Abstract
Background: The EROSION study demonstrated that patients with an acute coronary syndrome (ACS) caused by plaque erosion could be treated with antithrombotic therapy without stenting. However, the long-term prognosis of this strategy is still unclear.
Aims: The aim of this study was to test whether a non-stenting antithrombotic strategy was still effective at four-year follow-up and to explore potential predictors of long-term prognosis.
Methods: This study was a long-term follow-up of the EROSION study. Follow-up was conducted by phone call or clinical visit. Patients were divided into two groups – those with target lesion revascularisation (the TLR group), and the non-TLR group.
Results: Out of 55 patients who completed one-month follow-up, 52 patients finished four-year follow-up. The median duration was 4.8 years (range, 4.2-5.8 years). The majority of patients remained free from events, and all patients were free from hard endpoints (death, myocardial infarction, stroke, bypass surgery, or heart failure). Only one patient had gastrointestinal bleeding, and 11 patients underwent TLR. Patients in the non-TLR group had more optical coherence tomography (OCT) thrombus reduction from baseline to one month; 95% of patients in the non-TLR group versus 45% in the TLR group (p=0.001) met the primary endpoint (thrombus volume reduction >50%). Angiographic results showed that the TLR group had less improvement in diameter stenosis (p=0.014) at one month compared with the non-TLR group.
Conclusions: Four-year follow-up findings reconfirmed the safety of an antithrombotic therapy without stenting for ACS caused by erosion. Patients with better response to antithrombotic therapy in the first month were less likely to require stent implantation during the next four years.
Introduction
Early and late stent-related complications (stent thrombosis and stent restenosis) remain challenging problems, especially in patients presenting with acute coronary syndrome (ACS) and undergoing primary percutaneous coronary intervention (PCI) with stent implantation, without taking into consideration differences in underlying mechanisms1,2,3. Plaque rupture and plaque erosion are the most common causes of ACS, accounting for 60-70% and 30-40% of ACS, respectively4. However, plaque erosion differs from plaque rupture because erosions have less lipid and more platelet-rich thrombus, and patients with erosions are more often smokers and female5,6,7. Because optical coherence tomography (OCT) allows in vivo detection of plaque erosion (vs plaque rupture)8, we performed a proof-of-concept study entitled EROSION (Effective Anti-Thrombotic Therapy Without Stenting: Intravascular Optical Coherence Tomography-Based Management in Plaque Erosion) to test the safety and feasibility of not stenting erosion ACS-related culprit lesions. Favourable results were observed at one month and one year9,10. In the current study we report four-year outcomes.
Methods
STUDY DESIGN
This study was a long-term follow-up of the EROSION study. The EROSION study was a single-arm, prospective, proof-of-concept study (NCT02041650); the detailed protocols have been published previously9,10. Briefly, when an ACS patient was diagnosed as having plaque erosion by OCT with <70% residual angiographic diameter stenosis (DS) after thrombus aspiration, Thrombolysis In Myocardial Infarction (TIMI) flow grade 3, and no progressive chest pain, the patient was treated with antithrombotic therapy without stenting. Manual aspiration and glycoprotein IIb/IIIa inhibitor (GPI) use were based on clinical practice. The primary endpoint was >50% reduction of thrombus volume measured by OCT at one month. Major adverse cardiovascular events (MACE: a composite of cardiac death, reinfarction, re-hospitalisation due to unstable or progressive angina, clinically driven target lesion revascularisation [TLR], stroke, and major bleeding) were the secondary endpoints.
In the present study, clinical follow-up was carried out either by phone call or by clinical visit every three months in the first year and annually after 12 months. A questionnaire collected detailed information of clinical events during the four years including MACE, quality of life, and medications. Detailed definitions of each event have been listed in previous papers9,10. Medications included aspirin, ticagrelor/clopidogrel, statins, β-blockers, angiotensin-converting enzyme inhibitors (ACEI), and angiotensin receptor blockers (ARB).
A detailed methodology of angiographic and OCT image analysis has been described in previous studies9,10. This study was approved by the Ethics Committee of the Second Affiliated Hospital of Harbin Medical University (Harbin, China). All patients provided written informed consent.
STATISTICAL ANALYSIS
SPSS, Version 25.0 (IBM Corp., Armonk, NY, USA) was used to analyse all data. The Kolmogorov-Smirnov test was used for continuous variables to determine their distribution. An independent samples t-test was used for normally distributed variables and the Mann-Whitney U test for non-normally distributed variables. Continuous variables are shown as mean±SD for normally distributed variables or median (interquartile range) for non-normally distributed variables. Categorical data are shown as absolute frequencies (percentages) and analysed using the chi-square test or Fisher’s exact test. A multivariable logistic regression analysis was conducted to explore independent predictors of TLR. Receiver operating characteristics with area under the curve (AUC) were used to determine the best cut-off value for continuous predictors of TLR. A two-tailed p-value <0.05 was considered statistically significant.
Results
Among 55 EROSION study patients who finished one-month follow-up, 52 patients completed four-year follow-up (median duration of 58 months [4.8 years]) (Figure 1). Two patients were lost to follow-up, and one quit the study because a computed tomography (CT) scan confirmed an aortic ulcer at one month. No patient experienced death, stroke, recurrent myocardial infarction (MI), coronary artery bypass grafting (CABG), or heart failure.
