Atrial fibrillation (AF) poses a significant burden to healthcare systems, physicians and patients, due to its high prevalence (affecting at least 3% of adults worldwide); increased risk of major adverse events, including stroke and systemic embolism; heart failure; hospitalisation; impaired quality of life and mortality; and comprehensive multidomain treatment requirements that are often challenging for both the patient and the responsible physician1.
Most patients with AF are clinically complex, i.e., elderly and multimorbid. Indeed, AF shares many common risk factors and often coexists with numerous comorbidities, including, for example, heart failure or coronary artery disease1. Multidirectional interactions among any underlying comorbidities, coexistent cardiovascular risk factors and AF all profoundly affect overall cardiovascular wellbeing and atrial substrate (i.e., atrial cardiomyopathy), thus increasing the risk of AF-related major adverse events. Discerning the exact role of AF in such a milieu may sometimes be challenging, as AF could be the main driver of adverse events or just a bystander (i.e., a consequence of multiple pathological processes)2.
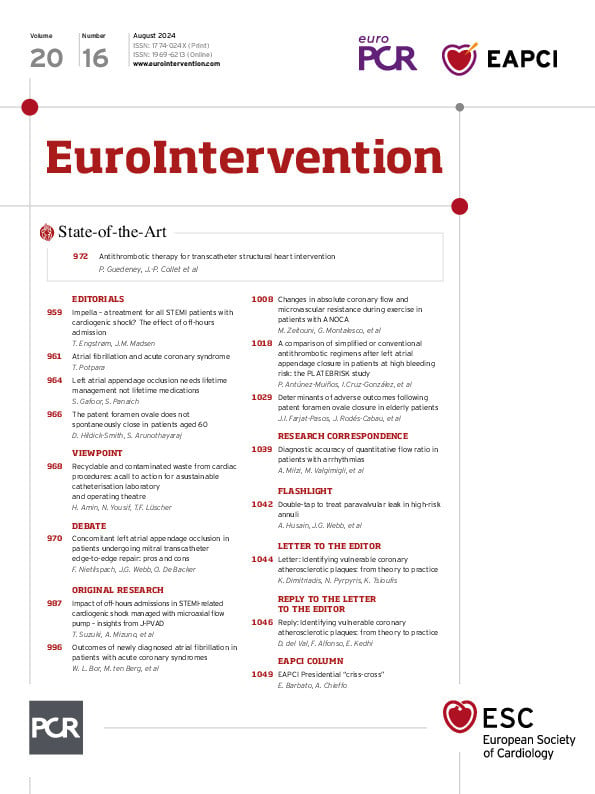
In this issue of EuroIntervention, Bor and colleagues report their observations on the incidence and characteristics of newly diagnosed AF in patients with acute coronary syndromes (ACS) and explore its association with 1-year major adverse events (a composite of all-cause mortality, myocardial infarction [MI] and ischaemic stroke) in a registry-based cohort of nearly 4,500 patients with ACS3. It is of great clinical relevance, since both AF and MI contribute significantly to the global burden of cardiovascular disease, and the bidirectional relationship between AF and MI has important treatment and prognostic implications.
Notwithstanding the major limitations inherent to all observational studies and a relatively small sample size, the present study3 broadly confirms previous findings that AF and MI often coexist (AF occurs in up to 21% of patients with MI, and MI is observed in up to 63% of patients with AF), and patients with both conditions have worse prognosis than those with either AF or MI only45. However, the relevance of the temporal relationship of the disease onset (i.e., whether MI occurred before AF, simultaneously with AF, or after AF is diagnosed) remains controversial, likely because of a selection bias. While observations from MI cohorts mostly found new-onset AF to be associated with worse prognosis3 and studies based on AF cohorts mostly reported MI occurring after AF as the least favourable setting4, a study of an unselected cohort reported no significant temporal relationship, with comparable prognostic implications of coexistent AF and MI, whichever came first5.
Bor and colleagues reported that a longer duration of new-onset AF (>24 h, observed in 44% of patients with new-onset AF in the study cohort) was associated with a significant 2-fold greater risk of major adverse events and all-cause mortality as well as a trend towards a greater risk of ischaemic stroke, compared with shorter AF episodes3. Notwithstanding the inadequacy of the method for adjudicating the duration of AF in their study (manual review of available electrocardiogram [ECG] tracings), this observation broadly confirms the generally well-documented gradual risk increase with increasing AF duration. Importantly, the duration of the ECG-documented AF episode (so-called clinical AF) must not guide the AF treatment decision regarding the use of oral anticoagulant (OAC) therapy for stroke prevention, which is primarily based on the individual patient’s risk of stroke1. Indeed, the strikingly suboptimal, guideline-non-adherent OAC prescription rate in patients with new-onset AF in the present study (slightly above 50% of patients, apparently irrespective of the individual patient’s stroke risk and more influenced by the AF duration)3 is rather worrisome, given that the risk of AF-related complications is especially increased early after new-onset AF1. Overall, the suboptimal OAC use is perhaps the most important finding in the present study, highlighting the urgent need for improving the management of patients with AF and ACS. A holistic, integrated management of patients with AF, as summarised in the guideline-recommended “Atrial fibrillation Better Care” (ABC) pathway (A – avoid stroke using OACs with periodic regular stroke and bleeding risk reassessment, B – better symptom control using rate and rhythm control, and C – comorbidity and risk factor identification and management)1, has been shown to be associated with significant reductions in all-cause mortality, stroke and other adverse events compared with usual care in all AF patients including those with concomitant AF and ACS6.
Conflict of interest statement
The author has no conflicts of interest to declare.