Abstract
Aims: We present our first clinical experience to substitute ethanol with special designed microspheres in a TASH procedure (transcatheter ablation of septal hypertrophy). TASH is a standard approach for the treatment of patients with hypertrophic obstructive cardiomyopathy, severely symptomatic despite maximal medical therapy. However, the injection of alcohol remains a source of some possible complications.
Methods and results: We substituted alcohol with special designed microspheres. A highly symptomatic HOCM patient underwent a procedure of percutaneous ablation of his hypertrophied septum with the use of Embozene® microspheres. The procedure was successful, as the gradient was reduced from 70 before the procedure to 10 mmHg afterwards.
Conclusions: TASH by means of microspheres embolisation instead of alcohol was a safe and successful in the short-term procedure.
Introduction
Transcoronary ablation of septal hypertrophy (TASH)
Since 1995, alcohol septal ablation by selective ethanol injection into the target septal branch has been used as a therapeutic tool for hypertrophic obstructive cardiomyopathy (HOCM)1-3. Current clinical studies have demonstrated its therapeutic efficacy4,5, but there is an ongoing debate about the long-term impact of the resultant myocardial scar and comparison with surgical therapy of HOCM (surgical myectomy).
The principal idea of the procedure is inducing a septal infarction by catheter techniques, exactly at that position where the outflow tract is being obstructed by the hypertrophied septum. The acute damage causes the septum to lose its inward movement, where furthermore replacement by scar tissue, a usual process with all myocardial infarcts, causes even bigger shrinkage and hence obliteration of the left ventricle outflow gradient.
Microspheres
The technology of safe and reliable embolic agents to occlude the blood supply to tumours and certain arteriovenous malformations and to control bleeding has evolved during the past 35 years. From the mid-1970s, when physicians embolised microvessels with resorbable agents, to the mid-1980s when irregular polyvinyl alcohol (PVA) came into use. The shift to spherical particles led to the development of calibrated spherical embolisation devices for predictable vessel occlusion and easy, safe, and targeted delivery.
Nowadays, such spherical particles – so called microspheres – are used for the treatment of uterine fibroids, hepatocellular carcinoma, liver metastases, preoperative tumours, certain arteriovenous malformations, and for the management of bleeding5,6.
Embozene™ Color-Advanced Microspheres, developed by CeloNova BioSciences, Inc. (Newnan, GA, USA) are a specially designed spherical embolic material.
Briefly, Embozene™ Microspheres are built of a hydrogel core and coated with a special proprietary polymer, called Polyzene®-F, which offers biocompatibility. They come in various sizes, which range from 40-µm to 900-µm particles, while each size is coloured differently.
Materials and methods
Study design
This study was conducted to demonstrate the efficacy and safety of injecting Embozene Microspheres instead of ethanol inside the human coronary circulation, in an attempt to substitute alcohol with this agent in the TASH procedure.
Case history
The patient was a 45-year-old Caucasian male, smoker, who had started experiencing episodes of dyspnea on exertion, NYHA class III, as well as typical angina pectoris complaints, since a few months. On routine examination, including transthoracic echocardiography and coronary angiography/ ventriculography, a diagnosis of hypertrophic obstructive cardiomyopathy had been made, with a intraventricular septum measuring 26 mm. Invasively measured, the rest intraventricular gradient was 120 mmHg and the left ventricular function was high-normal with an EF of 80%. Furthermore, a mitral regurgitation grade III was obvious, attributable to the systolic anterior movement of the mitral valve, a characteristic finding in this disease.
Based on these findings the patient had been put on the highest affordable dose (120 mg once per day) of verapamil, with only little amelioration of his symptoms. For this reason, we decided to proceed with the percutaneous ablation of his hypertrophied septum. Instead of injecting alcohol we used the Embozene™ Microspheres. Their novel use in the heart was based on the assumption that they would offer a safer, however, equally effective alternative to the standardised alcohol procedure.
The patient provided written informed consent and the procedure was approved by the local ethics committee.
