Abstract
Background: CT-QFR is a novel coronary computed tomography angiography (CTA)-based method for on-site evaluation of patients with suspected obstructive coronary artery disease (CAD).
Aims: We aimed to compare the diagnostic performance of CT-QFR with myocardial perfusion scintigraphy (MPS) and cardiovascular magnetic resonance (CMR) as second-line tests in patients with suspected obstructive CAD after coronary CTA.
Methods: A paired analysis of CT-QFR and MPS or CMR, with an invasive FFR-based classification as reference standard was carried out. Symptomatic patients with >50% diameter stenosis on coronary CTA were randomised to MPS or CMR and referred for invasive coronary angiography.
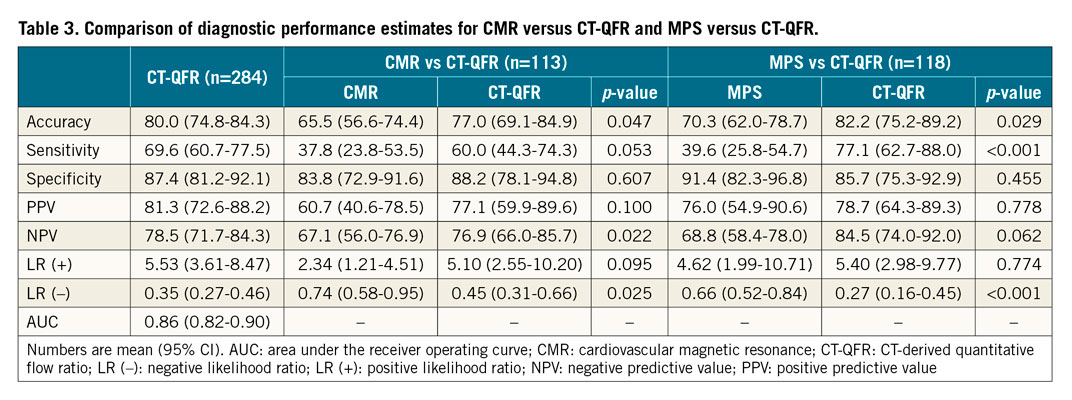
Results: The rate of coronary CTA not feasible for CT-QFR analysis was 17%. Paired patient-level data were available for 118 patients in the MPS group and 113 in the CMR group. Patient-level diagnostic accuracy was better for CT-QFR than for both MPS (82.2% [95% CI: 75.2-89.2] vs 70.3% [95% CI: 62.0-78.7], p=0.029) and CMR (77.0% [95% CI: 69.1-84.9] vs 65.5% [95% CI: 56.6-74.4], p=0.047). Following a positive coronary CTA and with the intention to diagnose, CT-QFR, CMR and MPS were equally suitable as rule-in and rule-out modalities.
Conclusions: The diagnostic performance of CT-QFR as a second-line test was at least similar to MPS and CMR for the evaluation of obstructive CAD in symptomatic patients presenting with ≥50% diameter stenosis on coronary CTA.
Introduction
Coronary computed tomography angiography (CTA) has a class I recommendation as a first-line test for diagnosis of obstructive coronary artery disease (CAD) in patients with low to intermediate pre-test risk1. Despite an excellent negative predictive value for ruling out obstructive CAD, coronary CTA’s positive predictive value remains unsatisfactory. A well-defined downstream diagnostic strategy for patients with suspected obstructive CAD on coronary CTA is currently lacking.
According to the NICE guidelines, CT-derived fractional flow reserve (FFRCT) may be considered in patients with stable chest pain following positive coronary CTA to ensure appropriate referral for invasive investigations2. Quantitative flow ratio (QFR) is an alternative method for fast computation of fractional flow reserve (FFR) from coronary images using three-dimensional coronary reconstruction and fluid dynamic equations3. A recent pilot study applied the QFR algorithm to coronary CTA (CT-QFR) with promising results4. However, CT-QFR has not been compared to perfusion imaging for second-line investigation following coronary CTA indicative of obstructive CAD.
The main aim of the current study was to compare the diagnostic performance of CT-QFR, myocardial perfusion scintigraphy (MPS) and perfusion cardiovascular magnetic resonance (CMR) as second-line tests after a coronary CTA showing at least one vessel with >50% diameter stenosis using an invasive FFR-based classification as reference standard.
