Abstract
Aims: Contemporary coronary chronic total occlusion (CTO) PCI has been associated with increased success rates. However, the rate of periprocedural complications for hybrid CTO PCI remains incompletely defined. We leveraged the OPEN CTO study in order to describe the prevalence, predictors, and health status outcomes of complications during contemporary CTO PCI.
Methods and results: Baseline demographics, procedural characteristics and rates of in-hospital complications were prospectively collected for 1,000 consecutive procedures at 12 expert US centres from 02/2014 to 07/2015. Multivariable logistic regression was used to evaluate the association of pre-specified anatomic and physiologic variables with complications. Patient-reported health status measures over the year following CTO PCI were also compared between those with and those without periprocedural complications. The overall complication rate was 9.7% (n=97/1,000). The most common adverse events were perforation (8.8%), periprocedural myocardial infarction (2.6%), arrhythmia requiring treatment (1.2%), cardiogenic shock (1.1%), and in-hospital death (0.9%). Independent predictors of complications during CTO PCI were: use of the retrograde approach (OR 1.98, 95% CI: 1.32-2.99), age (OR 1.30, 95% CI: 1.07-1.58 per 10-year increment), and J-CTO score (OR 1.20, 95% CI: 1.03-1.41 per one point increment). Mean health status scores over 12 months were worse for patients who experienced complications compared to those who did not, even after adjusting for baseline health status.
Conclusions: Complication rates for CTO PCI are more frequent than those reported for non-CTO PCI and were independently associated with retrograde approach, increasing age, and increasing lesion complexity. In addition, these periprocedural complications were also associated with worse long-term health status outcomes.
Abbreviations
BMI: body mass index
CTO: chronic total occlusions
DF: degrees of freedom
J-CTO: Japanese chronic total occlusion
MI: myocardial infarction
OPEN CTO: Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures
PCI: percutaneous coronary intervention
QOL: quality of life
TIMI: Thrombolysis In Myocardial Infarction
Introduction
Coronary chronic total occlusions (CTO) are common complex lesions that are variably treated among operators and institutions with percutaneous techniques1. One commonly cited reason for avoidance of CTO percutaneous coronary intervention (PCI) is the increased periprocedural risk of these procedures. However, there remains considerable variability in reported complication rates of CTO PCI2,3. Moreover, few of these studies have provided insights into the predictors of risk and the impact of complications on longer-term outcomes including patients’ health status trajectories. We sought to define more clearly the prevalence, predictors, and health status implications of procedure-related complications associated with the hybrid treatment approach to CTO PCI.
We leveraged the Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures (OPEN CTO) study in order to define accurately the frequency of in-hospital complications during CTO PCI, to develop a model using patient, anatomic, and physiologic variables to predict these complications, and to evaluate the association of these complications with health status measures over time. A better understanding of the prevalence, predictors, and health status implications of complications during CTO PCI in a real-world setting will serve to inform better the shared decision-making exercise between patients and practitioners prior to these complex procedures.
Methods
We used data from the OPEN CTO study, an investigator-initiated, single-arm, 12-centre registry of 1,000 patients who underwent CTO PCI between February 2014 and July 2015. The definitions, patients, procedures, and NCDR audit results that ensured the consecutive nature of enrolment have been published previously4. CTO was defined as a 100% occlusion with antegrade intraluminal Thrombolysis In Myocardial Infarction (TIMI) flow of 0 and clinical or angiographic evidence of occlusion duration ≥3 months. The study included adjudication by both a core lab and an events committee to prevent under-reporting (sensitivity) and improve specificity of angiographic and clinical events. Technical and procedural success have been described previously for this cohort4. Informed consent was obtained from every subject enrolled in the OPEN CTO study. Each participating institution’s own institutional review board approved the study.
HEALTH STATUS ASSESSMENT
Several patient-reported quality of life (QOL) health status measures were also captured in the OPEN CTO cohort at baseline and at 1-, 6-, and 12-month follow-up visits. These included the Seattle Angina Questionnaire (SAQ), the Rose Dyspnoea Scale, the EQ-5D visual analogue scale, and the PHQ-8 depression score. SAQ and EQ-5D scores range from 0-100, with higher scores denoting better health status. Rose scores range from 0-4 and PHQ-8 scores range from 0-24, both with lower scores denoting better health status. Methods used to collect follow-up health status measures have been published previously4.