Results (Figure 1)
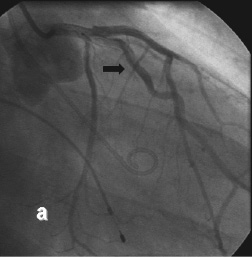
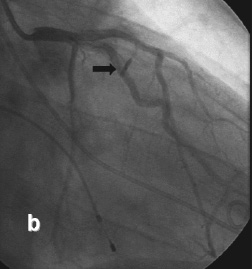

Figure 1. TASH procedure, with use of Embozene® Microspheres. a) Initial image with target septal perforator (black arrow), b) procedure with balloon inflated (black arrow) and c) final result, showing vessel stump (black arrow).
In our patient the TASH procedure was conducted using the following approach. After placement of a pacemaker wire in the RV apex and a pigtail catheter in the LV apex, the left coronary artery was selectively intubated with an EBU 3.5-6 Fr guiding catheter (Medtronic, Minneapolis, MN, USA). Initial measurement showed a intraventricular gradient of 70 mmHg (Figure 2) with post extra systolic augmentation.
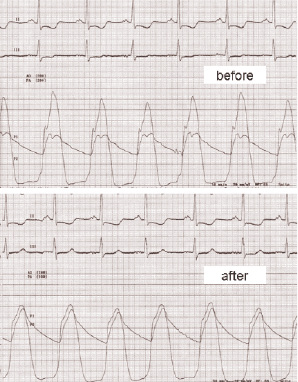
Figure 2. Left ventricular intracavitary gradient invasively measured, before and after the procedure with microspheres. Ao: aortic pressure; LV: pressure in left ventricle
The second septal perforator branch of the LAD was selectively wired by means of a Whisper LS hydrophilic wire (Abbott Vascular, Redwood City, CA, USA), and a 1,5/10 mm over-the-wire balloon was consequently advanced. After inflation of the balloon with 12 atm, echo contrast was injected through the balloon’s lumen to delineate the area to be infarcted and to exclude contrast deposition in remote myocardial regions such as the left ventricular posterior wall or papillary muscles. The optimal septal branch was identified by echo opacification of an area in the basal septum.
Following, 2.5 ml of microspheres measuring 100 µm in diameter were injected over the course of three minutes, and then the balloon was deflated and retracted.
At the end, the gradient was reduced from 70 to 10 mmHg (Figure 2), while the 1st septal branch could no longer be opacified. After 24 hours the pacemaker wire was removed.
The patient remained in the coronary care unit for four days, with a peak CK of 711 U/l and a peak CK-MB of 122 U/l, and was discharged from the hospital after seven days.
No allergic reactions were reported after the use of the microspheres. On ECG and transthoracic echo, no sign of necrosis of the LV anterior wall was noted, proving that the injection of microspheres did not cause embolisation in a territory other than the one intended.
Discussion
Percutaneous ablation of a septal branch by means of alcohol injection is considered nowadays an established method of permanently ablating the part of the septum that causes the left ventricle outflow obstruction. Immediate necrosis is followed by a further shrinkage due to the substitution of normal muscle tissue by scar tissue. This procedure carries the possible complication of alcohol being spilled out of the specifically targeted septal branch and causing a myocardial infarction to a territory far away from the one targeted. In this way, the left anterior descending artery could fill with alcohol with a consequent anterior wall infarction.
In the effort to make the procedure easier and safer, instead of alcohol we used specifically engineered microspheres, which theoretically would better match the dimensions of the target vessel. The avoidance of the direct toxic effect of alcohol on the myocardium made this concept even more appealing. Our initial attempt to cause a lasting haemodynamic improvement, accompanied by a clinical improvement, succeeded in our patient. The elevation in myocardial necrosis markers, namely CK and CK-MB, proved that we indeed caused myocardium necrosis, results comparing favourably to that of others7.
Conclusion
We report on our first clinical experience to test the hypothesis that a novel embolisation agent, namely Embozene® Microspheres, could be safely and effectively be used inside the human coronary circulation in a TASH procedure. In our case their use resulted in immediate improvement in the haemodynamics, without any adverse effects.

