Introduction
Social media, in particular Twitter, have radically changed how physicians communicate. Many cardiologists now routinely use Twitter as a rapid vehicle with which to build, share, and consume new educational information about patient care – a phenomenon recently described in the pages of EuroIntervention as Twitterature1. For interventional cardiologists, a popular hashtag used in this capacity is #TAVR – referencing transcatheter aortic valve replacement (TAVR). According to Symplur data, in the first week of June 2020, #TAVR was used 451 times by 295 users with over 1.2 million impressions.
Despite enthusiasm for and the potential value of social media in sharing knowledge, concerns exist regarding selective reporting of experiences within this medium. A bias towards communicating only “ideal” cases in tweets, for example, may imply better-than-expected outcomes for complex procedures like TAVR. Our goal was to characterise the content and outcomes of #TAVR tweets associated with real-world patient cases.
Methods
The Twitter database was searched between June 2019 and May 2020 to identify tweets with patient cases linked to #TAVR and videos (to saturate results with case reports). We then removed retweets, advertisements, published case reports, non-TAVR cases, and cases which described only one part of the TAVR procedure (e.g., access) without valve implant. From the remaining tweets, an interventional cardiologist/fellow abstracted clinical and outcomes data using a standardised case report form. TAVR success was defined as documented implant of a valve in a functional position. Outcomes were reported as “Yes”, “No”, or “Missing” and included death, stroke, myocardial infarction (MI), as well as post-procedural complications. If conflicting data were present between what was reported by the author and what was seen directly in the videos, we recorded outcomes from the author’s perspective rather than an interpretation of angiograms or haemodynamics. We also noted whether the tweet was posted with patient permission. This study used publicly available data and was exempt from human subjects protection review.
Results
Over the 12-month period, there were 499 #TAVR tweets with videos, including 170 unique cases from 83 users. There was a 100% success rate with no deaths or strokes reported. There was substantial missing data. One MI and three vascular complications were reported. No permanent pacemaker (PPM) implant or paravalvular leak (PVL) worse than mild was reported. Assuming missing data would be interpreted by the reader as not occurring, overall rates of outcomes were much lower than reported in clinical trials or registries2,3,4: death 0%, stroke 0%, MI 0.6%, PPM 0%, PVL 0%, vascular complications 1.8% (Figure 1). Non-femoral access was used in 6 (3.5%) patients. Cases were posted with explicit patient permission in 2 (1.2%) cases.
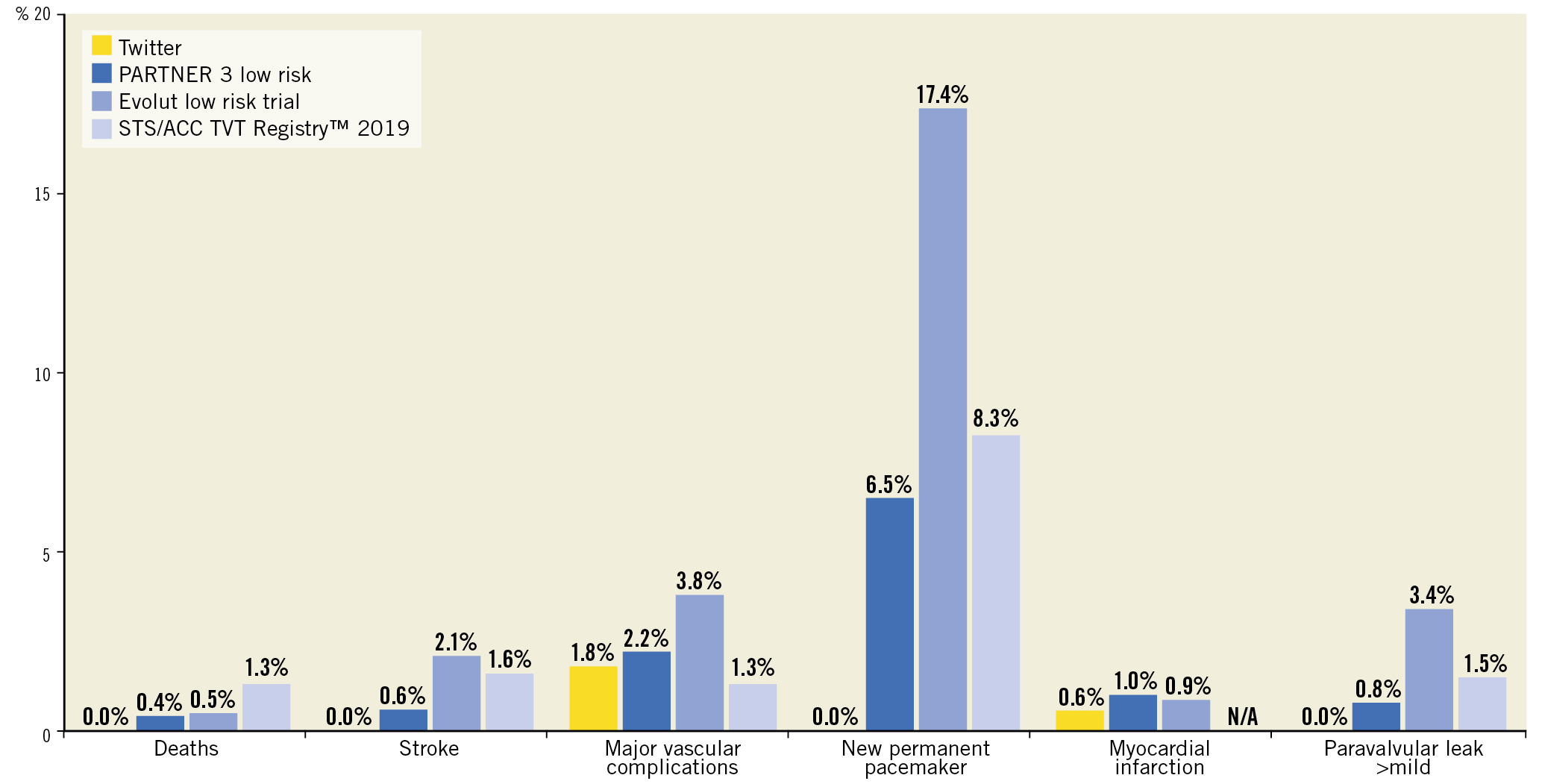
Figure 1. Comparison of transcatheter aortic valve replacement outcomes reported on Twitter with contemporary clinical trial and registry data.
Discussion