DEFINING COMPLICATIONS
Unadjusted in-hospital complication rates both in aggregate and as individual components were reported. Complications collected included: all-cause death, periprocedural myocardial infarction (MI), coronary perforation (core lab adjudicated and categorised by the Ellis classification system for perforations), need for emergent cardiac or vascular surgery during or after the procedure, stroke/transient ischaemic attack, retroperitoneal bleed, donor vessel thrombosis (for retrograde cases), cardiogenic shock, and arrhythmia requiring defibrillation or placement of a temporary or permanent pacemaker5. In-hospital death was defined as death from any cause prior to discharge for the admission during which the index revascularisation procedure was performed. Periprocedural MI was defined according to the European Society of Cardiology/American College of Cardiology Foundation/American Heart Association/World Health Federation task force for the redefinition of myocardial infarction, specifically type 4a, defined as an increase in serum troponin level of more than three times the 99th percentile upper reference limit post PCI along with clinical evidence of ischaemia, including angina, new ECG changes suggestive of ischaemia, and/or new wall motion abnormalities on cardiac imaging6. As OPEN CTO was an observational registry, post-PCI cardiac enzyme testing was not mandated, and all post-PCI serological values were self-reported by the investigators. Major bleeding was defined using the NCDR definition7. Coronary perforations were classified by the Ellis classification system5. Definitions for the other complications have been previously described for OPEN CTO4.
STATISTICAL ANALYSIS
A priori selected predictors of procedure-related complications were evaluated using logistic regression8,9. These included age, body mass index (BMI), current smoking status, diabetes, prior MI, prior PCI, prior coronary artery bypass graft (CABG), prior stroke/transient ischaemic attack (TIA), peripheral arterial disease, chronic heart failure, chronic kidney disease, chronic lung disease, left ventricular systolic dysfunction (ejection fraction <40%), high-risk findings from non-invasive testing, Japanese chronic total occlusion (J-CTO) score (core lab adjudicated), additional coronary lesions attempted during the CTO PCI procedure, need for haemodynamic support, any use of the retrograde approach, radial access, and any deviation from the hybrid algorithm. Despite judicious selection, the final list comprised 21 degrees of freedom (DF), or approximately five events per DF, substantially lower than the 10-20 generally recommended to avoid overfitting in prediction models. To account for this, we used penalised maximum likelihood estimation, which injects a negative bias into the model estimates in order to reduce variances and improve predictive accuracy10. Multicollinearity was assessed by the condition index of the predictor matrix, which was 2.7, well below the threshold of 30 commonly used to indicate potential concerns. Continuous variables were entered as linear terms; an overall test of the presence of any non-linear effects was conducted using restricted cubic splines and was non-significant (p=0.48). Model calibration (comparison of observed and predicted outcomes) and discrimination (c-statistic) were assessed using bootstrap validation.
Among the 991 patients (99.1%) surviving their CTO PCI hospitalisation, we estimated the mean health status scores at each time point for those with and without periprocedural complications using linear mixed-effect models, including fixed effects for the presence of complications (yes/no), month of assessment, a complications-by-month interaction, and an unstructured within-patient covariance matrix to account for correlated assessments. The first model included all four time points, estimating unadjusted mean scores over time. A second model was then constructed among the follow-up assessments only, to estimate the effect of periprocedural complications on health status outcomes following CTO PCI, adjusting for baseline health status. In this model, if the interaction with time was significant (p<0.05), then effects were reported separately at each follow-up point; if not, then the model was re-run omitting the interaction term and an overall effect was estimated, averaging over the three follow-up assessments. Only two candidate predictors had missing values: LV systolic dysfunction (8.7% missing) and non-invasive test results (69.1% missing). In neither case was data completeness associated with the incidence of complications (p=0.87 and p=0.64, respectively). For modelling purposes, dummy indicator variables for missing data were constructed, to allow inclusion of all patients in the analysis. Among hospital survivors, missing follow-up health status scores occurred due to death (3.2%), lost to follow-up (9.8%) and skipped items/incomplete assessments (range 1.7% to 3.8% depending on the instrument). Missing scores were assumed to be missing at random conditional on observed scores at other time points; the mixed-effect models described above correct for biases attributable to this type of missingness. Furthermore, we conducted a sensitivity analysis repeating the above analyses among patients who survived to one year.
