Abstract
Hypertrophic obstructive cardiomyopathy (HOCM) is the most frequent genetic cardiovascular affection and is associated with high mortality and morbidity. Invasive treatment of symptomatic patients with HOCM refractory to drug therapy was limited to surgical myomectomy for years. In the mid 1990s, alcohol septal ablation (ASA) emerged as a new and less invasive option for septal ablation (SA) and is now considered a good alternative with excellent short- and long-term outcomes. Besides ASA, other techniques have been promoted to treat HOCM. The present review aims to summarise current practice and evidence of catheter-based techniques from the treatment of HOCM. We also detail technical points to achieve a safe and effective procedure.
Hypertrophic cardiomyopathy: a frequent disease, often obstructive!
About one third of patients with hypertrophic cardiomyopathy (HCM) develop left ventricular outflow tract (LVOT) obstruction (LVOTO) under resting conditions, defined as an instantaneous peak Doppler LVOT gradient of >30 mmHg at rest or during physiological provocation. A gradient of >50 mmHg is usually considered to be the threshold at which LVOT obstruction becomes haemodynamically significant1. LVOTO in HCM is usually the combination of basal septal hypertrophy and systolic anterior motion (SAM) of the mitral valve. LVOTO is associated with higher morbidity and mortality in patients with HCM. Pharmacological therapy using negative inotropic agents (mainly beta-blockers) is effective in the majority of patients. However, a significant proportion of patients experience drug-refractory symptoms or intolerance to treatment. Therefore, septal ablation (SA) should be considered in patients with an LVOTO gradient ≥50 mmHg, moderate-to-severe symptoms (NYHA functional Class III-IV), and/or recurrent exertional syncope in spite of maximally tolerated drug therapy.
The “old days” when surgery was the only option
In these patients, surgical treatment has been the gold standard for years, reducing LVOT gradients significantly in over 90% of cases, reducing SAM-related mitral regurgitation, and improving exercise capacity and symptoms. Long-term symptomatic benefit is achieved in 70-80% of patients, with a long-term survival comparable to that of the general population2. The main surgical complications are AV nodal block, ventricular septal defect and aortic regurgitation, but these are uncommon in experienced centres. Concomitant mitral valve surgery is required in about 15 to 20% of patients. Recently, Maron and Braunwald even encouraged the European cardiovascular community to reconsider surgical SA as a treatment option for severely symptomatic hypertrophic obstructive cardiomyopathy (HOCM) patients3. This was based on the fact that the less invasive alcohol septal ablation (ASA) has become more and more common practice in Europe.
Alcohol septal ablation: a new standard of care?
In 1994, an alternative technique of SA was proposed by Ulrich Sigwart4. The concept of ASA is to perform a chemical myomectomy of the basal interventricular septum by inducing a localised infarction with septal alcohol injection. The LVOT widens, and the basal septum does not move towards the MV in systole. This reduces not only SAM and LVOTO but also, by removing obstruction, the global left ventricular mass at follow-up5.
The “key” technical principles and the procedure step-by-step are described in Table 1 and Figure 1. In the vast majority of cases, the procedure is performed through the radial or femoral approach and identification of the septal(s) to be treated, as well as gradient measurements before and after ASA, are monitored by echocardiography. A temporary pacemaker (PM) should be inserted before the procedure, especially in patients with a high risk of post-ASA AV block. It should be systematic in patients with pre-existing left bundle branch block (LBBB). A guidewire is advanced to the presupposed septal branch. A short over-the-wire balloon is then advanced into the septal branch and inflated. The guidewire is removed and a small amount of angiographic contrast (0.5 ml) injected into the septal branch to ensure no spill back into the parent artery or collateral connection to other septal or major epicardial vessels. Myocardial contrast echocardiography is then used to demonstrate the area of myocardium supplied by the chosen vessel. Once the target artery has been satisfactorily identified, a small volume (1-3 ml) of absolute alcohol (95-96°) is injected slowly (usually 1 ml/min). The volume of alcohol injected will depend on the area of myocardium opacified with contrast injection. Balloon occlusion should be maintained for at least 3 to 5 minutes. A final angiographic image is taken to show the septal branch no-reflow and rule out any unwanted coronary artery damage. In case of failure (gradient reduction <50% and area of SA incomplete, a second septal or subseptal branch should be explored). The patient is kept under coronary care supervision for 24-72 hrs. Indication for definitive PM is decided at day two or three to allow intrinsic conduction to recover in case of acute AV block. Hospital stay is four to five days if no complication is observed. The 10 key technical “rules” for a safe and effective ASA are summarised in Table 1.