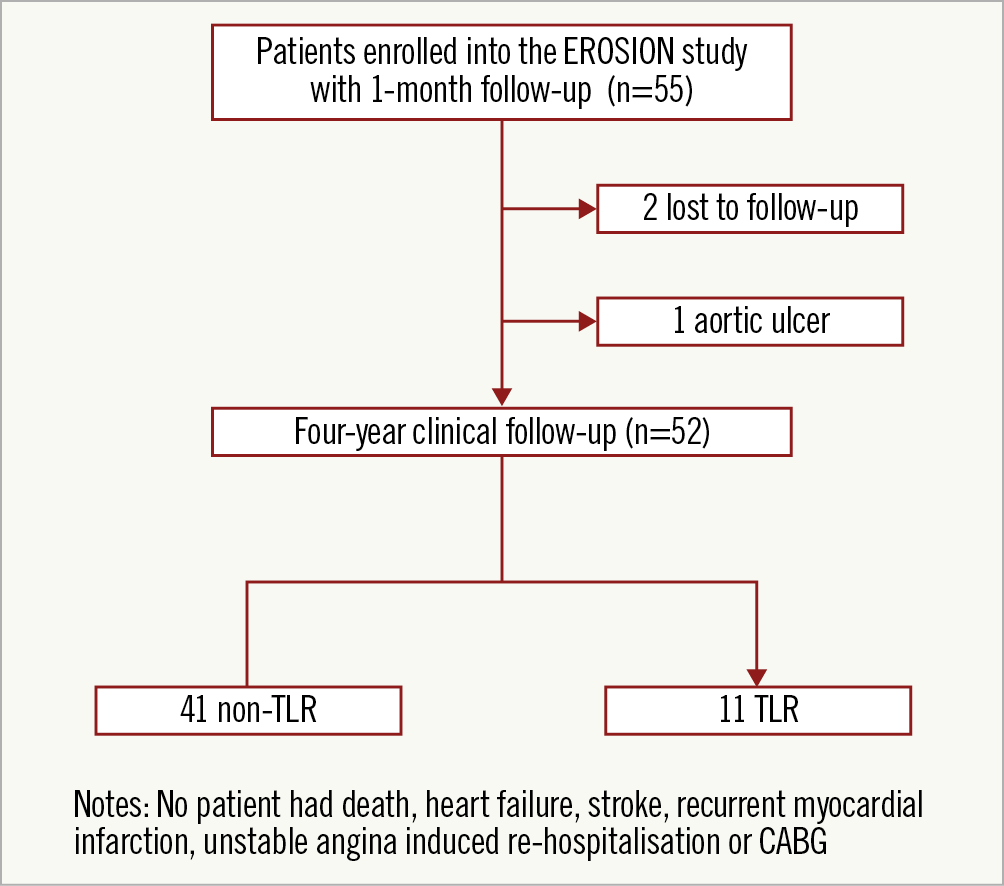
Figure 1. The study flow chart. CABG: coronary artery bypass grafting; TLR: target lesion revascularisation
At four years, 11 out of 52 patients (21%) underwent elective PCI with stent implantation while the other 41 (79%) remained free from revascularisation. Ten of them underwent revascularisation because of exertional angina, and one patient was stented because of a tight stenosis on angiography at one-month follow-up. Timing and angiographic information for these 11 patients at the time of repeat revascularisation is shown in Figure 2 and Supplementary Table 1. Five patients underwent TLR within one year, and six patients were stented between one and four years.
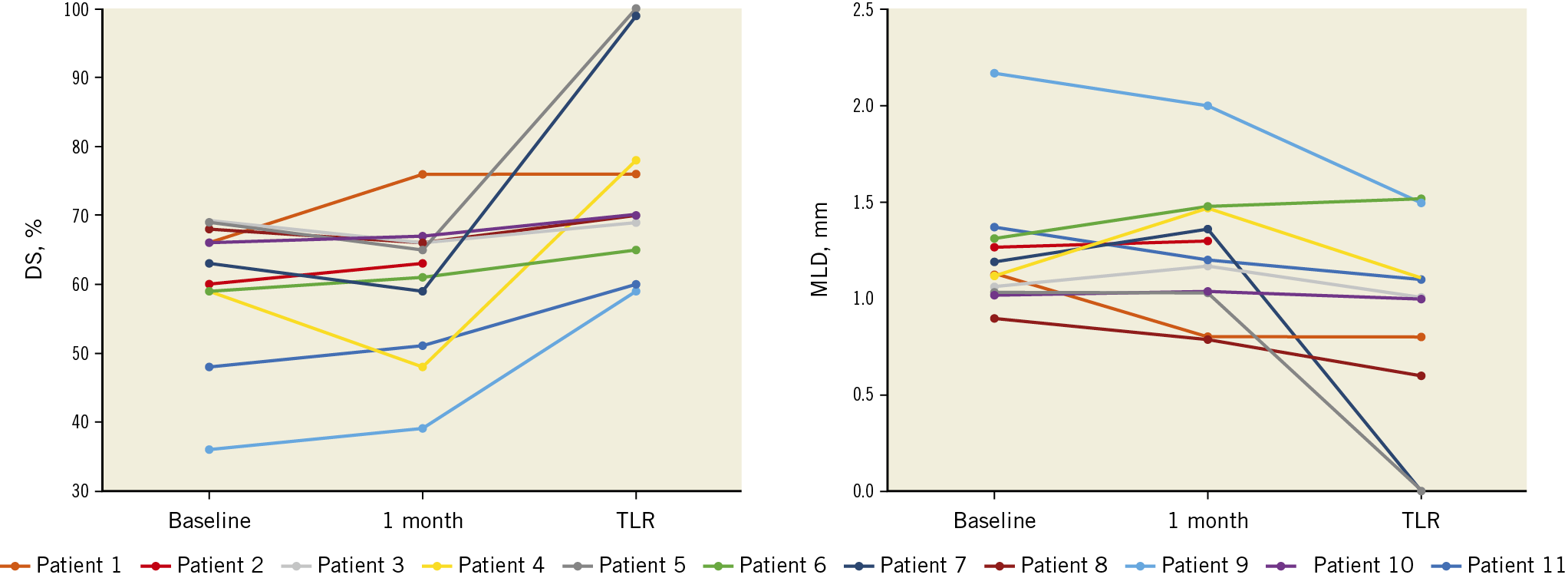
Figure 2. Detailed angiographic progressions of the 11 TLR patients between baseline and revascularisation. DS: diameter stenosis; MLD: minimal lumen diameter; TLR: target lesion revascularisation
Details of medications and clinical events at four years are reported in Supplementary Table 2. All patients were on dual antiplatelet therapy (DAPT) for at least 12 months, except for one patient who stopped ticagrelor at three months due to gastrointestinal bleeding. At four-year follow-up, 44 of 52 (85%) patients continued to take aspirin, 6 of 52 (12%) continued to receive DAPT, and 34 patients (65%) were on statins with a higher tendency in the TLR group versus the non-TLR group (10 [91%] vs 24 [59%], p=0.073).