All statistical analyses were performed with SAS, version 9.4 (SAS Institute, Inc., Cary, NC, USA) and R version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria)11.
Results
Baseline patient and procedural characteristics for the entire cohort and those with and without periprocedural complications are summarised in Table 1. The majority of patients in the cohort were Caucasian and male, 40% were diabetic, and 36% had prior bypass. One third (35.3%) had left ventricular systolic dysfunction (ejection fraction <55%). Compared to patients who did not experience complications during CTO PCI, patients with complications were more likely to be older (p<0.01), female (p=0.02), have a lower BMI (p<0.01), have chronic lung disease (p=0.01), have higher baseline J-CTO scores (specifically the presence of calcium in the lesion [p<0.01] and bending >45 degrees [p=0.01]), and had dissection re-entry methods used during the case (p=0.02 for anterograde and p<0.01 for retrograde dissection re-entry). The overall core lab adjudicated procedural success rate was 86.2% and most (88.4%) of the procedures were undertaken for symptomatic relief and/or ischaemia reduction/complete revascularisation, as previously reported4.
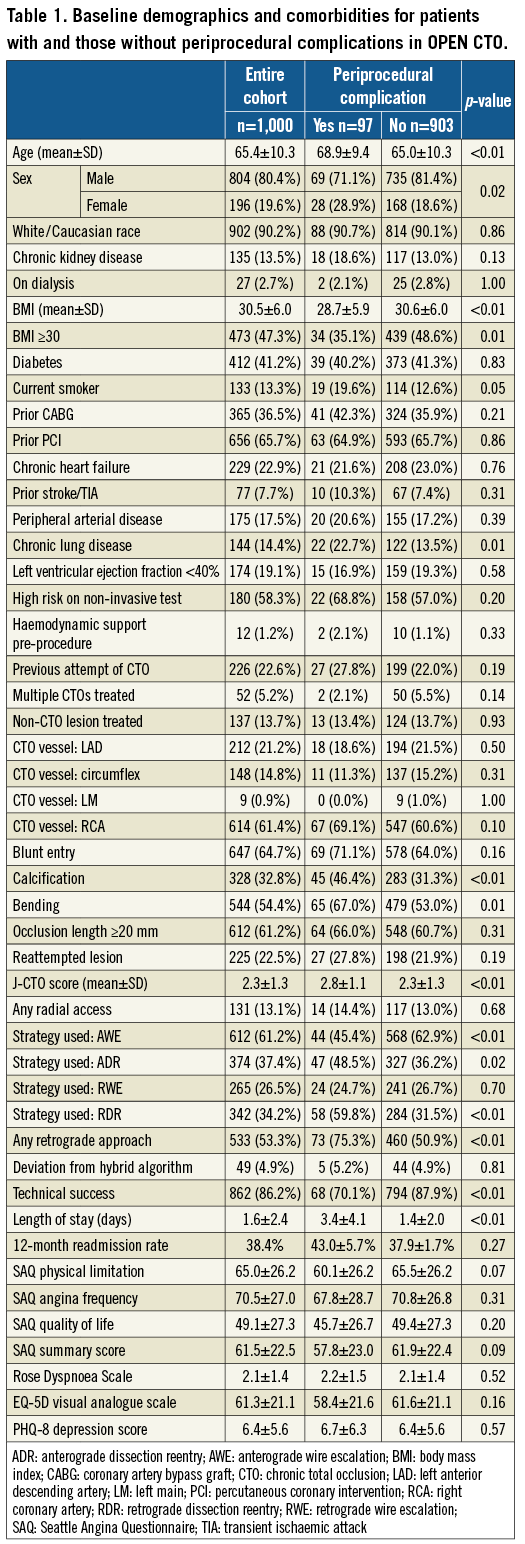
The overall periprocedural complication rate for this cohort was 9.7% (n=97), as shown in Table 2. The most common adverse events were clinical perforation (8.8%, n=88); of those, 48/88 (54.5%) required some form of urgent treatment. Half (50.0%, n=44/88) of the perforations were Ellis grade II. Grade III perforations were observed in 33 (37.5%). Cavity spilling was identified in 5/33 (15.2%) of the grade III perforations. Periprocedural MI was identified in 26 patients (2.6%), arrhythmias requiring treatment in 12 (1.2%) and cardiogenic shock in 11 (1.1%). A total