the aortic valve. However, data on the feasibility and safety of TAVI through the BC approach using either an upper partial sternotomy or a suprasternal cut-down are very limited14,15. We report our experience of TAVI through the BC approach using a simple suprasternal cut-down without sternotomy.
Methods
POPULATION
Between March 2014 and March 2016, a total of 26 patients at very high or prohibitive surgical risk, with symptomatic severe AS not suitable for TF or SC access and with relative contraindications to the TA route were selected for TAVI through the BC approach. The indication for TAVI and the selection of the route were based on the judgement of a multidisciplinary team including cardiologists, cardiovascular surgeons and anaesthesiologists. All patients provided written informed consent before the procedure. Data were prospectively gathered in a local database. Outcomes were defined according to the Valve Academic Research Consortium-2 (VARC-2) procedural criteria16.
SCREENING
Screening included clinical evaluation, transthoracic echocardiography (TTE), and multislice computed tomography (MSCT) scanning of the entire vascular bed from the aortic root down to the femoral arteries, including the BC and the SC arteries. Standard analysis criteria included: minimal vessel diameters, presence, location and amount of calcification, tortuosity and anatomical variations (Figure 1).

Figure 1. Multislice computed tomography focusing on the ascending aorta and supra-aortic arteries required for the screening of patients considered for TAVI using a BC access. The analysis includes minimal vessel diameters, location and extent of calcification, tortuosity and anatomical variations.
Suitability of the BC using a suprasternal cut-down was defined according to the following MSCT criteria: 1) a minimal luminal diameter >7.0 mm; 2) a high position, at least 10 mm above the upper border of the manubrium; and 3) a distance ≥7.0 cm between the artery entry site and the aortic valve. As the branching pattern of the human aortic arch may show several anatomical variations, the latter were systematically searched for. Patients with a common origin of the BC and left carotid arteries were considered suitable for this approach if the following two conditions were fulfilled: 1) a large BC artery (>10 mm), allowing a non-occlusive cannulation, and 2) a low junction of the left carotid artery, just above the aortic arch (Figure 2). In addition, an evaluation of cerebral arteries by MSCT and Doppler flow study, including carotid arteries and vertebral arteries, was required to exclude significant atherosclerotic disease or anatomical abnormalities and to confirm the permeability of the circle of Willis.

Figure 2. Multislice computed tomography showing a BC artery with a common origin with the left common carotid artery. The large diameter of the BC artery at its origin (>18 mm) and the low position of the left carotid artery allow a BC access.
PROCEDURE
Procedures were performed in the catheterisation laboratory under transoesophageal echocardiography (TEE) guidance by a team composed of two interventional cardiologists, a cardiac surgeon, an echocardiographer, and an anaesthesiologist. For safety reasons and patient comfort, all patients were under general anaesthesia. Aspirin 75 mg was administered the day before the procedure. All patients received weight-adjusted heparin to achieve an activated clotting time of at least 250 seconds throughout the procedure. Cerebral perfusion was continuously monitored using near-infrared spectrometry. No other specific neuroprotection was used.
Operators were positioned on the right side of the patient’s head. BC access was obtained suprasternally through a 4 cm skin incision, medial to the right sternocleidomastoid muscle. BC and the right common carotid artery were exposed by retracting the right sternocleidomastoid muscle laterally. No systematic vessel-clamping test was done, considering that the large diameter of the BC artery allowed non-occlusive cannulation in most cases. A double purse-string CV-4 ePTFE GORE-TEX® suture (W.L. Gore & Associates, Flagstaff, AZ, USA) was placed over the BC artery. Then, a short 6 Fr arterial sheath was inserted through the purse-string suture on a standard 0.035” J wire. Using a 5 Fr Amplatz Left 1 or 2 diagnostic catheter (Cordis, Johnson & Johnson, Miami Lakes, FL, USA), a J pre-shaped stiff wire (Amplatz Super Stiff™ or Safari™; Boston Scientific Corporation, Marlborough, MA, USA) was placed at the apex of the left ventricle after crossing the aortic valve. Then, according to the type of valve used, a 14 Fr or 18 Fr vascular access sheath (Cook Medical, Bloomington, IN, USA) or a 14/16 Fr E-sheath (Edwards Lifesciences, Irvine, CA, USA) was carefully advanced into the ascending aorta with simultaneous pullback of the dilator. After fixation of the sheath to the skin to avoid any displacement, the rest of the procedure was performed as usual, using either the CoreValve System, the CoreValve® Evolut™ R (Medtronic, Minneapolis, MN, USA), or the SAPIEN 3 valve (Edwards Lifesciences). Alignment and fine tuning of the SAPIEN 3 valves was performed in the ascending aorta, just out of the introducer. Rapid ventricular pacing was used in all the patients treated with the SAPIEN 3 valve, but was not systematic in those receiving Medtronic devices. The vertical trajectory of the introducer may cause technical difficulties for valve implantation in patients with a horizontal ascending aorta and a vertical aortic annulus. In these patients, the SAPIEN 3 valve may be preferred to the Evolut R, due to the distal flexion property of its catheter and its ability to centre the valve within the annulus and increase coaxiality (Figure 3).
