
Left ventricular outflow tract (LVOT) obstruction occurs in 70% of patients with hypertrophic cardiomyopathy (HCM) and can be associated with disabling symptoms1. Current therapies for drug-refractory symptoms are surgical myectomy2 and alcohol septal ablation (ASA)3. Both procedures improve clinical symptoms and reduce outflow gradients. To take advantage of surgical myectomy and ASA and to avoid sternotomy and damage to the conduction system distributed underneath the endocardium, we proposed a novel procedure (named the Liwen procedure) whereby percutaneous intramyocardial septal radiofrequency ablation is used in the hypertrophic septum to reduce LVOT obstruction.
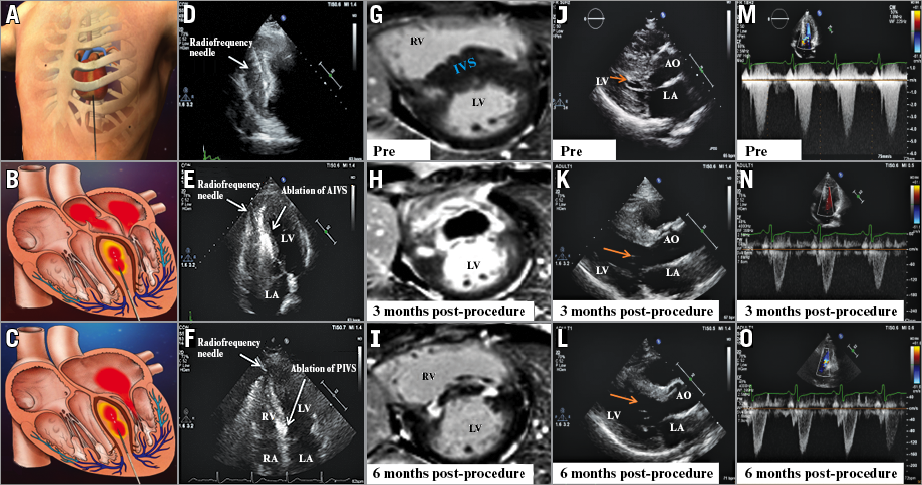
The Institutional Ethics Committee (KY20162042-1) of Xijing Hospital approved the procedure, which was performed in accordance with the ethical standards of the Declaration of Helsinki. This study was registered at clinicaltrials.gov (NCT02888132). Panels A-C illustrate the Liwen procedure. Under transthoracic echocardiography (TTE) guidance, the puncture site is positioned at the apex (Panel D). A guiding line is applied along the septal long axis and the radiofrequency ablation electrode needle (17G, Cool-tip™ RF Ablation System and Switching Controller; Medtronic, Minneapolis, MN, USA) pierced towards the hypertrophic anterior interventricular septum (AIVS) 8-10 mm from the subaortic valve (Panel E). Each ablation lasts for up to 12 min and the ablation power is gradually increased from 40 to 100 W. Then, the ablation needle is withdrawn 10 mm to prepare for the next application. Overall, 3-4 applications are performed in each patient. The ablation creates an area of thermal coagulative myocardial necrosis that appears as a hyperechogenic reflection detected by TTE. If deemed necessary, we repeat the procedure at the posterior interventricular septum (PIVS) (Panel F).
A 26-year-old HCM female patient underwent the Liwen procedure. The peak LVOT gradient at rest was 88 mmHg. Although she had taken β-blockers for several years, she had three episodes of syncope and progressive shortness of breath. Both anterior and posterior IVS were ablated 2-3 times with a maximum of 100 W. On cardiac magnetic resonance imaging, a low signal core was present in both anterior and posterior IVS with a thin enhancing rim representing inflamed tissue surrounding the ablated zone three months post procedure, and the zone of ablation showed ongoing fibrosis and shrinkage of the ablation-induced septal lesion six months post procedure (Panel G-Panel I). After six months, her symptoms were significantly relieved and she had no significant complications. With continuously improving LVOT obstruction (Panel J-Panel L), the peak LVOT gradient was reduced to approximately 10 mmHg (Panel M-Panel O).
Conflict of interest statement
The authors have no conflicts of interest to declare.