of 107 patients (10.7%) had post-procedural cardiac enzymes drawn (40 troponin-T only, 19 troponin-I only, 28 CK-MB only, 14 troponin-T+CK-MB, 6 troponin-I+CK-MB). There were nine procedure-related deaths (0.9%). All procedural deaths were associated with perforation and occurred among patients with previous CABG surgery. Twelve-month mortality rates were compared between those with and those without periprocedural complications (Table 3). As shown, there was a significant increase in mortality rates for those with complications compared to those without that became evident at one month and persisted at one-year follow-up (12.4% compared to 3.1%, respectively, p<0.01). After adjusting for differences in baseline clinical characteristics, only the use of the retrograde approach (OR 1.98, 95% CI: 1.32 to 2.99), age (OR 1.30, 95% CI: 1.07 to 1.58 per 10-year increment), J-CTO score (OR 1.20, 95% CI: 1.03 to 1.41 per +1 point) and lower BMI (OR 0.84, 95% CI: 0.70 to 0.99 per +5 kg/m2) were independently associated with complications (Figure 1). Complications were higher in those where the retrograde approach was used (75.3% versus 50.9%, p<0.01). However, we were unable to delineate differences between the various types of retrograde approach further (septal vs. epicardial, versus bypass graft) due to the small numbers in each group. Using bootstrap validation, calibration of the penalised regression model was excellent (slope and intercept of observed vs. predicted values –0.01 and 1.00, respectively), though discrimination was modest (c-statistic=0.68).
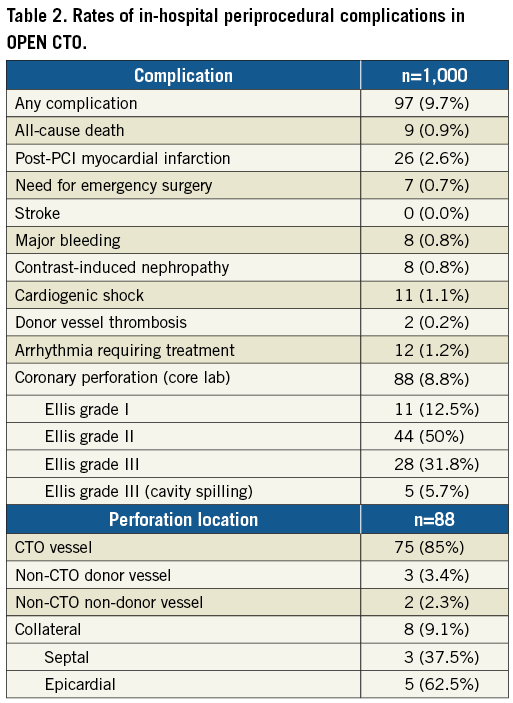
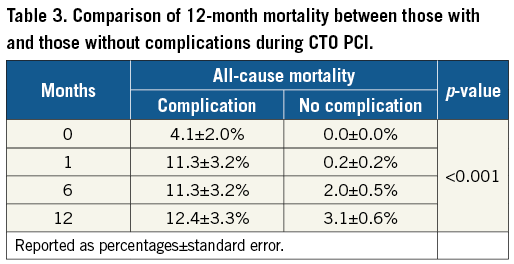
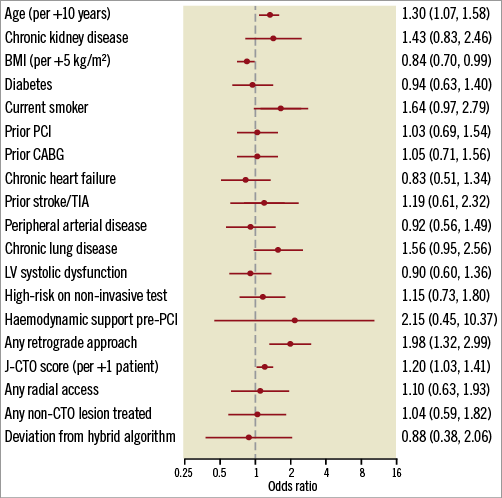
Figure 1. Adjusted odds ratios for clinical and anatomic predictors of in-hospital complications during chronic total occlusion angioplasty.