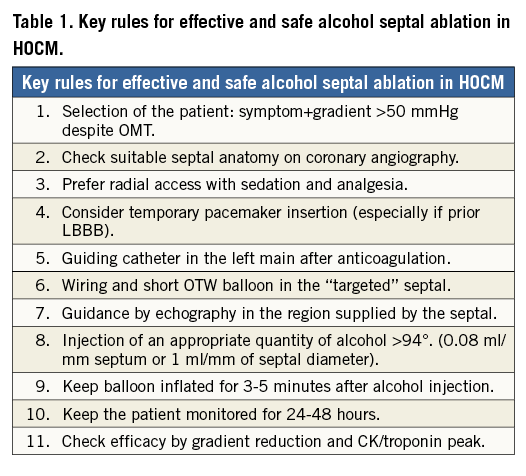
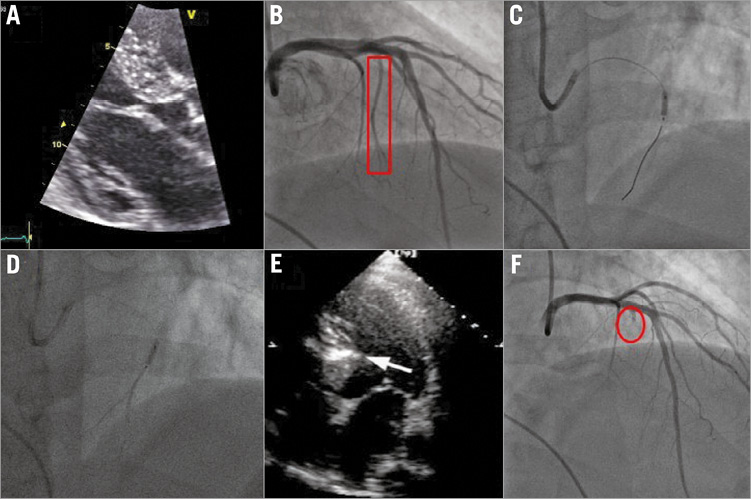
Figure 1. Step-by-step procedure of alcohol septal ablation for HOCM (A-F).
The most prominent complication associated with ASA is the need for a permanent PM occurring in about 10% of cases (<5% in patients with no pre-existing LBBB and 25-30% in case of pre-existing LBBB). Lower doses of alcohol and increased operator experience appear to reduce this risk. However, we must bear in mind that pacing can be an effective treatment to reduce LVOTO gradients and that patients with long-term pacing seem to have a similar outcome to those without pacing following ASA. Other severe periprocedural complications are rare (ventricular arrhythmia, LAD dissection). The fears regarding a pro-arrhythmic risk from the iatrogenic scar formed by ASA do not appear to have been substantiated, with most of the series showing no increased risk of sudden death. The long-term survival benefit of ASA, as with any other technique of SA including myomectomy, has not been demonstrated. However, HOCM patients with resting LVOTO have a higher mortality than matched HCM patients without a gradient, and recent case series have suggested that removing the gradient may have a beneficial effect on survival1. These data, although results from observational studies, will, however, go some way to reassuring operators that the iatrogenic scar of ASA does not increase mortality in the long term. These favourable results have recently been confirmed in the large European registry6.
Alcohol or surgery: an endless debate!