Most users are aware of the downside of social media. Instagram, for example, may provide a platform for artistic expression, but use has been associated with anxiety, depression, and “fear of missing out” (FOMO) due to distortion of reality by selectively highlighting life successes over failures. Awareness of the pitfalls of social media is increasing in the general public. Physicians too must be vigilant to prevent our practice from being unduly influenced by our social media experience and suffering interventional FOMO. Despite growth in users of social media platforms across areas of medicine such as interventional cardiology, there has been little written on, or formal scrutiny of, educational content in these settings5.
In the present study, we attempted to fill this important gap in knowledge. During a one-year period, we found that outcomes reported for cases under #TAVR on Twitter were universally successful with few complications when compared with results from contemporary randomised trials and registries. This suggests strong selection bias in both the types of cases being reported and also their outcomes. This finding underscores the importance of registry data and institutional quality reviews to counterbalance the Pollyanna-ish view we may develop from social media. Avoiding overoptimism in Twitter users may be especially true for new or high-risk treatments such as TAVR, where innovation occurs regularly and evolving practices may proliferate.
Patient privacy has also often been overlooked with cases posted on Twitter. Even if de-identified in the traditional sense, other content such as procedural date or its unique features may result in patient awareness of the posting of their procedure. Our finding that few cases were posted with patient permission is worrisome.
Limitations
We only examined a single hashtag for a single procedure over one year. Whether our findings are consistent for other circumstances is uncertain. We also only examined Twitter, which encourages abbreviated posts. While other social media platforms do exist, Twitter has become a critical vehicle for sharing medical information. Finally, Twitter outcomes had no specified time interval (e.g., 30 days), limiting precise comparison to clinical trial or registry data.
Conclusion
Twitter is changing how we interact as a medical community including interventional cardiology. The stakes are high in these open forum conversations regarding potentially life-altering interventions. We must commit to using Twitter wisely.
Conflict of interest statement
N.R. Sutton has received speaking honoraria from Zoll and is the recipient of research grants from the National Institute on Aging and the American Heart Association. B.K. Nallamothu is a principal investigator or co-investigator on research grants from the NIH, VA HSR&D, the American Heart Association, and Apple, Inc. He also receives compensation as Editor-in-Chief of Circulation: Cardiovascular Quality & Outcomes, a journal of the American Heart Association. Finally, he is a co-inventor on U.S. Utility Patent Number US15/356,012 (US20170148158A1) entitled “Automated Analysis of Vasculature in Coronary Angiograms” that uses software technology with signal processing and machine learning to automate the reading of coronary angiograms, held by the University of Michigan. The patent is licensed to AngioInsight, Inc., in which B.K. Nallamothu holds ownership shares and receives consultancy fees. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.