Unadjusted mean health status scores at baseline and at 1-, 6-, and 12-month follow-up among hospital survivors are displayed in Figure 2. In general, patients with and without non-fatal periprocedural complications had non-statistically significant differences in baseline QOL metrics. However, patients with non-fatal periprocedural complications had lower follow-up QOL scores. In analyses adjusting for baseline health status, non-fatal complications were associated with significantly worse mean follow-up health status scores for all measures except SAQ physical limitation, as shown in Supplementary Table 1. For example, patients with periprocedural complications reported a 3.7 point (95% CI: –0.64 to –0.9, p<0.01) lower mean SAQ summary score at 12-month follow-up compared to those without a periprocedural complication. As shown, interactions with time were found for SAQ angina frequency and PHQ-8 scores, with angina frequency showing statistically significant worse scores among patients who experienced non-fatal complications during the 12-month follow-up.
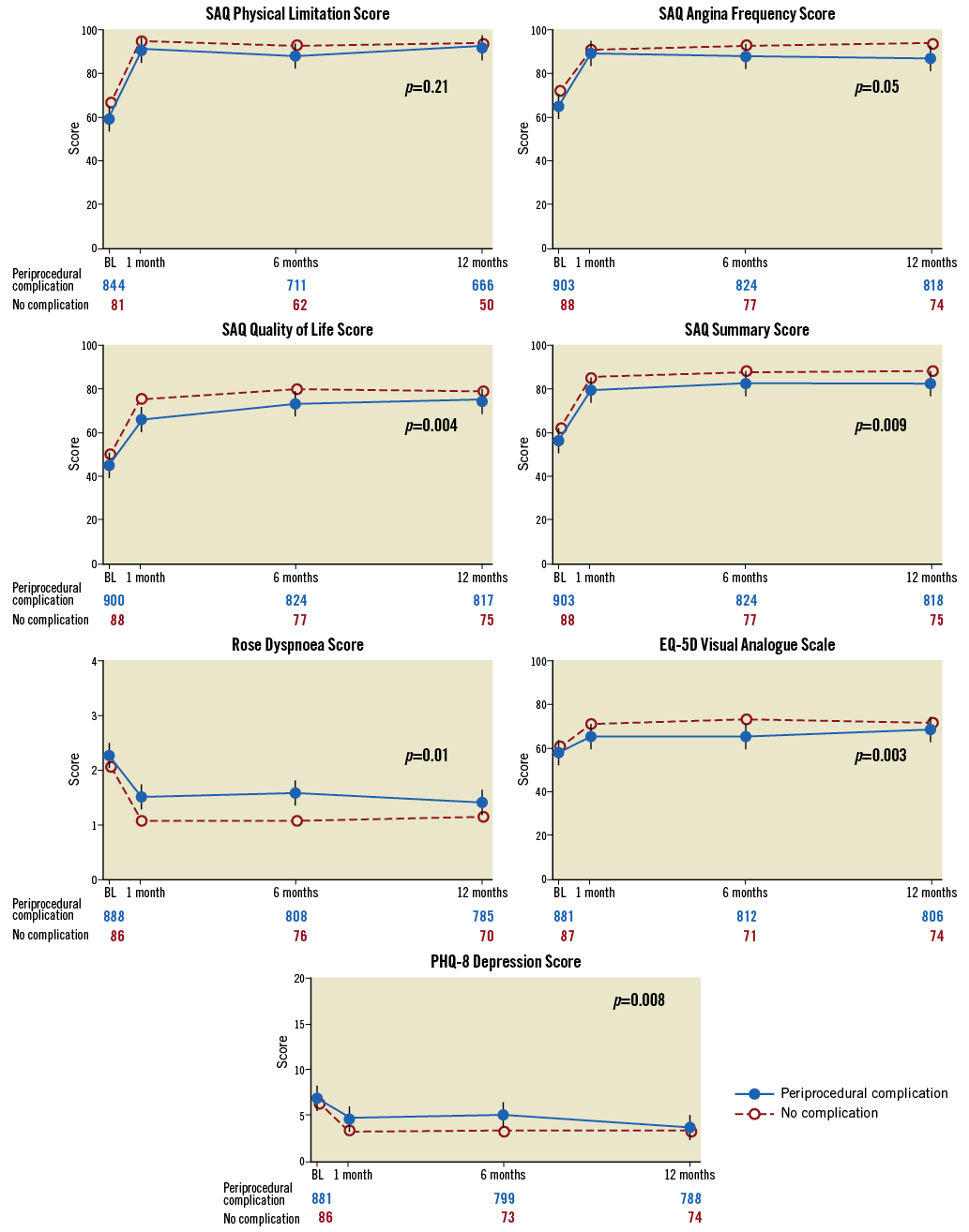
Figure 2. Unadjusted mean health status scores among patients with and those without periprocedural complications over 12-month follow-up. SAQ and EQ-5D scores range from 0-100, with higher scores denoting better health status. Rose scores range from 0-4 and PHQ-8 scores range from 0-24, both with lower scores denoting better health status. Vertical bars denote 95% confidence limits; p-values reflect tests of any difference in follow-up health status, adjusting for baseline health status.