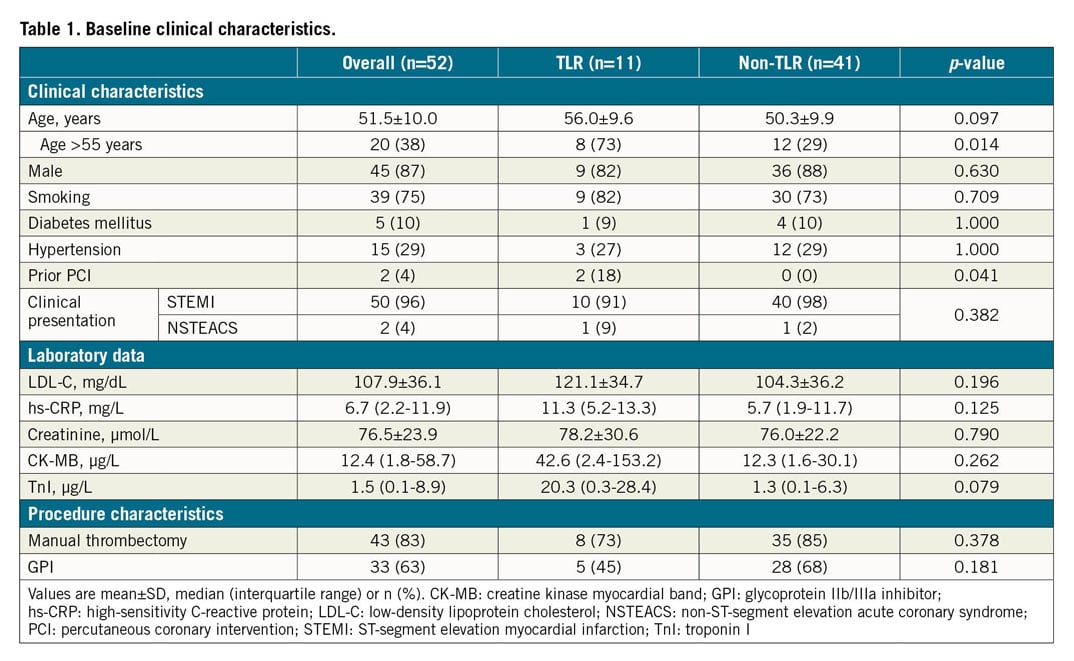
BASELINE CLINICAL, ANGIOGRAPHIC AND OCT FINDINGS IN PATIENTS WITH VERSUS THOSE WITHOUT TLR DURING FOUR-YEAR FOLLOW-UP
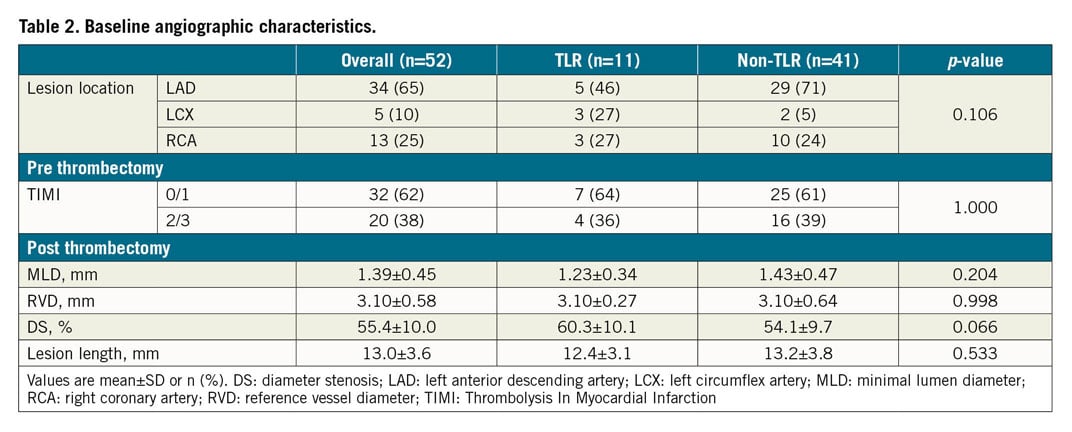
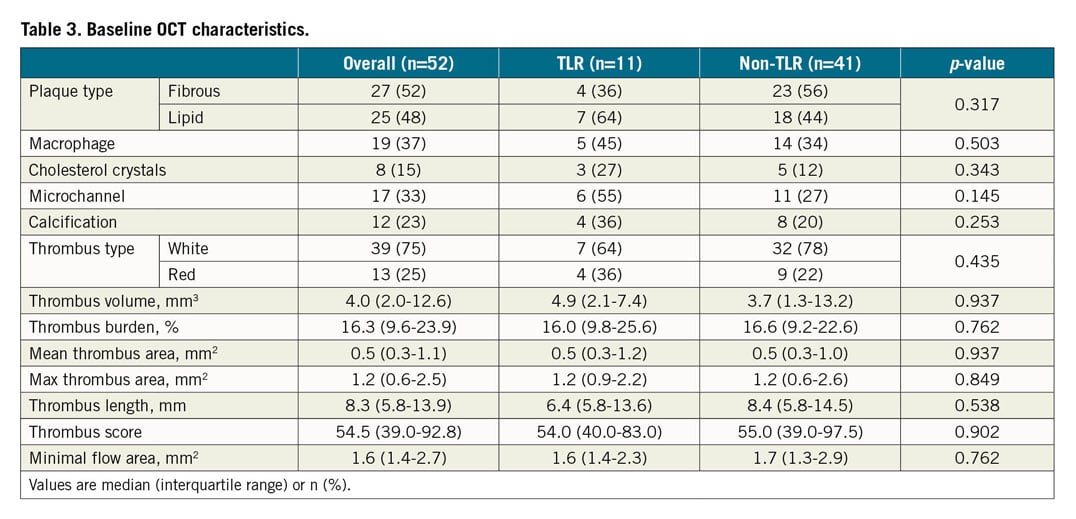
Baseline characteristics of patients with versus those without four-year TLR are shown in Table 1-Table 3. TLR patients tended to be older (56.0±9.6 vs 50.3±9.9 years, p=0.097) and more were >55 years of age (8 [73%] vs 12 [29%], p=0.014). Other cardiovascular risk factors and biomarkers were comparable. Except for a higher post-PCI angiographic DS (60.3±10.1% vs 54.1±9.7%, p=0.066) in the TLR group, lesion location and pre-PCI lesion severity were similar between the two groups.
CLINICAL, ANGIOGRAPHIC, AND OCT FINDINGS AT 30 DAYS IN PATIENTS WITH VERSUS THOSE WITHOUT TLR DURING FOUR-YEAR FOLLOW-UP
One-month follow-up data are summarised in Table 4, Table 5, and Supplementary Table 3. After 30 days of antithrombotic treatment, patients in the non-TLR group showed improvement in terms of reduction