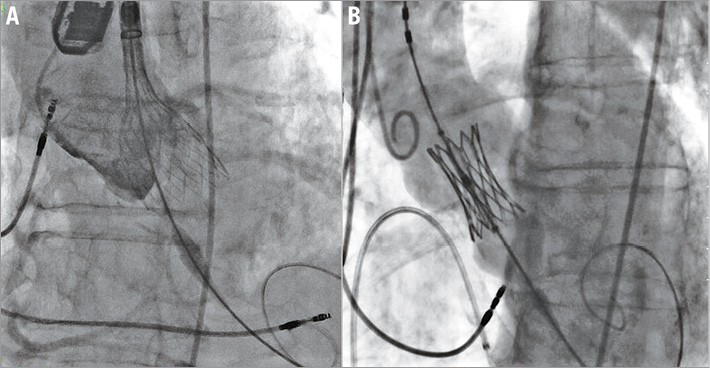
Figure 3. Fluoroscopic images of transcatheter valve implantation through the BC artery. A) Deployment of a CoreValve Evolut R. B) Deployment of a SAPIEN 3.
Angiography was performed to confirm the absence of vascular complications in selected patients.
FOLLOW-UP
Patients were followed up through clinical visits or phone contacts with patients and their cardiologists at one month, one year and yearly thereafter. Outcomes were reported according to the VARC-2 criteria16. All data were prospectively collected from the beginning of patient recruitment.
STATISTICAL ANALYSIS
Quantitative variables were expressed as mean±standard deviation or median (25th-75th percentile) as appropriate. Qualitative variables were expressed as number and percentage.
Results
BASELINE CHARACTERISTICS
Baseline characteristics of the patients are displayed in Table 1. The mean age of the study population was 79±11 years and most patients were women (84%). All patients had symptoms with a New York Heart Association (NYHA) functional Class III or IV. The mean EuroSCORE II was 6.5±5.5% and STS score 6.8±4.9%. The reasons for choosing the BC access are displayed in Table 2. The mean diameter of the BC artery was 12±1 mm. Figure 4 shows the main anatomical relationships between the sternum and the BC artery, as evaluated by MSCT in the study population.
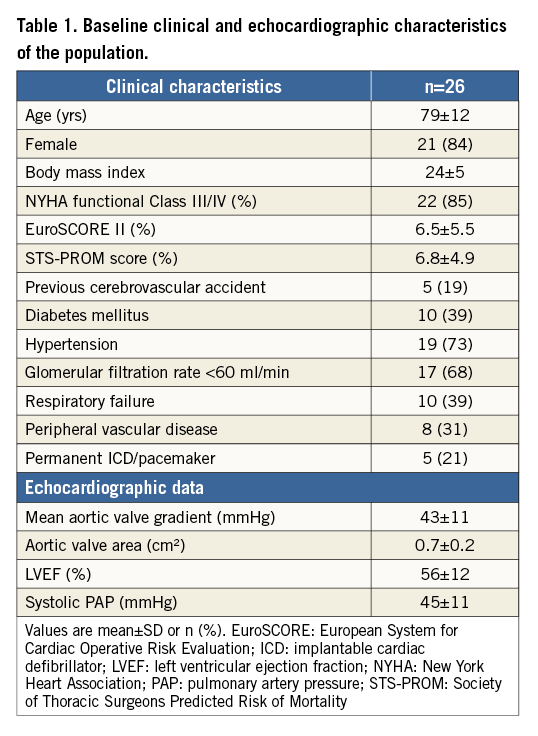
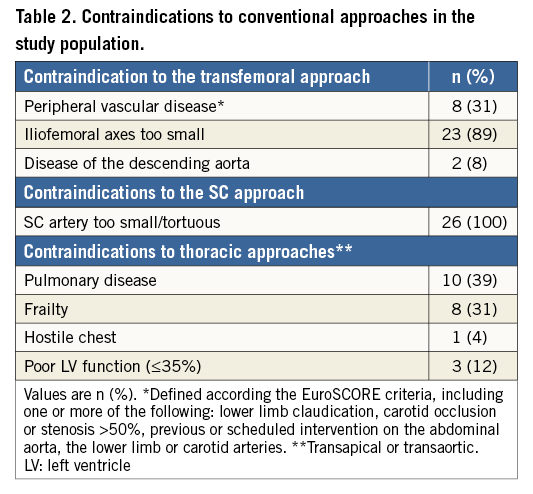
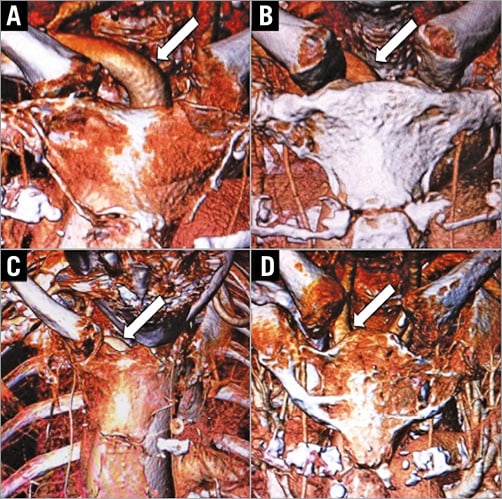
Figure 4. Multislice computed tomography findings in patients considered for TAVI using a suprasternal brachiocephalic approach. The white arrows show the brachiocephalic or the right common carotid artery. A) Ideal anatomy: excellent exposure of the vessel above the sternum. B) Acceptable anatomy: the vessel can easily be accessed via a small suprasternal cut-off. C) Unfavourable anatomy: the vessel is not high enough above the sternum to be easily accessed via a simple suprasternal cut-off. D) Anatomy unfavourable for a suprasternal brachiocephalic access: possible conversion to a right common carotid artery access.