In order to delineate the effects of technical success versus complications on QOL metrics further, we stratified QOL metrics by technical success and complication (Supplementary Figure 1), as well as adjusted effects of technical success and complications in multivariable models (Supplementary Table 2). These data show: (1) patients who had technical success and no complications had the best health status outcomes, and (2) technical success versus failure was more strongly associated with QOL outcomes than with the presence vs. absence of complications. This was also found in multivariable analyses, showing highly significant effects of technical success on mean health status outcomes. After adjusting for technical success, the association of complications with health status outcomes was notably reduced, achieving statistical significance only for the SAQ quality of life, EQ-5D VAS and PHQ-8 depression scores. For example, in adjusted analyses, technical success was associated with a 6.0 higher mean SAQ summary score (95% CI: 3.8 to 8.3, p<0.001); after adjusting for success, complications were still associated with lower scores, although not significantly so (mean –2.4, 95% CI: –5.2 to 0.4, p=0.09). There was no significant interaction between success and complications.
Discussion
In the OPEN CTO study, we found that CTO PCI was associated with a 9.7% in-hospital complication rate, with the most common events being coronary perforation, periprocedural MI, arrhythmia requiring treatment, cardiogenic shock, and death. Adjusted analyses of pre-specified clinical and anatomic risk factors for these complications showed that retrograde approach, increasing age, and increasing anatomic complexity of the lesion as reflected by J-CTO score were all significant predictors of complications in this group. Additionally, we found that patients who experienced periprocedural complications had worse health status scores after the procedure, though this was significantly mitigated in those with technical success.