in the angiographic DS (10.7±13.3% vs −0.1±9.1%, p=0.014) when compared with those in the TLR group, resulting in a smaller DS (48.2±11.2% vs 60.1±10.4%, p=0.003) and a larger minimum lumen diameter (1.60±0.55 vs 1.24±0.35 mm, p=0.044) at follow-up (Figure 3).
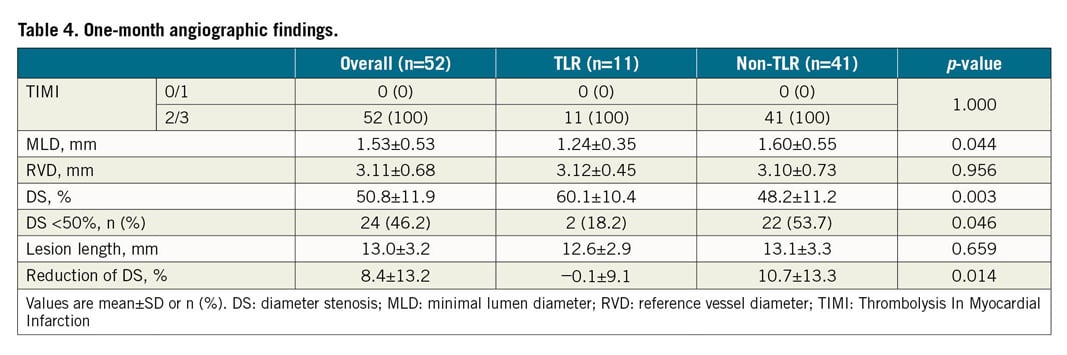
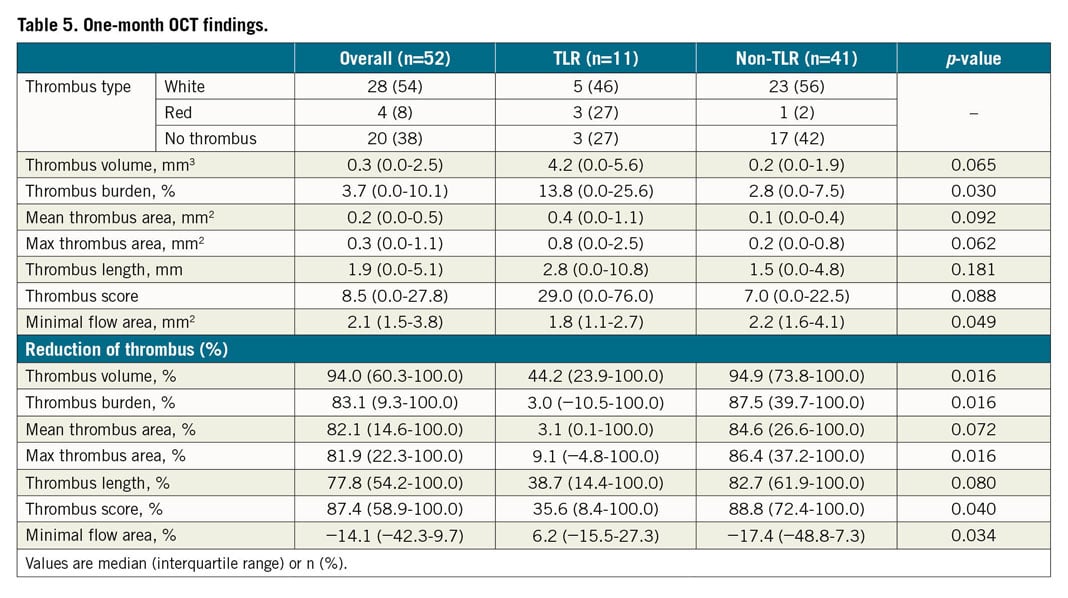
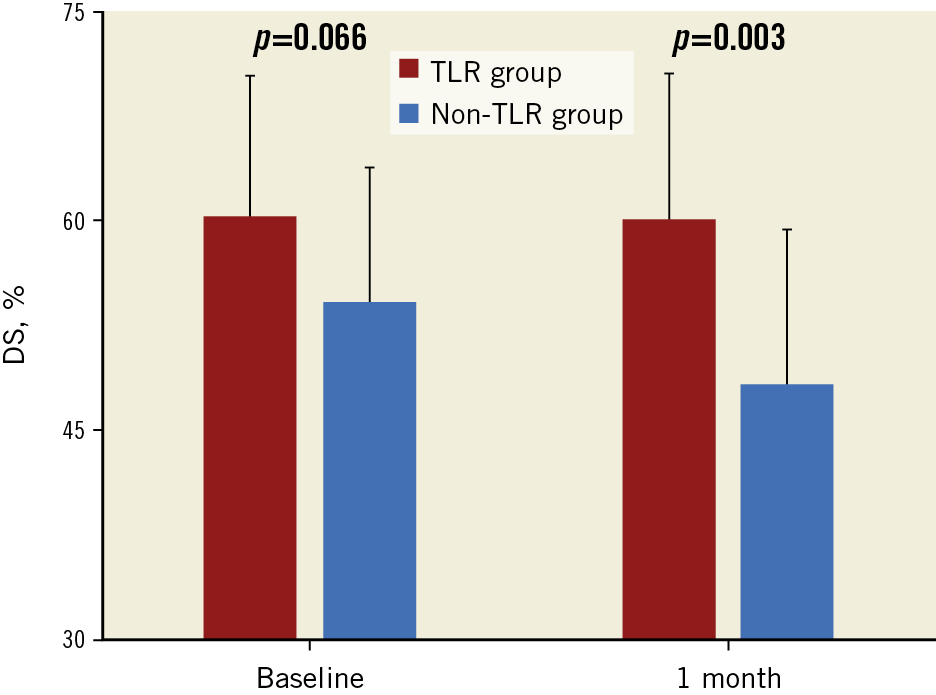
Figure 3. Angiographic DS evolution from baseline to one month. TLR patients had more severe DS at one-month follow-up. There was less lesion regression (DS reduction) in the TLR group after one-month antithrombotic therapy. DS: diameter stenosis; TLR: target lesion revascularisation
Notably, in the four-year non-TLR group compared to the TLR group there was a larger reduction in thrombus volume (94.9 [73.8-100.0] % vs 44.2 [23.9-100.0] %, p=0.016), thrombus burden (87.5 [39.7-100.0] % vs 3.0 [−10.5-100.0] %, p=0.016), maximum thrombus area (86.4 [37.2-100.0] % vs 9.1 [−4.8-100.0] %, p=0.016), and thrombus score (88.8 [72.4-100.0] % vs 35.6 [8.4-100.0] %, p=0.040) at one month, indicative of more thrombus dissolution during this initial one-month period. Fewer than 50% of patients who underwent TLR within the four-year follow-up period reached the primary endpoint of the EROSION study (thrombus volume decrease >50% at one month), whereas almost all patients in the non-TLR group achieved this primary endpoint (5 [45%] vs 39 [95%], p=0.001) (Figure 4). Representative cases of TLR and non-TLR are shown in Figure 5 and Figure 6.
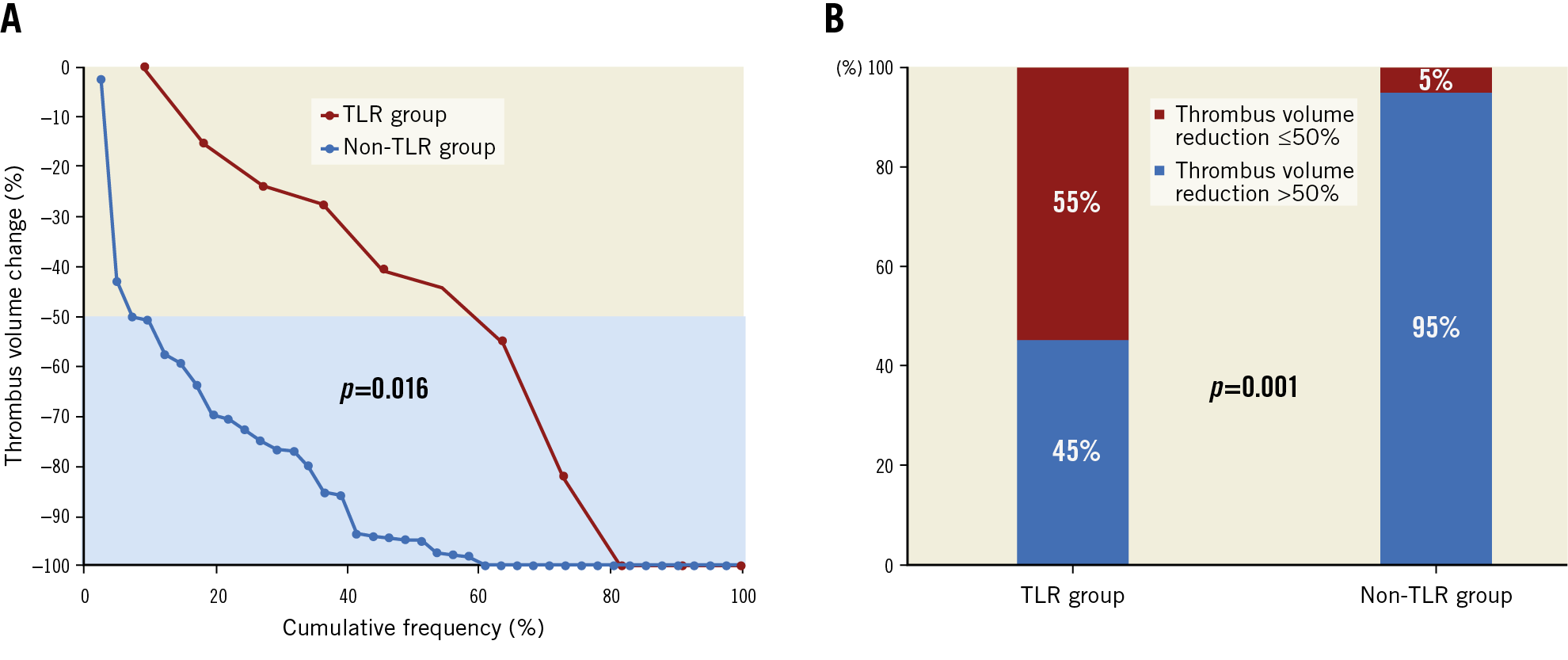
Figure 4. Thrombus reduction after one-month effective antithrombotic therapy in the TLR versus the non-TLR group. A) Individual thrombus volume evolution in the TLR versus the non-TLR group. B) Percentage of thrombus volume decrease >50% in the TLR versus the non-TLR group. TLR: target lesion revascularisation
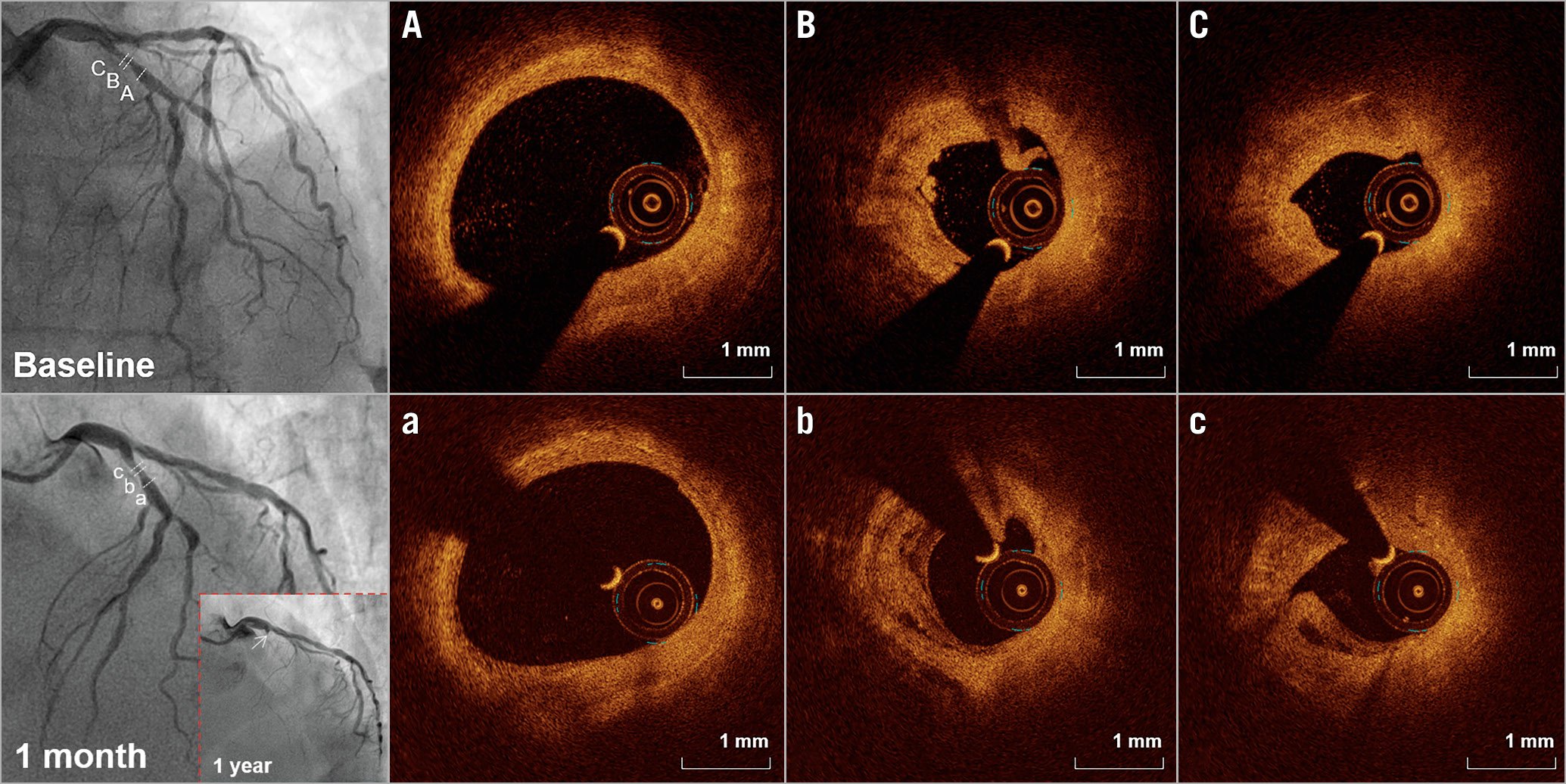
Figure 5. Representative case with target lesion revascularisation. A 69-year-old female without cardiovascular risk factors presented with STEMI with a 65% angiographic