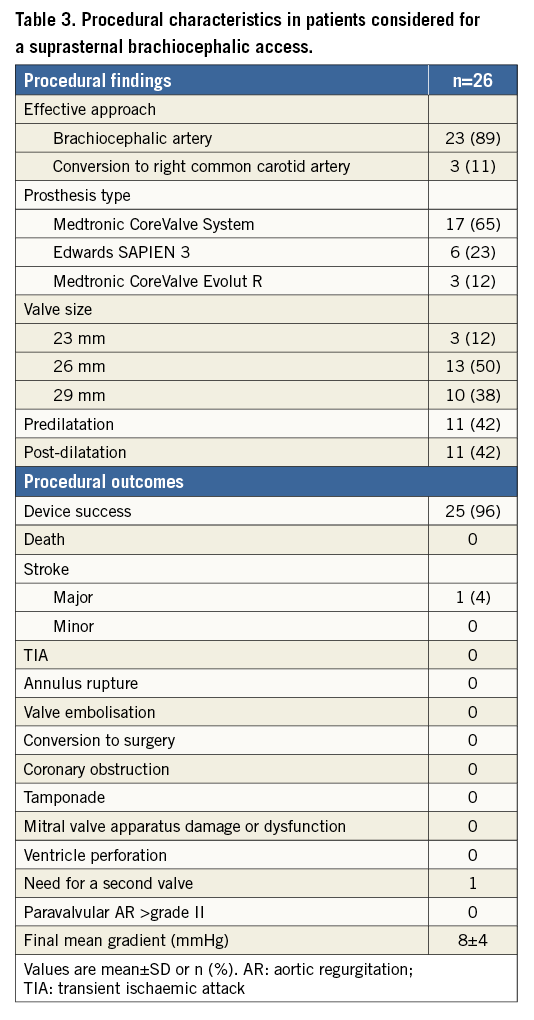
PROCEDURAL DATA
Procedural findings and outcomes are shown in Table 3. The BC artery was easily accessed and the procedure was performed as intended in 22 (85%) patients (Figure 5). In four patients (15%), the BC artery was not accessed because it was located in a position more caudal than anticipated, behind the sternal manubrium. In one of these patients, the BC artery was isolated despite the difficulties, and the procedure was performed as intended. In the other three patients (12%), the surgeon preferred to gain access through the origin of the right common carotid artery, to avoid excessive stretching of the BC artery. Balloon predilatation was performed in 11 patients (42%). The CoreValve System, CoreValve Evolut R and SAPIEN 3 devices were used in 17 (65%), three (12%), and six (23%) patients, respectively. The prosthesis was deployed in the intended position in all patients. Eleven patients (42%) required post-dilation due to paravalvular aortic regurgitation ≥2. One patient required bail-out implantation of a second valve within the first one because of a severe central leak in an Evolut R prosthesis. No patients had more than mild aortic regurgitation at the end of the procedure. Surgical closure was without complication in 25 (96%) patients, including the three patients who underwent TAVI through the right common carotid artery. One patient with the aforementioned difficult access had a dissection and thrombosis of the origin of the right carotid artery requiring thrombectomy and carotid stenting 24 hours after the procedure. Complete atrioventricular block occurred in three patients (12%) and left bundle branch block in two (8%).