Methods
STUDY POPULATION
The current work is a substudy of the previously reported Dan-NICAD study. The study design with patient flow and inclusion/exclusion criteria5, and the main results6 have been reported previously. In short, 1,675 patients with new-onset symptoms suggestive of CAD were referred for coronary CTA being the recommended first-line test in Denmark. Exclusion criteria included previous percutaneous coronary intervention (PCI)/coronary artery bypass grafting (CABG), contraindication for adenosine and reduced kidney function (eGFR <40 mL/min). Patients were referred for invasive coronary angiography (ICA) if coronary CTA was indicative of obstructive CAD (≥50% diameter stenosis [DS] in ≥1 coronary segment by visual estimation). Prior to ICA, patients were randomised to either MPS or CMR. Of the 1,675 patients referred for CTA, 391 (23.4%) had at least one coronary stenosis >50% DS by CTA. Of these, 301 (76.9%) completed either MPS or CMR and 362 (92.5%) were evaluated by ICA.
Patients with paired ICA and coronary CTA (n=358) were included in the present substudy. We applied substudy-specific exclusion criteria (Supplementary Appendix 1). The study complied with the Declaration of Helsinki and was approved by the local ethics committee. All patients provided informed written consent. The study was registered at ClinicalTrials.gov (Identifier: NCT02264717).
COMPUTED TOMOGRAPHY-DERIVED QUANTITATIVE FLOW RATIO
The CTA acquisition protocol was not optimised for subsequent CT-QFR analysis and has been described in detail previously5. Delineation of the coronary lumen was performed semi-automatically using a validated software package (QAngio CT Research Edition version 3.1; Medis Medical Imaging, Leiden, the Netherlands). Lumen contours were subsequently exported into a prototype software package (CtaPlus; Pulse Medical Imaging Technology, Shanghai, China). Details of the computation are provided in Supplementary Appendix 1. In short, all the coronary branches were merged into a hierarchical tree structure. Subsequently, the reference lumen was reconstructed assuming no stenosis. Patient-specific resting coronary flow was computed based on the size of the reference lumen and the allometric scaling law (Supplementary Figure 1). Finally, the CT-QFR value at each position of the coronary tree was computed based on a novel method that was adapted from the invasive angiography-based QFR algorithm, using the simulated hyperaemic flow modelled from the resting flow as boundary condition3. The coronary CTA segmentation was performed at a core laboratory (CardHemo; Med-X Research Institute, Shanghai Jiao Tong University, Shanghai, China) by experienced analysts, who were blinded to demographic, invasive FFR, and follow-up data. The observer variability at the core laboratory was reported previously4. After completing all CT-QFR analyses, the CT-QFR values were transferred to Aarhus University Hospital, Denmark, for statistical analysis. For CT-QFR, ≤0.80 was used as diagnostic cut-off. A fixed CT-QFR value of 0.50 was applied to suboccluded and occluded vessels.
MYOCARDIAL PERFUSION IMAGING AND INVASIVE CORONARY ANGIOGRAPHY
The MPS, CMR and ICA protocols are shown in Supplementary Appendix 1.
STATISTICAL ANALYSIS
Distribution of data was checked with Q-plots and the Shapiro-Wilk test. Continuous variables are presented as mean±SD, mean (95% CI) or median (IQR) as appropriate. Categorical variables are presented as count (%). Paired diagnostic accuracy, sensitivity and specificity estimates were compared with McNemar’s test. Positive predictive values, negative predictive values and likelihood ratios were compared using generalised score statistics. Diagnostic metrics for CT-QFR, MPS and CMR were recalculated using revascularisation as reference standard. Intention-to-diagnose analysis was performed by classifying non-evaluable and not-performed CT-QFR, MPS and CMR investigations as false-negatives and false-positives according to the ICA/FFR results. Patients and vessels were stratified into four groups based on diagnostic mismatch on a per-patient and per-vessel level. The Breusch-Pagan/Cook-Weisberg test was used to test for per-vessel heteroscedasticity between invasive FFR and CT-QFR. P-values <0.05 were considered significant.