stenosis in the LAD after manual thrombectomy (upper left). OCT showed plaque erosion in the culprit site (A-C). After one-month antithrombotic therapy, there was no improvement on the angiogram (lower left) and no thrombus reduction on the OCT images (a-c). The patient had angina at one-year follow-up and the angiogram showed total occlusion (white arrow). Stent implantation was performed. LAD: left anterior descending artery; OCT: optical coherence tomography; STEMI: ST-segment elevation myocardial infarction
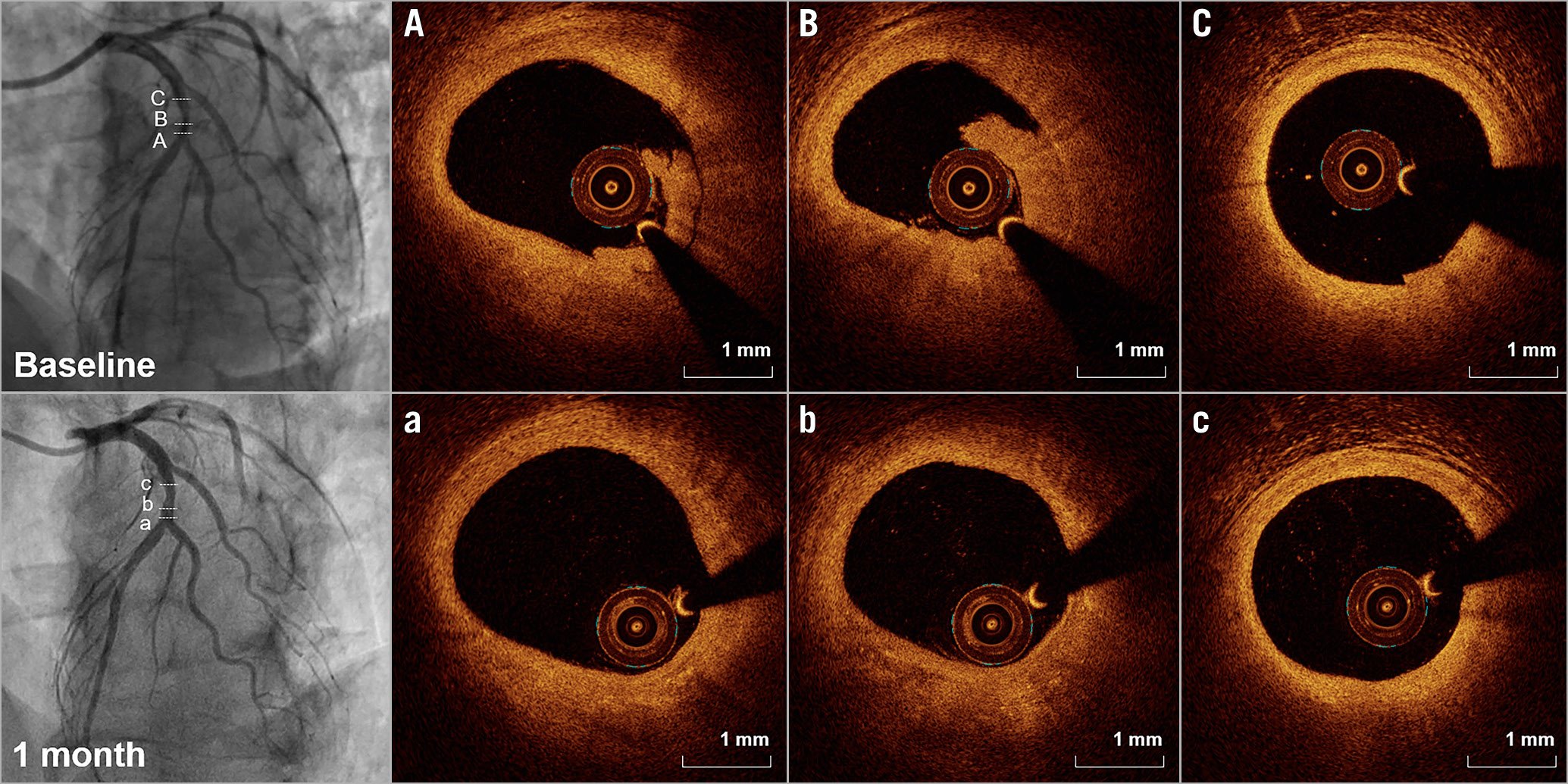
Figure 6. Representative case without target lesion revascularisation. A 56-year-old male without cardiovascular risk factors presented with STEMI with a 50% angiographic stenosis in the LAD after manual thrombectomy (upper left). Plaque erosion was detected by OCT (A-C). After one-month antithrombotic therapy, there was a significant improvement in the angiogram (lower left) and no residual thrombus on OCT images (a-c). The patient remained well at a five-year follow-up. LAD: left anterior descending artery; OCT: optical coherence tomography; STEMI: ST-segment elevation myocardial infarction
PREDICTORS OF TLR
According to clinical features, the evolution of angiographic and OCT characteristics during one-month follow-up, and the results of univariate analysis and their mechanistic relationship to TLR, we selected four variables to test in the multivariate analysis – patient age, angiographic DS improvement at one month, thrombus volume reduction at one month, and OCT minimal flow area at one month. There was no correlation (Pearson’s correlation, p<0.01) among any of these variables. Thrombus volume reduction at one month was the only independent predictor of TLR during four years of follow-up (odds ratio [OR], 0.97) (Supplementary Table 4). Using receiver operating curves, the best cut-off value of one-month thrombus volume reduction to predict TLR was 56.2% (AUC: 0.731, Youden’s index: 0.539, sensitivity: 0.902, specificity: 0.636, p=0.020), very close to the primary endpoint of the EROSION study.