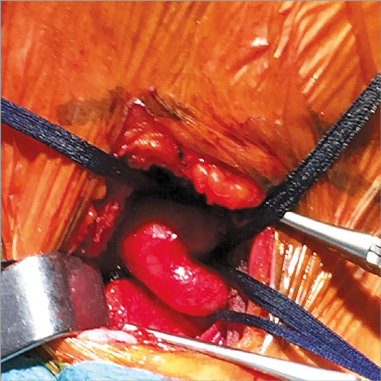
Figure 5. Surgical exposure of the brachiocephalic artery.
30-DAY OUTCOME
Thirty-day outcomes are displayed in Table 4. No patient had died at 30 days. The patient with dissection of the BC artery developed a left-sided hemiparesis with partial clinical recovery. Three patients (12%) had major vascular complications. Two of these patients had a haematoma requiring a simple surgical evacuation with no additional vascular intervention. Major bleeding occurred in two patients (8%). At day four, one patient had a transient ischaemic attack (TIA), with normal brain imaging. Permanent pacemaker implantation was required in four patients (15%). Pre-discharge TTE showed a mean transaortic gradient of 8±4 mmHg, and no patient had more than mild paravalvular aortic regurgitation.
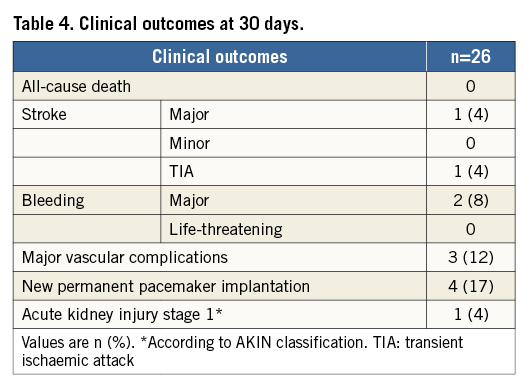
MIDTERM OUTCOMES
At a median follow-up of 317 days (interquartile range 57-705), two patients had died (8%), both from cardiovascular causes. One extremely frail patient with severe immunosuppression, who had a simple procedure and an initially favourable outcome, was readmitted for surgical site infection six weeks after the procedure. In hospital, a sudden rupture of the BC artery occurred, leading to haemorrhagic shock and death despite emergent surgery. Another patient died suddenly after an elective orthopaedic surgery two months after the procedure, probably due to massive pulmonary embolism. No other late complications occurred at the primary access site and no patients had late stroke. At the last follow-up, 19 out of 24 survivors (73%) were in NYHA Class I-II.
Discussion
The present study suggests that the suprasternal access to the BC artery is feasible and may represent an interesting route for TAVI in selected patients with no other alternatives.
Thanks to the continued technological improvements and decrease in introducer size, more than 80% of TAVI procedures are currently being performed through the TF approach and the proportion will increase further in the future. However, the question of the best alternative approach remains a matter of debate for a substantial number of patients with peripheral vascular disease or other contraindications to the TF approach.
Today, these alternatives mainly comprise two thoracic surgical and two peripheral arterial accesses. The thoracic routes, i.e., TA and TAo, share several limitations and potential complications: sternotomy or thoracotomy, post-procedural chest discomfort, pleural effusion and access-site bleeding. While the TA approach is contraindicated in patients with poor left ventricular function and respiratory failure, the TAo approach also has specific limitations in patients with porcelain aorta and coronary artery bypass grafts. Overall, both approaches should be used with caution in frail and elderly patients. A temporal trend has been observed towards lower use of the TA route with a parallel increase of the TAo approach17,18. Nevertheless, a recent meta-analysis showed similar survival rates for TAo and TA TAVI19, and the sternotomy required for TAo access may lead to severe complications, such as infection, in particular when performed in a catheterisation laboratory. The transarterial SC and TC approaches are less invasive and share some advantages with the TF route. General anaesthesia is not mandatory and the cut-down is limited to 3 or 4 cm with a short access to the artery. The left SC route has been used since the beginning of TAVI as an alternative to the TF approach with the CoreValve System and has proven its safety and effectiveness5-7. However, it is rarely suitable in elderly patients with poor femoral access because of frequent tortuosity and small diameter of the SC artery. In addition, its use carries a risk in patients with patent left internal mammary coronary grafts.