Results
Of 358 patients with paired coronary CTA and ICA, CT-QFR was computed for all vessels in 284 (79%) patients. CT-QFR feasibility accounted for 17% of exclusions, mainly due to motion artefacts and image noise (Figure 1). Patients for whom CT-QFR was not feasible had a higher heart rate and higher Agatston calcium score compared to patients where CT-QFR was feasible (Supplementary Table 1). Complete paired data were available for 118 patients in the MPS group and in 113 patients in the CMR group (Figure 1). Baseline demographics and procedural characteristics are listed in Table 1 and Table 2. A total of 125 (44%) patients had obstructive CAD at ICA with invasive FFR. For vessels with paired assessment of CT-QFR and invasive FFR (n=239), median CT-QFR was 0.87 (IQR: 0.81-0.93) and median invasive FFR was 0.85 (IQR: 0.77-0.90) with 35% of FFR measurements being ≤0.80 (Supplementary Figure 2). The diagnostic performance of CT-QFR is described in Supplementary Appendix 2, Figure 2, Table 2, and Supplementary Table 2.
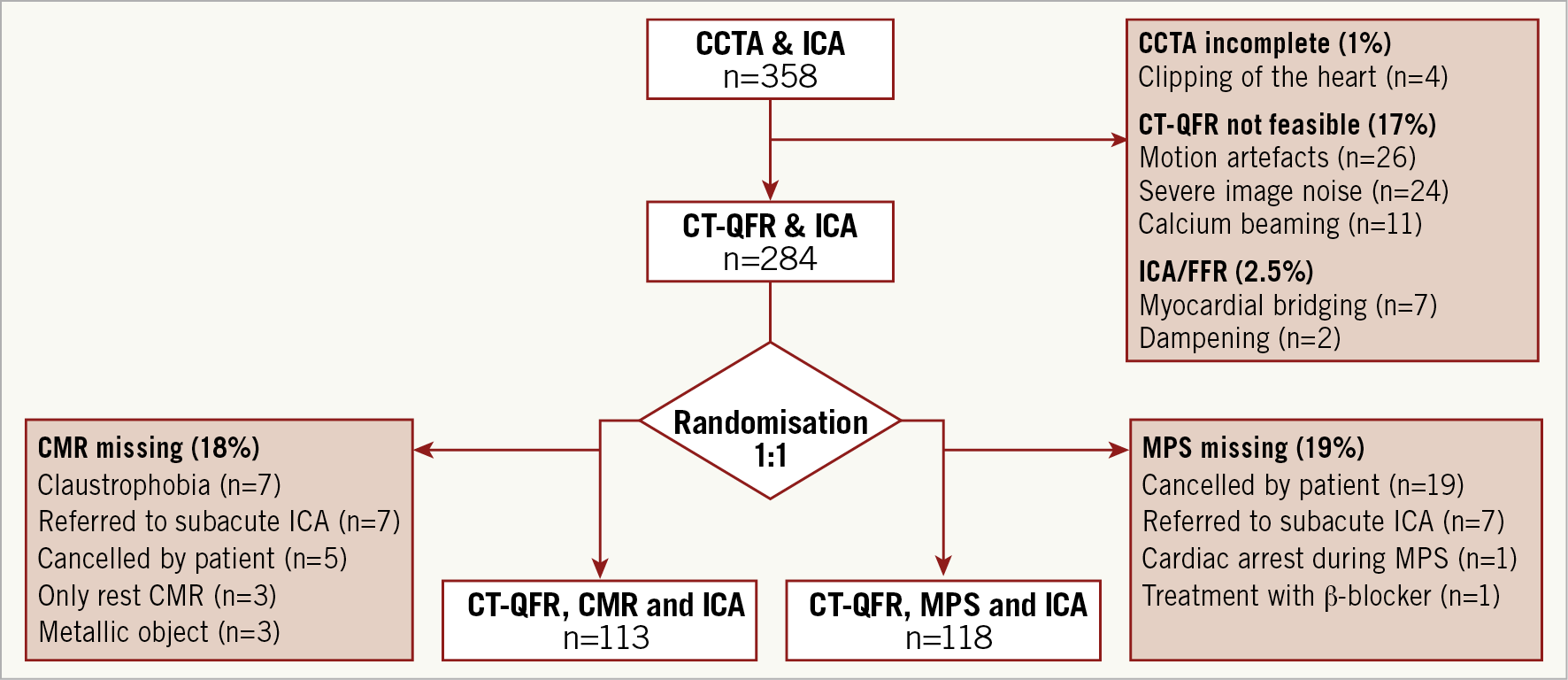
