Coronary angiography of a patient with non-ST segment elevation acute myocardial infarction, demonstrating an eccentric mid left anterior descending artery lesion (Panel A) associated with a large lipid core plaque by near-infrared spectroscopy (Panel B) and severe luminal stenosis by intravascular ultrasonography (Panel C). The results of near-infrared spectroscopy are presented as a chemogram, where yellow indicates lipid core plaque at longitudinal (x-axis) and rotational (y-axis) locations. After the lesion was stented with a 3.5 x 28 mm everolimus-eluting stent (Panel D), the patient developed slow flow and subsequent NIRS showed that the size of the lipid core had decreased (Panel E). IVUS revealed an intra-stent luminal filling defect suggesting massive plaque prolapse (arrows in Panel F), associated with a strong signal of lipid core by NIRS. Intracoronary nicardipine, and several attempts with aspiration and rheolytic thrombectomy failed to improve the flow and the filling defect persisted. The patient’s troponin T increased from 0.3 ng/mL before stenting to 0.7 ng/mL the day following intervention. The findings strongly suggest that the mechanism for slow flow in this case might have been distal embolisation of the lipidic content of the plaque.
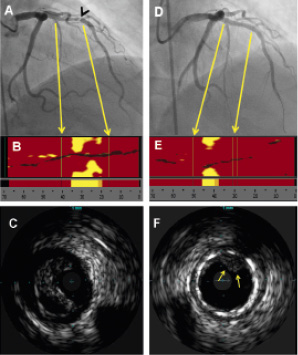
Figure 1. Angiographic, near-infrared spectroscopy, and intravascular ultrasonography images from a patient who developed slow flow during percutaneous coronary intervention.