Prior analyses of CTO PCI complication rates have been limited to a meta-analysis and data from the PROGRESS and RECHARGE registries. The meta-analysis reported a pooled complication rate of 3.1% among 18,061 cases, similar to rates in non-CTO PCI3. However, given the nature of the report as a meta-analysis, it had significant limitations such as its retrospective nature, reporting bias, inclusion of studies before wide dissemination of the hybrid algorithm, significant heterogeneity of the data and definitions used for reporting, and lack of auditing and core lab analysis. The PROGRESS registry reported overall periprocedural complication rates during hybrid CTO of 2.8% from 1,569 cases. Complications reported included death (0.6%), periprocedural MI (1.0%), emergent CABG (0.1%), stroke (0.3%), need for repeat PCI (0.3%), and tamponade from coronary perforation requiring pericardiocentesis (1.0%)2. RECHARGE was a similar contemporary European registry that reported an overall complication rate of 2.6%, with similar rates of death (0.2%), stroke (0.2%), periprocedural MI (2.2%), major bleeding (1.9%), and tamponade (1.3%). Our study reports higher overall composite and constituent complication rates compared to both of the other registries. One of the major differences was how coronary perforation rates were reported. Our analysis reported core lab adjudicated angiographic coronary perforations instead of just clinically reported perforations given the significant correlation with perforations and in-hospital death. Core lab adjudication of this endpoint is novel in OPEN compared to previously reported data and illustrates the difference between provider-reported complications and core lab adjudicated reporting, which probably affects previously reported coronary perforation rates during CTO PCI.
Independent predictors of procedural complications were similar between the data reported from the OPEN CTO and PROGRESS registries. Both found that increased age and any use of the retrograde approach were associated with increased procedural risk, which was also shown in a retrospective analysis of several experienced US CTO centres by Karmpaliotis et al in 201612. While the PROGRESS data also noted that increased lesion length was a significant predictor, this is similar to our data showing that increased J-CTO scores were an independent predictor of complications in the OPEN CTO data as a marker of overall anatomic complexity. The similarities in findings between these two large prospective registries adds significant weight to the idea that these markers are truly predictors of elevated procedural risk in this patient cohort. However, these predictors differ somewhat from the independent predictors of major adverse cardiac and cerebrovascular events at long-term follow-up reported from the European ERCTO registry and thus require further validation13.
While there have been a multitude of prior studies evaluating the health status benefits of PCI in stable ischaemic heart disease (both non-CTO and CTO lesions), there remains a lack of information about how complications during PCI affect these metrics, both in CTO and non-CTO lesions14,15. This study is one of the first to address how complications are associated with health status after PCI and has the advantage of having 12-month follow-up. Not surprisingly, health status scores at clinical follow-up were comparatively worse for those with complications compared to those without across nearly all measures. Interestingly, the decrease in health scores seen in patients with complications was significantly mitigated in those with technical success, which probably speaks for the benefit of establishing anterograde flow in vessels with CTOs.
Limitations
One of the major limitations of this analysis was the small number of events and restriction to in-hospital events with resulting possible uncertainty in identifying significant predictor variables. However, our use of methods to mitigate overfitting and the fact that our findings are similar to those from PROGRESS support the validity of these findings.
Regarding core lab adjudicated perforations, it is possible that there was over-reporting of Ellis class I perforations. Subintimal re-entry techniques by definition create a space between the true lumen and the adventitia and can have the appearance of a “crater” in the vessel wall, which could overlap with the definition of a class I perforation, especially for core lab adjudication where lab reviewers only have limited cine runs to define angiographic variables.
Conclusions
While procedural success rates for CTO PCI are increasing, complication rates for these procedures are higher than those for non-CTO PCI, particularly in older patients, more complex lesions, and when the retrograde approach is utilised. These complications also appear to include long-term health status ramifications, though this effect is significantly mitigated in those with technically successful procedures. These findings can be used to inform patients better during the consent process, aid in case selection based on operator experience, and facilitate further investigations regarding risk mitigation strategies for these procedures.
| Impact on daily practice Coronary CTOs are common lesions found on angiography. The complication rates during CTO PCI are higher than those reported for non-CTO PCI and are increased with the retrograde approach, increasing patient age, and increasing lesion complexity. Additionally, there are long-term health status outcomes associated with complications during CTO PCI. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Supplementary Figure 1. CTO PCI quality of life scores stratified by technical success and procedural complications.
Supplementary Table 1. Baseline-adjusted differences in mean health status scores, for patients with compared to those without periprocedural complications during CTO PCI from the OPEN CTO registry.
Supplementary Table 2. Adjusted differences in follow-up health status for patients with versus those without complications, adjusting for technical success.
To read the full content of this article, please download the PDF.