The new guidelines support SA (myectomy or ASA) in symptomatic patients with an LVOTO gradient >50 mmHg, provided that the septal reduction therapy is performed by experienced operators and teams1. Regarding the respective values of these two techniques, there are no randomised trials comparing surgery and ASA, but several meta-analyses have shown that both procedures improve functional status with similar procedural mortality. ASA is the preferred option in patients with mid ventricular obstruction and appropriate coronary anatomy. However, the less invasive version of the septal reduction therapy comes at a price: a higher risk of AV blocks requiring permanent pacemaker implantation. The new guidelines therefore state that septal myectomy, rather than alcohol septal ablation, is recommended in patients with other lesions requiring surgical intervention. It is also imperative that ASA procedure should be systematically echo-guided. Owing to limited patient populations, a randomised controlled study to compare mortality benefit between ASA and myomectomy will probably never be performed. Besides, other catheter-based techniques have been proposed for septal ablation1-3.
Alternative catheter-based techniques for septal ablation
SEPTAL ABLATION WITH ISCHAEMIA-RELATED DAMAGE TO MYOCARDIUM
Alternative methods of septal ablation have been explored, including injection of glue, microspheres, coil embolisation1 or covered stents7,8. In 2008, a French registry (using coils) was published with acceptable results and a low rate of complications9. In this study, 20 patients with HOCM underwent non-surgical myocardial septal reduction by coil embolisation and occlusion of the septal branch was successful in all cases (Figure 2). This study showed a significant reduction of gradient with very low complications, except for one ventricular septum defect. However, all of these methods damage myocardium by ischaemia. The rich collateralisation of the septum may challenge the possibility in effectively reducing long-term gradients by ischaemia alone. In the pilot study using coils, the gradient reduction was stable up to six months after the procedure9, but no long-term data are available.
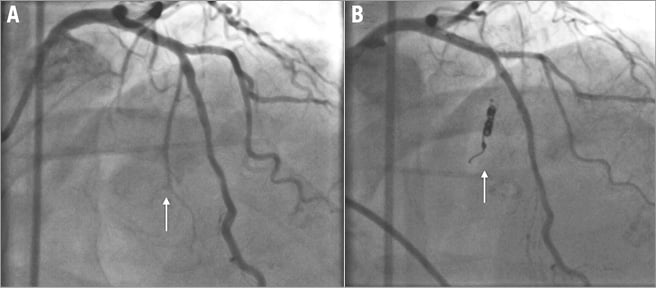
Figure 2. Septal ablation in HOCM by coil embolisation (A & B) (from Durand et al9).
ENDOCARDIAL RADIOFREQUENCY ABLATION OF SEPTAL HYPERTROPHY (ERASH)
Another approach by direct endocavitary ablation (radiofrequency, cryotherapy) has been proposed. Indeed, Lawrenz et al10 performed ERASH in a cohort of 19 adults, eight of whom had ineffective ASA due to inappropriate coronary anatomy. Although follow-up imaging showed a minor reduction in the magnitude of septal hypertrophy, deep scars were visible within the septum on cardiac MRI. This is in contrast to ASA, where a more marked change in the septal thickness in diastole is observed. Despite this, an important reduction in resting and provoked gradients was observed and NYHA status reduced significantly. The authors concluded that ERASH could be a new therapeutic option in the treatment of HOCM, allowing a significant and sustained reduction of the LVOTO as well as symptomatic improvement with acceptable safety. It may be suitable for patients not amenable to ASA or myectomy10.
These alternative methods have not been directly compared with other SA therapies and long-term outcome/safety data are not available. However, no one can deny that newer methods of non-surgical SA therapy may provide greater options for specific subsets of patients within the HOCM cohort. So far, these new techniques have been performed in small series of patients and larger studies are required before defining both the effectiveness and the safety of these new approaches.
Conclusion
In the 1960s, the only option for invasive management of coronary artery disease (CAD), aortic stenosis (AS) and HOCM was surgery. Over the years, developments in catheter-based techniques have extended to become an alternative and the default strategy in many cases. As with PCI for coronary artery disease and transcatheter aortic valve implantation for aortic stenosis in high-risk patients, catheter-based techniques have become the default strategy for the treatment of HOCM, with the most mature of these being the widely used and validated alcohol septal ablation.
Conflict of interest statement
The authors have no conflicts of interest to declare.