Figure 1. Study flow chart. CCTA: coronary computed tomography angiography; CMR: cardiovascular magnetic resonance; CT-QFR: CT-derived quantitative flow ratio; FFR: fractional flow reserve; ICA: invasive coronary angiography; MPS: myocardial perfusion scintigraphy
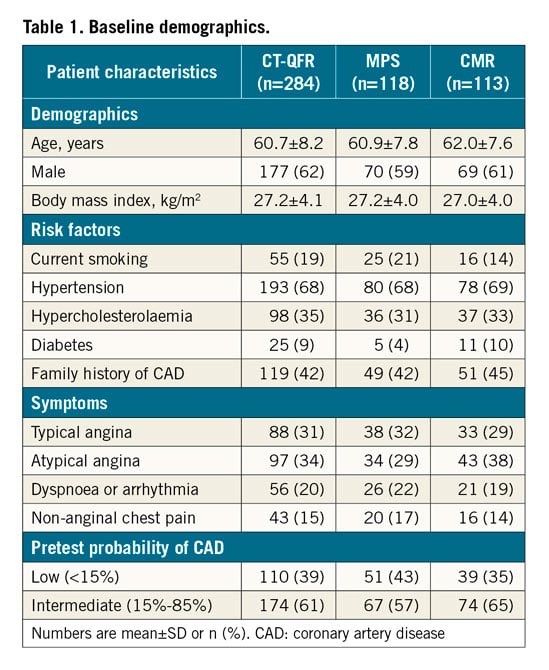
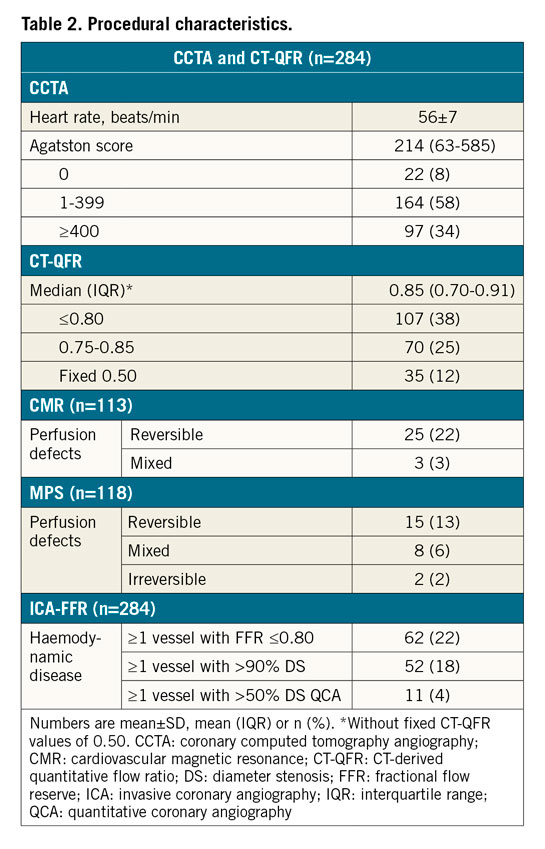
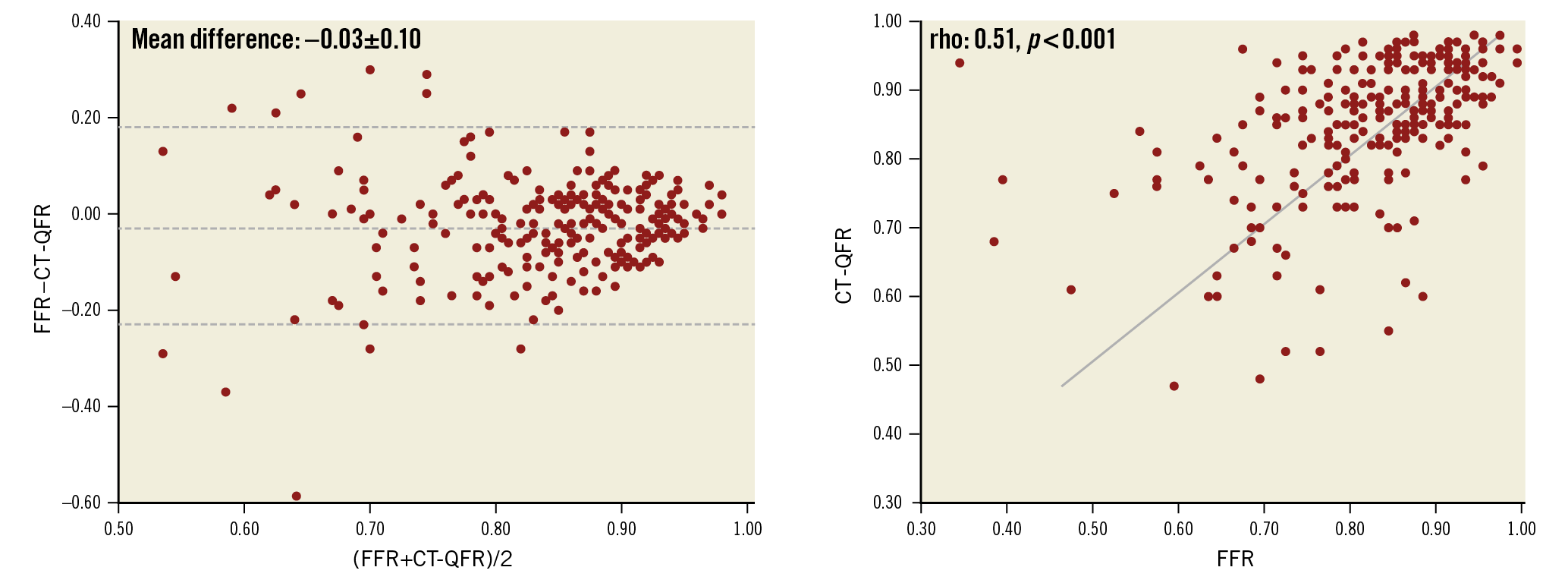
Figure 2. Lesion-level correlation and agreement of CT-QFR and FFR. CT-QFR: CT-derived quantitative flow ratio; FFR: fractional flow reserve
COMPARISON OF THE DIAGNOSTIC PERFORMANCE FOR CT-QFR, MPS AND CMR
A comparison of CT-QFR versus MPS and CT-QFR versus CMR on diagnostic performance estimates is presented in Table 3, with examples shown in Figure 3. While CT-QFR displayed better sensitivity and diagnostic accuracy, specificity was similar between the respective modalities. Based on the likelihood ratios presented in Table 3, CT-QFR, CMR and MPS were equally suitable to rule in CAD as defined by ICA and invasive FFR, while CT-QFR was more suitable as a rule-out modality. The same was true with the use of revascularisation as reference standard (Supplementary Table 