More recently, TC access has emerged as a possible option in patients with no other suitable access10. It has been rapidly adopted by some European teams, while many others remain reluctant because of a potential cerebral hazard12. Mylotte and colleagues recently reported their experience on 96 patients with a TC TAVI, with encouraging results: procedural mortality was 3%, 30-day mortality 6% and the stroke rate was 0%13. However, as suggested by the authors, the true rate of neurological events could have been underestimated, since a pre- and post-procedure neurological evaluation was not systematically performed.
These observations highlight the unmet needs which remain in subgroups of patients with no peripheral arterial access and relative or absolute contraindications to thoracic routes. There are several reasons for considering the BC approach as an interesting additional option for these patients. It is a large vessel, most frequently >10 mm in diameter, able to accommodate up to 18 Fr sheaths with no distal flow limitation. Similar to the TC and SC approaches, the BC approach offers a straight and short distance to the aortic valve that allows accurate valve positioning. In addition, it can be used equally with either the SAPIEN XT/3 or the CoreValve and Evolut R prostheses. Access to the BC approach can be obtained through partial upper sternotomy, but also, in a large number of patients, through a small suprasternal cut-off when the artery is located at the level of the upper third of the sternal manubrium, which renders the procedure less invasive and the surgical technique easier.
Data on BC access are limited to the study reported by Philipsen et al, on a series of 20 patients who underwent TAVI with the CoreValve System15. A suprasternal approach was performed in 15 patients and a partial upper sternotomy in five. The 30-day and one-year survival rates were 95% and 75%, respectively. No stroke, vascular or bleeding complications were reported.
Our series is the first reported experience of the BC approach performed exclusively through a simple suprasternal cut-down using three different types of valve prosthesis. It shows that this approach can be carried out effectively and safely in the majority of cases. However, one patient suffered a major stroke directly related to the BC access. In this case, the BC artery was located beyond the sternum, deeper than anticipated on MSCT and closure of the vessel was difficult, creating a flow-limiting dissection at the ostium of the right carotid artery. Of note, this event occurred at the beginning of our first experience with this procedure. This learning curve complication emphasises the mandatory need for an optimal computed tomography screening and a good surgical exposure of the BC artery before carrying out the procedure as intended. If not, another strategy should be adopted, with two possible options: 1) to perform an upper sternotomy and improve the surgical exposure of the BC artery, or 2) to abandon the latter and access higher at the origin of the right common carotid artery, provided an adequate screening has been performed before intervening. The latter option was chosen in three patients, with good immediate procedural results. The delayed septic rupture of the BC artery observed in one of our patients was the consequence of extreme frailty and immunosuppression. Retrospectively, taking into account these severe comorbidities, this patient should probably not have been retained as an acceptable candidate for TAVI (“group C”), whatever the intended approach.
Study limitation
This is a single-centre, observational study on a limited number of patients. It represents an initial experience with an impact of the learning curve on the results. However, the nature of the study guaranteed homogeneous patient selection, procedural technique, post-procedural care and data collection.
Conclusions
Our study suggests that the BC approach without upper sternotomy may represent an interesting additional approach in patients with contraindications to conventional routes to TAVI. It emphasises the need for a careful preprocedural MSCT imaging to discuss the anatomical suitability. In case of unexpected technical difficulties, this approach offers the possibility of a simple conversion towards a right common carotid access. This preliminary experience will require further confirmation in larger cohorts to define its exact place among the various approaches for TAVI in the future.
| Impact on daily practice The question of the best alternative approach for TAVI remains a matter of debate for a substantial number of patients with peripheral vascular disease or other contraindications to the transfemoral approach. The suprasternal brachiocephalic approach is feasible and safe, and avoids the invasiveness of a sternotomy or thoracotomy. Therefore, it may represent an additional alternative approach for TAVI when other vascular access routes are not available. |
Conflict of interest statement
D. Himbert is a proctor for Edwards Lifesciences and Medtronic. A. Vahanian received speaker’s fees from Edwards Lifesciences. The other authors have no conflicts of interest to declare.