Discussion
In the current study we report the long-term outcomes of ACS patients with OCT-detected culprit lesion plaque erosion who were treated without stent implantation during the primary PCI. The main findings of this study are as follows. (1) The majority of patients remained free from events (and all patients were free from hard events such as death, stroke, recurrent MI, CABG, or heart failure) at a median follow-up time of 58 months, reconfirming the feasibility and safety of a non-stenting strategy for patients with ACS caused by erosion. (2) The overall TLR rate was 21% at four-year follow-up. (3) Patients who improved from baseline to one month (based on OCT assessment of thrombus burden) were the ones who did well at four (or more) years of follow-up.
COMPREHENSIVE EVALUATION OF THE EROSION STUDY
Previous studies, as well as the one-month and one-year results of the EROSION study, suggested that ACS patients with an intact culprit lesion fibrous cap or an OCT-detected culprit erosion did better than patients with culprit lesion plaque rupture and could be treated without stent implantation during the primary PCI9,10,11,12,13,14. However, the long-term (beyond one year) safety of this strategy and, in particular, the rate of recurrent MI was not addressed. The cumulative rate of MACE and TLR in the current study was 23% (12 of 52) and 21% (11 of 52), respectively, with a median follow-up time of five years. MACE were primarily related to TLR in the current study, except for one patient with gastrointestinal bleeding at three months. In particular, all TLR in the present study were non-emergent and not associated with an ACS.
INSIGHTS ON POTENTIAL MECHANISMS OF TLR
Based on the angiographic findings that patients who underwent revascularisation showed significant progression with greater severity of stenosis and smaller luminal diameter compared to baseline, organisation of residual thrombus probably contributed to lesion progression. This was also supported by OCT findings that thrombus volume reduction at one month was significantly smaller in patients with TLR versus those without TLR. Considering previous studies and the angiographic findings during revascularisation, we speculated that the possible mechanisms of TLR in the current erosion patients treated conservatively were insufficient dissolution of residual thrombus and the formation of new thrombus during the process of residual thrombus organisation, leading to lesion progression4,15. Different from the rapid and massive thrombosis in the acute setting of MI, this might be a chronic and repeated process of thrombosis followed by organisation.
The underlying mechanism for insufficient thrombus dissolution might be the poor response to antithrombotic treatment, which is affected by several factors such as age, race, genetic polymorphism, etc.16. There is a relationship between high platelet reactivity (HPR) and ischaemic events17, although the feasibility of HPR to predict clinical outcomes is still controversial18,19. Besides, the emergence of new P2Y12 inhibitors has provided increased benefits, especially in ACS patients. In the current study, all patients took a new P2Y12 inhibitor (ticagrelor) for at least one year.
CLINICAL IMPLICATIONS
The current study results highlight the importance of responsiveness to antithrombotic therapy in erosion patients treated with a non-stenting strategy, particularly during the first month. Patients with the greatest thrombus dissolution at one month were less likely to require revascularisation at long-term follow-up. While procedural OCT is necessary to identify patients with a culprit lesion erosion, one-month OCT in all such patients is not feasible. Thus, further study should focus on the use of non-invasive methods (such as coronary CT angiography) to identify high-TLR-risk individuals in whom more intensive (or longer-term) medical treatment may be needed. Also, biomarkers should be collected and tested for their ability to identify high-TLR-risk patients. Nevertheless, it is reassuring that, even without a one-month imaging assessment, a non-stenting strategy in these patients may not be associated with an increased frequency of death, MI, stroke, CABG, or heart failure. Conversely, recent studies have focused on high bleeding risk patients as well as on the bleeding complications with long-term dual antiplatelet therapy. Only one patient in the current study had bleeding.
Limitations
First, this study enrolled a relatively small number of patients. Second, two patients who finished one-month follow-up were missed because they could not be contacted. Third, the use of GPI and thrombectomy was decided by the operators. While the latter might have affected lesion morphologies, care was taken to avoid excessive trauma. Fourth, the EROSION study predominantly enrolled young males with a high prevalence of smoking. Fifth, there was no functional evaluation at the time of repeat revascularisation. Sixth, the overlying thrombus might have reduced the accuracy of OCT to assess underlying plaque characteristics. To minimise this limitation, manual thrombus aspiration was performed to remove the thrombus before OCT imaging; patients with residual massive thrombus or an unclassified culprit lesion were excluded from the study. Finally, we do not have long-term OCT data in these patients to assess the degree of ongoing thrombus dissolution.
Conclusions
Four-year follow-up demonstrated that most patients with culprit lesion erosion treated with antithrombotic therapy without stenting in the EROSION study had favourable long-term clinical prognosis, with a cumulative TLR rate of 21%. Patients with poor response to antithrombotic therapy in the first month were more likely to require stent implantation during the next four years.
|
Impact on daily practice A mechanism-based strategy should be conducted for ACS patients. Effective antithrombotic therapy without stenting was promising for the majority of ACS patients with underlying plaque erosion. Patients with more effective thrombus dissolution during the first month were more likely to achieve good prognosis and be free from revascularisation at long-term follow-up. |
Funding
B. Yu has received research grants from the National Key R&D Program of China (2016YFC1301103) and the National Natural Science Foundation of China (81827806). H. Jia has received grants from the National Natural Science Foundation of China (81671763 and 81722025). S. Hu has received grants from the National Natural Science Foundation of China (81701804).
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.