3). The diagnostic performance estimates for MPS with abnormality defined as a summed stress score (SSS) >3 are presented in Supplementary Table 4. When compared to patients with reversible perfusion defects, patients with fixed or irreversible perfusion defects were more likely to have high-grade stenoses as identified by ICA, albeit not reaching statistical significance (46% vs 28%, p=0.18) (Supplementary Table 5).
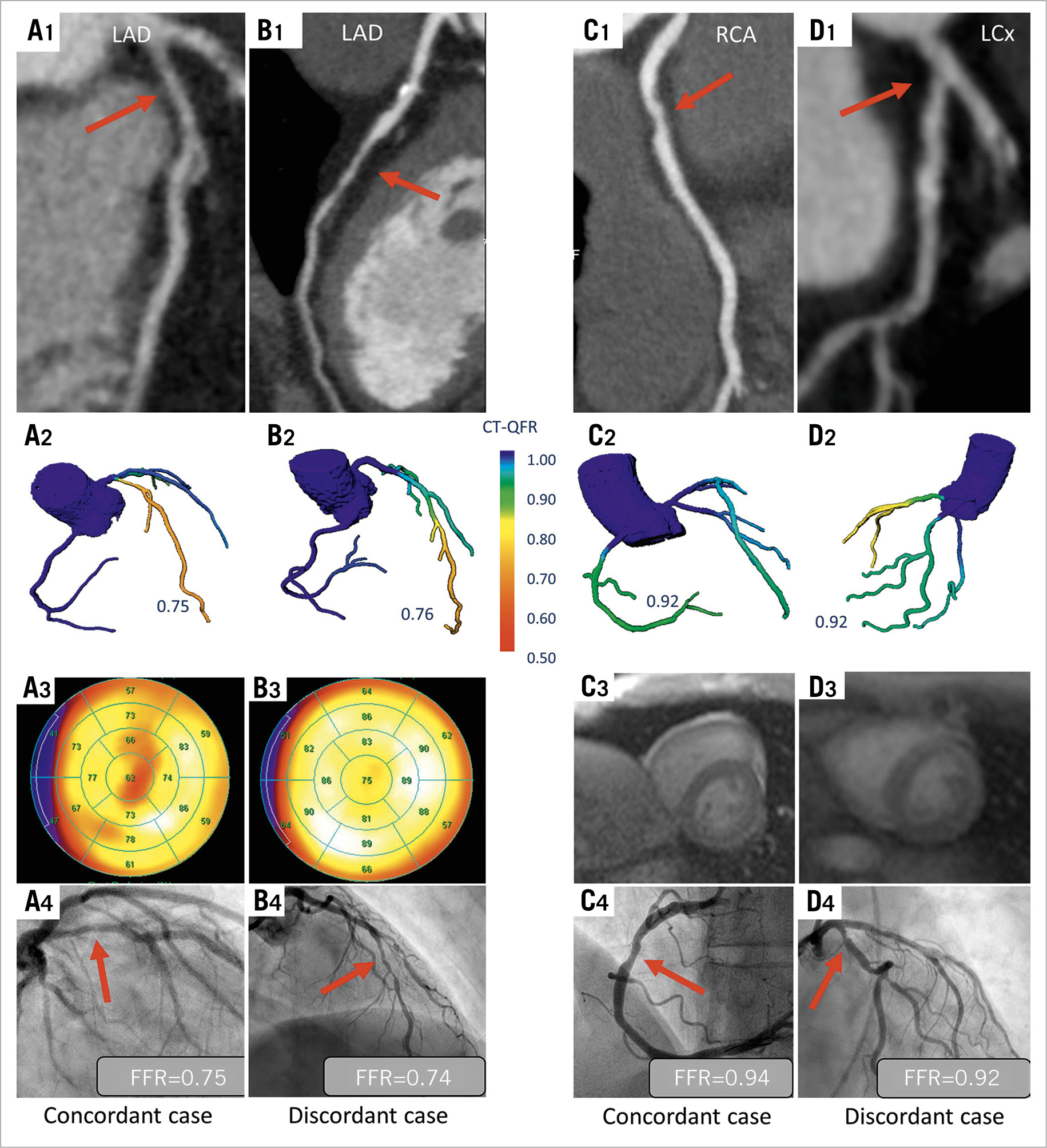
Figure 3. Illustrative examples of four study patients. A1-A4 indicate coronary CTA-identified intermediate stenosis on the LAD (A1) considered obstructive by CT-QFR (A2), MPS (A3) and invasive FFR (A4). B1-B4 indicate calcified and soft plaques on coronary CTA (B1) considered obstructive by CT-QFR (B2) and invasive FFR (B4) but not by MPS (B3). C1-C4 indicate coronary CTA-identified intermediate stenosis on the RCA (C1) not considered obstructive by CT-QFR (C2), CMR (C3) and invasive FFR (C4). D1-D4 indicate plaques on coronary CTA (D1) not considered obstructive by CT-QFR (D2) and invasive FFR (D4) but obstructive by CMR (D3). CT-QFR: CT-derived quantitative flow ratio; FFR: fractional flow reserve; ICA: invasive coronary angiography; LAD: left anterior descending artery; LCx: left circumflex artery; RCA: right coronary artery
COMPARISON OF THE DIAGNOSTIC PERFORMANCE FOR CT-QFR, MPS AND CMR WITH THE INTENTION TO DIAGNOSE
An intention-to-diagnose analysis using the full population with conclusive ICA results is presented in Supplementary Table 6 with 3*2 contingency tables and in Supplementary Table 7 with diagnostic performance estimates. Sensitivity remained better for CT-QFR when compared to MPS and CMR. Specificity was better for MPS when compared to CT-QFR and similar for CT-QFR when compared to CMR. CT-QFR, MPS and CMR remained equally suitable as rule-in and rule-out modalities (Supplementary Table 7).
Discussion
The main findings were that, following a coronary CTA with suspected obstructive CAD, 1) CT-QFR can be used to rule in and rule out the presence of obstructive epicardial CAD with at least similar efficiency to MPS and CMR, and 2) CT-QFR feasibility was hampered in patients with a high heart rate and high Agatston calcium score.
