Transcatheter aortic valve implantation (TAVI) has revolutionised the treatment of aortic stenosis (AS). It is hoped that the ongoing innovations in TAVI will improve patient outcomes compared with the previous-generation valves as TAVI is extended to patients at low surgical risk.
Since the first aortic transcatheter heart valve (THV) implanted in a human, multiple iterations of the balloon-expandable SAPIEN platform (Edwards Lifesciences) have been developed. The fourth-generation THV using the SAPIEN platform, the SAPIEN 3 Ultra (S3U), achieved the CE (European conformity) mark and U.S. Food and Drug Administration approval. Compared with the SAPIEN 3 (S3), the S3U has a 40% higher sealing skirt in addition to an outer textured polyethylene terephthalate skirt, designed to achieve better sealing. Previous studies reported improvements in paravalvular leak (PVL) rates with the S3U compared with the S3 at short-term 30-day follow-up12.
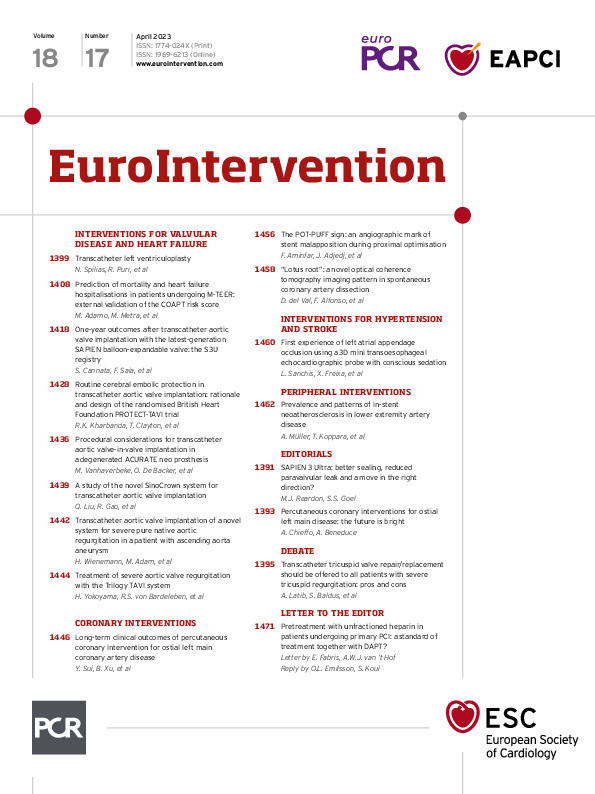
In this issue of EuroIntervention, Cannata and colleagues report the 1-year outcomes after TAVI with the S3U from the S3U registry3. They previously reported in-hospital and 30-day outcomes from the same registry4. The S3U registry is an international, multicentre, physician-led registry of patients undergoing TAVI with the SAPIEN balloon-expandable platform at 12 centres across 4 European countries. Given that the S3U is not made in a 29 mm size, patients undergoing TAVI with a 29 mm SAPIEN 3 were excluded, as were patients undergoing TAVI with alternative access, valve-in-valve TAVI and those with bicuspid AS. A total of 1,692 patients met the study criteria and, using 1:1 propensity matching, 496 matched pairs were compared. Significantly lower rates of mild PVL were seen with the S3U compared with the S3 at 30 days (17.4% vs 27.1%) and were maintained at 1-year follow-up (17.2% vs 29.5%). The rate of no PVL was also significantly more frequent, in favour of the S3U. The rate of moderate or severe PVL was low with both valves and not statistically significant at 30-day or 1-year follow-up. The rates of 1-year all-cause mortality, cardiac death, disabling stroke, permanent pacemaker implantation and hospitalisation for heart failure were comparable between the S3U and the S3.
Most prior comparisons between the S3U and S3 have been limited to in-hospital and 30-day follow-ups and these have consistently shown reduced rates of PVL with the S3U compared with the S3, without significant difference in haemodynamic gradients125. In a recent report by Isogai et al, there was lower prevalence of mild PVL at 1 year with the S3U compared to the S3 (13.7% vs 22.3%; p=0.044); however, the S3U group had a larger increase in the mean gradient from implantation to 1 year (median +4.7 vs +1.6 mmHg; p<0.001)6. The proportion of patients with a mean gradient ≥20 mmHg at 30 days was similar (14.7% vs 13.8%; p=0.87); however, at 1 year this was higher in the S3U group compared to the S3 (23.2% vs 14.6%; p=0.04). It is unclear if the reported increase in gradients is associated with the higher skirt height of the S3U. In the present study, the early mean gradient was slightly higher with the S3U compared to the S3; however, this difference did not persist at 1-year follow-up. While reassuring, this needs replication in other studies with longer follow-up.
Moderate and severe PVL are associated with worse outcomes; however the impact of mild PVL on outcomes has been debated. Emerging data has shown that mild PVL is associated with an increased risk of mortality at 5-year follow-up7. This is particularly important as TAVI is increasingly offered to patients with a longer life expectancy. There are several limitations in the data, including the lack of an independent echocardiography core laboratory, the exclusion of bicuspid valves and larger annuli, and the lack of data on the effective orifice area and the Doppler velocity index. In addition, it is impossible to match for anatomical features that impact PVL as assessed by preprocedural computed tomography in an observational study. Data beyond one year are clearly warranted.
Pending longer-term data, the present study, in conjunction with the existing literature, demonstrates a reduction in mild PVL with the S3U compared to the S3. This iteration of the valve appears to be a move in the right direction for TAVI.
Conflict of interest statement
S.S. Goel is a consultant for Medtronic and W.L. Gore & Associates; and is on the speakers’ bureau for Abbott Structural Heart. M.J. Reardon is a consultant for Medtronic, Abbott, Boston Scientific, and Gore Medical.