COMPARISON TO ALTERNATIVE CORONARY CTA-DERIVED FFR SOLUTIONS
Increasing emphasis is given to post-processing of coronary CTA data for derivation of FFR. The pioneer modality, FFRCT (HeartFlow, Redwood City, CA, USA), has good diagnostic accuracy with invasive FFR as reference standard and is able to differentiate high-risk and low-risk patients in terms of deferral or referral to further downstream testing7,8. Despite a numerically slightly poorer sensitivity of CT-QFR indicated by this study, the overall diagnostic accuracy of CT-QFR to predict revascularisation appears at least similar to that of FFRCT in a cohort identical to the present analysis (diagnostic accuracy 75.2% for CT-QFR [Supplementary Table 2] and 61% for FFRCT)9.
Comparing the presented diagnostic performance estimates to similar studies should be done with caution given the impact of differences in distribution of the target condition (e.g., FFR ≤0.80) and level of calcification that varies substantially8,10. The observed per-vessel numerical agreement between CT-QFR and invasive FFR was modest and comparable to other coronary CTA-derived FFR solutions with broad ranges of agreement11. The uncertainty related to the numerical agreement indicates that, even though CT-QFR and alternative coronary CTA-derived FFR solutions may improve the usual-care diagnostic pathway in patients with suspected obstructive CAD, the numerical value can currently not be used to plan subsequent revascularisation12.
FFRCT requires transfer of images to a centralised core laboratory. Importantly, a pilot study on CT-QFR using off-the-shelf computers showed that the average segmentation process took 17 minutes, while the subsequent CT-QFR computation on average took 19 seconds, thus illustrating the feasibility and potential for use of CT-QFR in same-day diagnostic work-ups4. The latter study found a better correlation and agreement of CT-QFR with FFR compared to our findings. This may be due to several factors. The diagnostic performance estimates may have been affected by retrospective selection of coronary CTA data in the pilot study, while the correlation and agreement may differ because the present study included more severe lesions (FFR <0.60) where the CT-QFR versus FFR scatter was larger.
COMPARISON TO CMR AND MPS
We found a sensitivity of MPS comparable to that reported in a previous study where MPS was tested as second-line modality13. Studies of CMR as a second-line test with invasive FFR endpoints are scarce. Studies testing CMR or MPS as first-line test with an FFR-based endpoint generally find sensitivities in the range of 57-90%14,15. The low sensitivity in the current report may be explained by the coronary CTA-based referral to MPS and CMR, because high-risk patients (e.g., suspicion of high coronary artery calcium score [CACS], high body mass index [BMI], kidney disease) are generally not referred to coronary CTA. This is backed by the findings of ReASSESS where symptomatic patients were referred to MPS based on 40-90% DS on coronary CTA and where MPS had a sensitivity of 41% (29-55) using an FFR-based reference standard13.
CT-QFR and invasive FFR are restricted to evaluation of epicardial vasculature, while CMR and MPS also include perfusion of the microvasculature. Hence, a good agreement between CT-QFR and invasive FFR was expected. Despite the fact that abnormal CMR/MPS investigations predominantly counted reversible and mixed perfusion defects (Table 2), our applied definition of abnormal CMR and MPS also included irreversible perfusion defects potentially indicative of infarcts. Irreversible perfusion defects would not be expected to correlate well with a pure FFR-based endpoint. However, the included population did not have any known coronary artery disease upon enrolment and, reflecting routine clinical practice, ICA would be indicated.
It cannot be ruled out that our inclusion of a proportion of patients with atypical symptoms influenced the diagnostic performance estimates, because the sensitivity of perfusion imaging as second-line test after coronary CTA is highest in patients with typical angina, probably due to a higher pre-test risk of obstructive CAD in these patients compared to, e.g., atypical, lower-risk patients16. We observed a similar pattern for CT-QFR as sensitivity and diagnostic performance were highest for patients with typical angina and lowest for patients with non-anginal chest pain (Supplementary Table 2, Supplementary Figure 3).
CHALLENGES IN DERIVING FFR FROM CORONARY CTA
The acquisition protocol for coronary CTA in the Dan-NICAD trial did not specify specific standards required for CT-QFR analysis. We found that 17% of the coronary CTA data in Dan-NICAD did not have the required quality for CT-QFR calculation. This is slightly higher compared to previous studies on CT-FFR reporting rejection rates around 12-13%. However, it is in line with FFRCT by HeartFlow when applied to the CMR population from the Dan-NICAD data set (rejection rate 21%)9. Coronary calcification was shown to be a particular challenge. Calcium score tended to be higher in patients with false-positive CT-QFR measurements compared to patients with true-negative CT-QFR measurements (Supplementary Table 3). This influence could be caused by challenges related to lumen segmentation in calcified vessels. We included patients prospectively before the knowledge of CTA findings and without specific criteria for CTA quality, which may explain the relatively large total calcium burden (mean total calcium score of 424±424 in the current study compared with, e.g., 302±468 in the Coronary Blood Flow Using CT Angiography: Next Steps [NXT] trial)8.
Discordant classification was, as expected, more frequent in the CT-QFR range of 0.75-0.85 (Supplementary Table 7). Some natural variance will be present close to the discrimination point for any test with a binary cut-off. Identification of a strict low (refer) and high (defer) CT-QFR limit may ensure a suitable second-line CT-QFR-based strategy following a positive coronary CTA and should be investigated in a prospective manner. Finally, our data indicate that CAD located in the LM and proximal LAD often occurs in vessels with false-negative CT-QFR measurements (Supplementary Table 7). This may reflect challenges of generalised computation algorithms to account for large increases in coronary blood flow, as expected in vessels supplying a large mass of myocardium. Given the prognostic importance of the left main coronary artery (LM) and proximal left anterior descending coronary artery (LAD) lesions, further refinement of the CT-QFR technique could be needed. Application of the QFR algorithm to ICA with the use of a Thrombolysis In Myocardial Infarction (TIMI) frame count yielded better diagnostic performance in previous studies and may therefore reflect a more patient-tailored solution than when using generic flow assumptions such as those in the current report3.
Limitations
The current Dan-NICAD substudy did not include a specific power calculation for the current aim. Consequently, the study should be considered exploratory and the findings hypothesis-generating. Secondly, the low sensitivity of MPS and CMR may be explained by our applied criteria for abnormal perfusion resulting in many false negatives. However, recalculation of perfusion defects with less stringent criteria provided similar diagnostic performance estimates as illustrated with MPS (Supplementary Table 3). Thirdly, referral of patients to ICA based on a coronary CTA with suspected obstructive CAD may have biased the analysis in favour of CT-QFR. However, coronary CTA is the recommended first-line test and, given the high negative predictive value, it would not be clinically feasible to refer all patients for ICA. Lastly, a substantial number of coronary CTA scans did not meet the criteria for CT-QFR analysis, which may have biased the primary paired CT-FFR versus MPS and CT-QFR versus CMR analyses. Furthermore, CT-QFR was not attempted in vessels with myocardial bridging. However, the intention-to-diagnose analysis likewise revealed that CT-QFR was able to rule in and rule out the presence of obstructive CAD to the same degree as MPS and CMR. Importantly, insufficient coronary CTA quality for CT-QFR analysis can swiftly be identified because the technique does not require transfer of images to a centralised laboratory. The true feasibility rate and time to CT-QFR should be assessed in prospective studies with coronary CTA protocols optimised for post-processing activities.
Conclusions
The diagnostic performance of CT-QFR was at least similar to MPS and CMR for the evaluation of obstructive coronary artery disease in symptomatic patients presenting with ≥50% diameter stenosis on coronary CTA.
|
Impact on daily practice The present study found that CT-QFR has a diagnostic performance comparable to MPS and CMR when used as second-line test after coronary CTA with suspected obstructive CAD but with room for improvement in feasibility. Pending confirmation in prospective studies, CT-QFR bears the potential to reduce unnecessary downstream diagnostic procedures and ensure a more appropriate referral of patients for invasive coronary angiography with the aim of identifying obstructive coronary artery disease. |
Acknowledgements
S. Tu would like to acknowledge support from the Natural Science Foundation of China (Grant No. 81871460), the Shanghai Municipal Science and Technology Commission (Grant No. 19441913600), and the Program of Shanghai Technology Research Leader. J. Westra acknowledges support from Aarhus University (PhD scholarship). S. Petersen acknowledges support from the National Institute for Health Research Barts Biomedical Research Centre.
Conflict of interest statement
S. Petersen reports personal fees from and is a shareholder of Circle Cardiovascular Imaging, Calgary, Alberta, Canada. There were no direct fees related to this research project. S. Tu reports grants from Pulse Medical Imaging Technology, and Medis Medical Imaging, during the conduct of the study. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.